Questions about UW Pharmacology?
Here are a couple of our most popular questions about studying Pharmacology at UW.
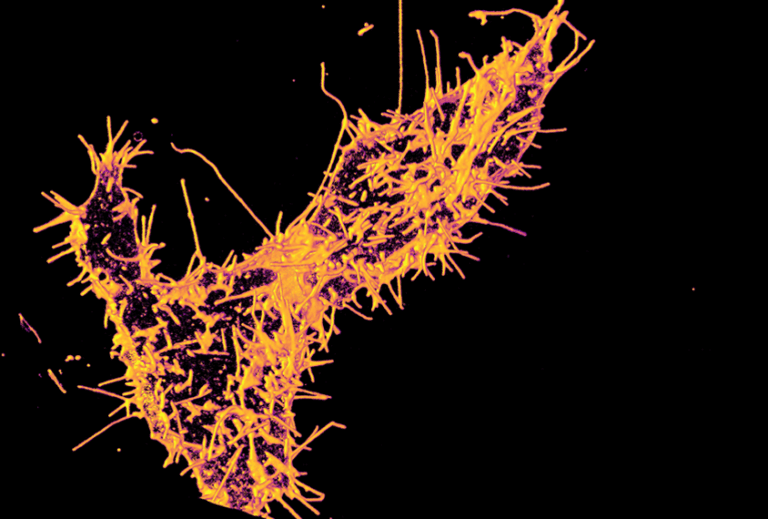
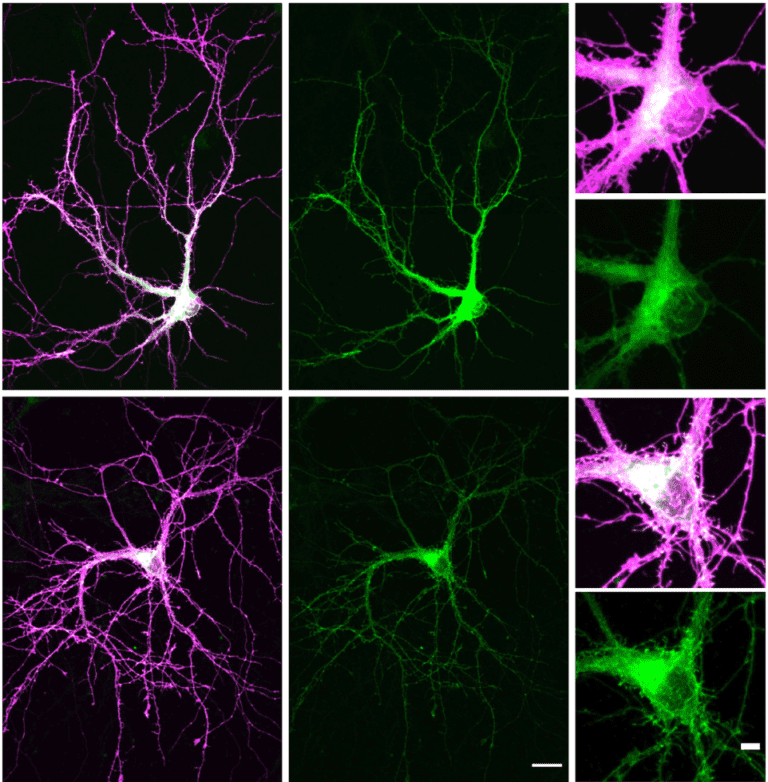
Read all about what we're doing in the department







Here are a couple of our most popular questions about studying Pharmacology at UW.
GRE Scores are not required to apply to our graduate program.
We consider top applicants who have prior research experience that can add to the diversity of our program. If you wish to apply, visit our admissions section for more information. To get started on your application, apply to the Graduate School on-line at https://www.grad.washington.edu/applForAdmiss/
Please visit the UW Graduate School website for information on who qualifies for fee waivers, how to apply and FAQ’s at https://www.grad.washington.edu/admission/application-fee-waivers/
The current time to earning the PhD is 5.5 years. This of course depends on your field of study, and how long it takes to complete your dissertation. For a year by year breakdown of the degree requirements please visit this page.
If interested in a postoctoral fellowship, we encourage you to contact the faculty member you wish to study with, directly. Please go to our people page and click on primary faculty. To learn more about their research, browse the Research section.

YOUR PHARMACOLOGY ADVENTURE STARTS NOW
A degree from the University of Washington in Pharmacology can open up career opportunities in academics, industry, policy, and venture investing.
ADMISSIONS