| Clinical Leadership | ||||||||
|
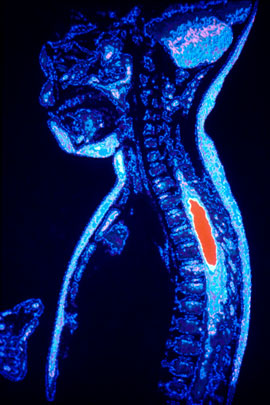
Seeing to the Core of the Problem |
||||||||
|
A person suffering a stroke has just three hours to reach the hospital for treatment to prevent long-term damage to the brain. However, ischemic strokes can affect mental acuity and mobility without causing pain. When this happens, people may not realize they're having a stroke until it's too late and their brain tissue has begun to die. Only four percent of stroke victims reach the hospital within that critical three-hour window.
"A stroke is analogous to a clogged drain," explained Beauchamp. "A blocked carotid artery is similar to a blocked pipe. If there's no delay, the clog can usually be fixed, but, if there's a long wait, the pipes on either side of the clog will be damaged. By helping physicians assess the situation, magnetic resonance imaging can show if surgery or inserting a stent would be advantageous to a patient or if another type of intervention would be more appropriate." Advances such at this in medical imaging have put radiology at the core of patient care. Beauchamp observed, "Radiology impacts almost every patient who comes into the hospital. " Among the emerging areas in radiology research is molecular imaging. By revealing fundamental structures and biological activity, molecular imaging can help evaluate physiology and morphology, as well as help map physiologic functions onto anatomic maps. "When genome scientists match genes to phenotypes (what an inherited trait or condition looks like physically on the outside), radiologist can help evaluate what's going on physiologically on the inside," said Beauchamp. "This is relevant in clinical trials both for participant selection and outcome measurements. Molecular imaging may also be used in measuring neuroplasticity (the ability of nerves or nervous tissue to grow or heal) and tracking stem cell therapy. It will play a key role in radiology, surgery, neurosciences, and vascular biology." Beauchamp joined the UW faculty in 2003 from his position as the interim radiology department chair at Johns Hopkins University in Baltimore. He hopes to lead the UW radiology programs into an era of innovations that foster patient comfort and treatment efficiency. "In the 1970s, physicians were asked to help deliver care in a cost-effective manner," said Beauchamp. "The fallacy was often a blanket limitation on the use of imaging services. Imaging today actually presents an invaluable tool for increasing therapeutic efficacy and decreasing the need for invasive procedures." Beauchamp is interested in optimizing imaging to benefit patient care. He'd like to do so cost-effectively by assessing screening programs and treatment outcomes. "Managing by gestalt is no longer an option," said Beauchamp. "Quantitative methodology needs to be inherent in how we manage our operations. This includes using statistical analysis to improve the efficiency of how we deliver care." Beauchamp predicts the UW Department of Radiology of the future will generate and process image data as a shared resource for UW Medicine, and eventually for other institutions in the WWAMI (Washington, Wyoming, Alaska, Montana, and Idaho) region. "Phase One is to enhance multidisciplinary programs in molecular imaging, nuclear medicine, magnetic resonance imaging, as well as establishing a brain center for peer-to-peer collaborations and a multidisciplinary imaging lab," said Beauchamp. "Phase Two is to create a Center for Imaging Sciences that would house these core programs and make them available to investigators at the UW and across the five states served by the UW medical school." Development Note
Over the past two years, private support has grown for the Department of Radiology's programs in molecular imaging and cancer detection. Many contributors are on the UW medical faculty. Among them are Dr. Soo Borson, professor of psychiatry and behavioral sciences; Dr. Alexander M. Spence, professor of neurology, pathology, and neurological surgery; and Dr. Kenneth A. Krohn, professor of radiology. They gave through the UW payroll deduction plan, which allows faculty and staff members to contribute regularly to the patient care, medical education, or research fund of their choice. |
||||||||
|
© 2003 - 2004 UW Medicine
Maintained by UW Health Sciences and Medical Affairs News and Community Relations Send questions and comments to drrpt@u.washington.edu |
||||||||