Core Components and Multimodal Strategies
In this introductory module you will learn the essential components of effective Infection Prevention and Control (IPC) programmes at the national and facility level, according to the scientific evidence and WHO’s and international experts’ advice. Using the WHO Core Components as a roadmap, you will see how effective IPC programmes can prevent harm from health care-associated infections (HAI) and antimicrobial resistance (AMR) at the point of care. This module will introduce you to the multimodal strategy for IPC implementation, and define how this strategy works to create systemic and cultural changes that improve IPC practices. This foundational knowledge will guide you in effective development, and implementation of IPC programmes and IPC education in your facility.
Learning Objectives
By the end of this module, you will be able to:
- Describe how the WHO Core Components relate to the implementation of a successful IPC programme.
- Describe multimodal strategies that can be applied to improve IPC activities.
Learning Activities
-
IPC Leadership and the WHO Core Components (10 min)
WHO created the Core Components of Infection Prevention and Control (IPC) Programmes to support countries as they develop their own IPC guidelines and plans.
Watch this video to learn more about why the Core Components are so integral to a successful IPC programme. Discover how your role in IPC can help save lives.
-
WHO Core Components (20 min)
The WHO Core Components are a roadmap for how IPC can effectively prevent harm due to HAI and AMR. We will use this graphic to describe how each component is interconnected in support of successful IPC implementation.
Click or tap each area on this graphic to see how each component creates a structure for an ideal IPC programme.
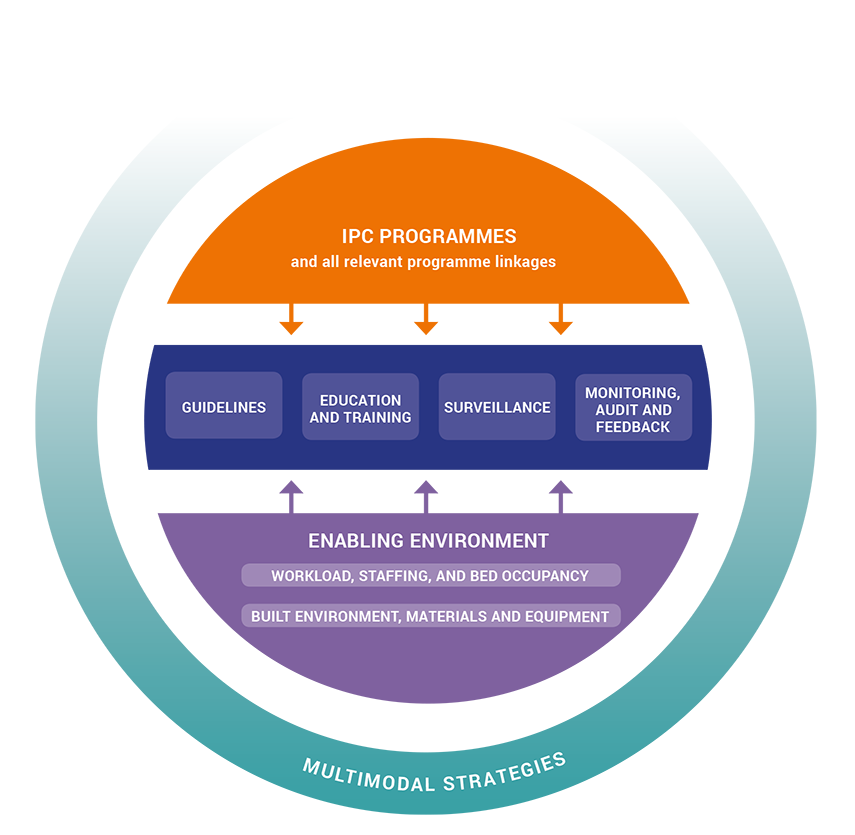
IPC Programmes
The purpose of an IPC programme is to prevent HAI and combat AMR. Health care facilities should have a dedicated and trained team of IPC professionals. IPC programmes are defined at the national level with clear objectives, functions, and activities. These policies will inform IPC programmes at the facility level. A well-functioning programme with a clear overall vision outlines what, where, how, and when each Core Component is supported, interacts, and progresses. National IPC programmes should be linked to other relevant national programmes and professional organizations for maximum efficiency. There should be specific resources dedicated towards IPC programmes.
Evidence-Based Guidelines
Key IPC principles to guide best practices should be described in evidence-based guidelines which are developed and implemented for the purpose of reducing HAI and AMR. For maximum uptake and correct implementation HCWs should be trained on IPC guideline recommendations. Processes must be in place to ensure that HCWs in your facility are educated and understand these guideline recommendations. Adherence with these guidelines should be monitored by the IPC focal person in conjunction with hospital management.
Education and Training
A successful IPC programme implements education and training for HCWs. At the facility level, it is best for participants to have hands-on experiences in best practices to reduce the risk of HAI and AMR. This is important for participants at all levels of education; individuals at pre-graduate, post-graduate, and in-service levels must be supported in IPC education and training. At a national level, it is beneficial for IPC programmes to collaborate with local academic institutions to ensure that training standards are being met. To increase improvements, the impact and effectiveness of training should also be evaluated.
Surveillance
At the facility level, HAI and AMR surveillance is conducted to guide IPC interventions and outbreak detection. Timely feedback of the results to HCWs in health care facilities and stakeholders at the national level will increase the likelihood that improvements will be made. This information can be used to evaluate the local situation with regards to HAI and compare facility data with national and other facilities data, which in turn can provide justification for allocating more resources to facilities that need them.
Monitoring, Audit, and Feedback
As with surveillance of HAI and AMR, monitoring and auditing IPC infrastructure, knowledge, and practices at an individual level can tremendously contribute to improving IPC interventions. Timely feedback should be provided to all relevant audited health care staff to increase adherence to best practices. A national IPC evaluation programme should assess to what degree national standards are being met in the activities performed. This criteria should be based upon the goals and objectives of the programme. Hand hygiene monitoring with feedback should be considered to be a key performance indicator at the national level.
Enabling Environment
Workload, Staffing, and Bed Occupancy
Addressing bed occupancy and staffing factors will significantly reduce the cross-transmission risk and ultimately reduce HAIs and the spread of AMR in health care. Bed occupancy should not exceed the standard capacity of the facility, and health care staffing should be at acceptable levels in relation to patient workload. Attention paid to these factors improves the quality of care your staff will be able to provide.
Built Environment, Materials, and Equipment
All patient care activities should take place in a clean, hygienic environment. Your facility should implement actions that support this environment. This includes the adequate availability of WASH infrastructure and services and IPC materials and equipment at the point of care (in particular hand hygiene facilities). When possible, centralized production and distribution of these supplies can be an effective approach. An example of this could be distribution of alcohol-based hand rub and soap by a national pharmacy.
water, sanitation, and hygieneMultimodal Strategies
Multimodal Strategies
At both national and facility levels, multimodal strategies represent the best approach to successfully implement IPC improvement efforts. A multimodal strategy consists of several elements implemented in an integrated way with the aim of improving an outcome and changing behaviour. The WHO multimodal improvement strategy addresses the areas of system change, training and education, monitoring and feedback, reminders and communications, as well as cultural change supporting IPC in a patient safety perspective. We will continually refer to this multimodal strategy throughout this course.
You can download a PDF of the WHO Multimodal Strategy in the Resources page of this course.
As the IPC focal person, it’s important to embrace the variety of technical, non-technical, clinical, social, human, managerial, and advocating skills to provide comprehensive and sustained support to the implementation of the Core Components. By doing this, patients have a better chance of a harm free experience in your facility.
Refer to the Resources activity in this module to download a PDF of the Core Components guidelines.
-
Core Components (10 min)
-
Multimodal Strategies (10 min)
Previously, we discussed how the multimodal strategy component plays an integral role in implementing a successful IPC programme. As the IPC focal person, you must be able to clearly articulate how the multimodal strategy applies to all IPC activities. Review the five elements of the strategy by clicking or tapping the green arrows or gray circles. In the next activity we will apply this strategy to a real life scenario.
Refer to the Resources page in this course to download the WHO Multimodal Improvement Strategy.
-
Multimodal Strategies in Real Life (10 min)
Last year, Joan noticed that safe sharps disposal was a problem at her facility. In the hope of resolving the issue to keep staff and patients safe, she has decided to launch a training programme on safe disposal of used needles.
Over the last few months, each staff member has participated in a training workshop.
To ensure that everyone is aware of these procedures, posters are placed on the walls. Joan has asked the hospital management to support the IPC team to conduct regular audits of safe sharps disposal.
Lately, however, Joan has noticed that there has been little to no change in behaviour—people are still not safely disposing sharps. One reason for this may be because sharp containers/safety boxes are not being regularly provided at the point of care. Other reasons could be because supplies regularly run out, and there hasn’t been a coordinated effort to regularly review audit results.
-
Summary (5 min)
In this module, you’ve learned that the WHO Core Components are essential to the implementation of a successful IPC programme. Each of these components work together to develop, support, and measure the efficient prevention of HAI and the reduction of AMR. As the IPC focal person, you will be expected to wear many different hats. These components support the technical, non-technical, clinical, social, human, managerial, and advocating skills required to create and maintain a functioning IPC programme that supports patients and HCWs.
In addition, remember that the multimodal strategy supports the rest of the components as a tool to integrate IPC activities in your facility. The aim is to improve patient outcomes and change health care worker behaviour. The five elements of the multimodal strategy are Build it (system change), Teach It (training and education), Check It (monitoring and feedback), Sell It (reminders and communications), and Live It (culture change). Be sure that you integrate these five elements to create strong, long lasting IPC programmes at your facility.
-
References
- 1WHO (2016) Guidelines on Core Components of Infection Prevention and Control Programmes at the National and Acute Health Care Facility Level.
- 2Storr J, Kilpatrick C, Allegranzi B, Syed S (2016) Redefining infection prevention and control in the new era of quality universal health coverage. Journal of Research in Nursing, Vol. 21(1) 39–52





