Environmental Cleaning and Disinfection
The healthcare environment contains a diverse population of microorganisms and can be a reservoir for potential pathogens. If environmental cleaning is not performed correctly, then environmental contamination can contribute to the spread of multidrug-resistant organisms and healthcare-associated infections. Collaboration between infection prevention and control (IPC) and environmental services (EVS) staff limits the role of the healthcare environment in disease transmission. In this module, you will learn the role of an IPC professional in environmental cleaning and understand how cleaning and disinfection prevents contamination of the healthcare environment.
Learning Objectives
By the end of this module, you will be able to:
- Describe areas of collaboration between IPC and environmental services
- Describe the healthcare environment and purpose of environmental cleaning
- Identify differences between routine and terminal cleaning
- Describe standard precautions to keep environmental services workers safe
- Understand the function of cleaning agents and disinfectants
- Describe uses of environmental monitoring in the healthcare setting
Learning Activities
-
IPC and Environmental Services (10 min)
Infection prevention and control (IPC) works with environmental services (EVS) to limit the role of the healthcare environment in disease transmission. Collaboration between EVS and IPC is essential to make sure cleaning standards are met. As an IPC focal point, you have responsibility to make sure IPC is integrated in the daily work of EVS staff.
Though many facilities have dedicated cleaners, some also rely on nursing staff to clean clinical areas. Some facilities directly hire cleaners, and others use an external contractor. Supervision of cleaning varies; an EVS manager ideally covers this role, but facilities often report that the nurse in-charge, IPC focal point, or facility management oversee cleaning activities. IPC should be closely linked to EVS activities regardless of what department oversees cleaning activities.
The IPC focal point or committee should review and approve EVS procedures. The IPC focal point helps standardize EVS procedures to ensure IPC is part of the daily work of cleaners. Examples of EVS procedures include:
- Routine cleaning of patient rooms
- Terminal cleaning of patient rooms
- Cleaning of common areas (waiting rooms and lobbies)
- Cleaning of procedural areas such as labor and delivery units
- Daily preparation of cleaning and disinfectant solutions
The IPC focal point or committee should also review and approve EVS products, such as disinfectants. This helps ensure that the product will be used as intended and that it meets established guidance.
EVS staff should be included in IPC trainings—they are part of the healthcare team. Given the unique functions of environmental cleaning, EVS staff should also receive job-specific training.
You’ll learn more below about environmental cleaning guidance for IPC staff.
-
The Healthcare Environment (10 min)
To keep patients and colleagues safe, IPC professionals must understand the potential role of the healthcare environment in disease transmission. The healthcare environment includes environmental surfaces—like patient beds and bathroom sinks—and medical equipment, like blood pressure equipment and IV pumps.
In the healthcare environment, there are a diverse number of microorganisms. They are present in our bodies and in our environment. The presence of a microorganism in the body and on healthcare environmental surfaces does not mean it will cause an infection. Most of these microorganisms are harmless, but some cause disease in susceptible hosts.
When patients receive medical treatment in healthcare facilities, the following factors can increase their susceptibility to infection:
- Patients who have underlying medical conditions such as diabetes, cancer, and organ transplantation are at increased risk for infection. These illnesses often decrease the immune system’s ability to fight infection.
- Certain medications used to treat medical conditions, such as antibiotics, steroids, and some chemotherapy medications, increase the risk of some types of infections.
- Medical devices and procedures such as urinary catheters, tubes, and surgery, increase risk of infection by providing additional ways that microorganisms can enter the body.
Microorganism survival and persistence in the environment depends on various factors, including type of surface, presence of organic matter, bioburden, temperature, and humidity. Because environmental contamination has been associated with transmission of pathogens in major outbreaks of healthcare-associated pathogens, like methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) and because these pathogens are known to persist on environmental surfaces for weeks and months, it is established that surfaces can play a role in disease transmission. However, it is important to note that environmental transmission of healthcare-associated infections (HAIs) can occur by different pathways.
Number of microorganisms present in the environment.The chain of infection pictured below illustrates that for any infection to spread, all steps in the chain must occur. The key to stopping the spread of infection is to break at least one link in the chain. For a full description of the chain of infection, refer to the Introduction to IPC module. Within the chain, the healthcare environment can act as a reservoir for pathogens.
It is important to understand that environmental cleaning reduces the number of microorganisms on environmental surfaces and medical equipment surfaces. Mitigating the role of the environment in the transmission of infectious agents requires collaboration between environmental services and IPC.
Environmental Surfaces and Medical Equipment
Environmental cleaning involves two main types of surfaces:
- Environmental surfaces: items like bed rails, tabletops, and floors
- Medical equipment: items involved in patient care, like monitors, IV pumps, and blood pressure machines.
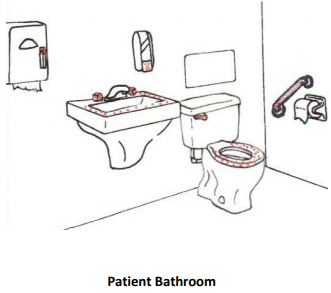
Patients and healthcare personnel touch some surfaces more than others, providing a greater risk of transmission. These are called “high-touch,” or frequently touched, surfaces. Frequently touched surfaces include door handles, light switches, bed rails, ends of beds, patient charts, monitor buttons, IV pumps and poles, and faucet handles. The images below are examples of these surfaces—the red dots indicate the areas often touched by HCW or patient hands.
Some surfaces are considered frequently contaminated given their function. Think of sinks, toilets/latrines fixtures, faucet handles, and bathroom countertops.

-
Knowledge Check (5 min)
-
General Functions of Environmental Services (5 min)
What is cleaning and disinfection?
Cleaning is the physical removal of foreign material, including dust, soil, and organic material such as blood, secretions, excretions, and microorganisms. It physically removes rather than kills microorganisms with water, detergents, and mechanical action. Cleaning is always essential prior to disinfection or sterilization. A surface that has not been cleaned effectively cannot be properly disinfected or sterilized. Organic material left on a surface or medical device can protect microorganisms or neutralize the action of disinfectants.
Disinfection is the inactivation or killing of most microorganisms on surfaces and items. It usually involves chemicals, heat, or ultraviolet light.
 When do you clean?
When do you clean?
At a minimum, all patient care areas should be cleaned once a day and more often when contamination is visible. Some national standards guide how often to clean the healthcare environment. Routine cleaning occurs when a patient occupies a bed or room, and terminal cleaning occurs when a patient has been discharged or transferred out of the bed or room. An example of procedures for routine and terminal cleaning is below.
Note that some patient care areas might require specialized cleaning procedures. Intensive care units, labor wards, and operating theatres are examples of areas where infection risk could be higher because of patients who are extremely susceptible or vulnerable to infection. Frequency of cleaning should take into account high-risk wards in the facility.
What about patients on Transmission-based Precautions?Transmission-based Precautions are used in addition to Standard Precautions for patients with known or suspected infections. You will learn more about Transmission-based Precautions in an upcoming module.
Bed spaces or rooms of patients on Transmission-based Precautions might require extra cleaning practices. Your facility should develop a protocol for environmental cleaning of areas with patients on Transmission-based Precautions.
Whenever possible, these patients should have designated patient care equipment used only for that patient. Always thoroughly clean and disinfect shared patient care equipment before use on a different patient. When cleaning patient care equipment, please follow manufacturer’s instructions to prevent damage of equipment, as different disinfectants are needed to clean equipment.
In some healthcare facilities, this is the responsibility of nursing staff, but all good cleaning strategies have clear roles and responsibilities for cleaning patient equipment. Please follow local protocol and policy.
-
Routine and Terminal Cleaning (10 min)
Let’s apply what we’ve learned. Click or tap the image below to see examples of routine cleaning and terminal cleaning.
Routine Cleaning
An example of routine cleaning of a patient bed space in an open ward includes:
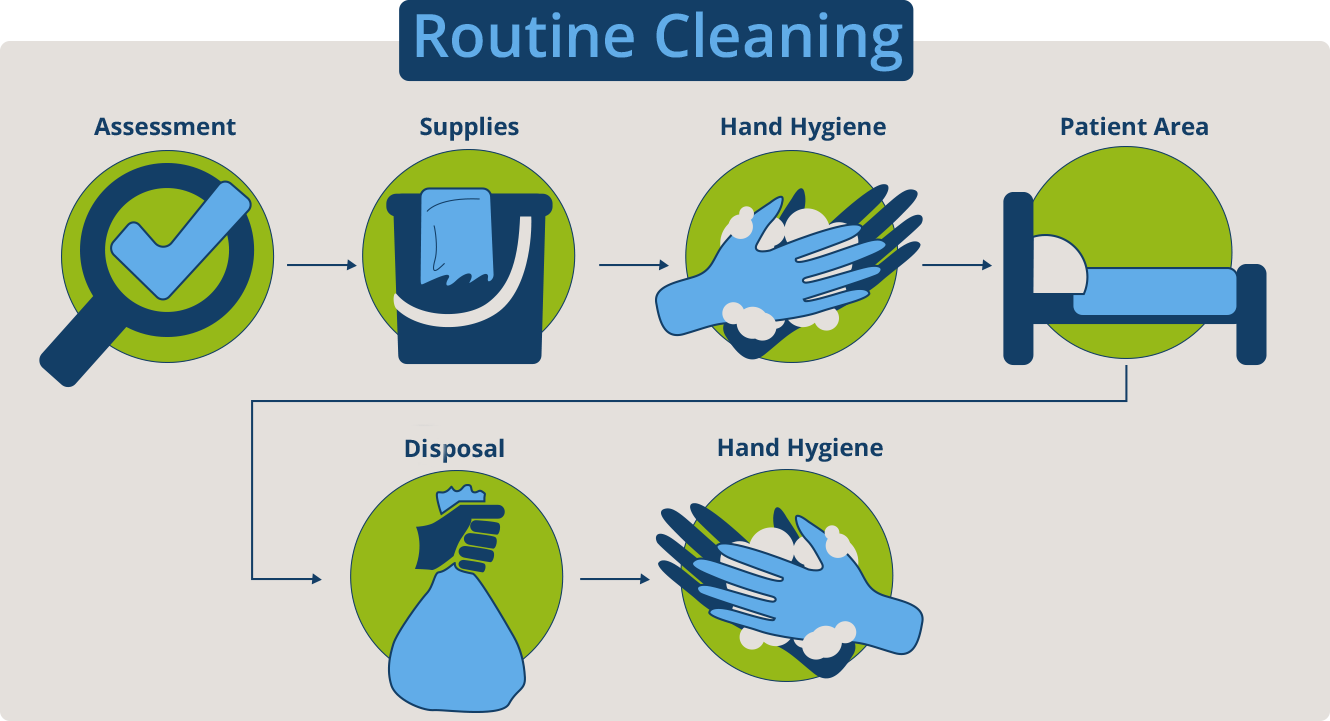
Assess
- Follow instructions on Transmission-based Precautions signage
- Visually inspect area to make sure there are no obstacles that could pose a challenge to safe cleaning, such as patient status, clutter, or worn-out or broken furniture and surfaces
Assemble supplies
- Make sure clean cloths are available
- Dilute cleaning (detergent) solutions correctly
- Restock missing or low-stock supplies
Hand Hygiene
Perform hand hygiene and put on gloves
Patient Area
Clean room or bed space with detergent solution, working from clean to dirtier areas and from high to low
- Check ceilings and walls and all areas for any visible soiling, and clean if required
- If privacy curtain, check for visible soiling and replace if required
- Clean all furnishings in the area including chairs, tables, and desks. Concentrate on frequently touched surfaces.
- Clean any light switches
- Clean medical equipment in area (IV pole and pump, monitors)
- Clean bed rails and any bed controls
- Clean commode or other private bathroom space
- Mop floor with detergent solution
Disposal
- Put used cloths in container to be laundered
- Segregate and place waste in appropriate containers (general waste, infectious waste)
Hand Hygiene
Remove gloves and perform hand hygiene with soap and water
Terminal Cleaning
If a patient room or bed becomes vacant, terminal cleaning is indicated. This is also called discharge cleaning in some countries. Terminal cleaning is meant to remove microorganisms that could contaminate the next patient occupying that space. It uses the same best practices as routine cleaning but is more detailed.
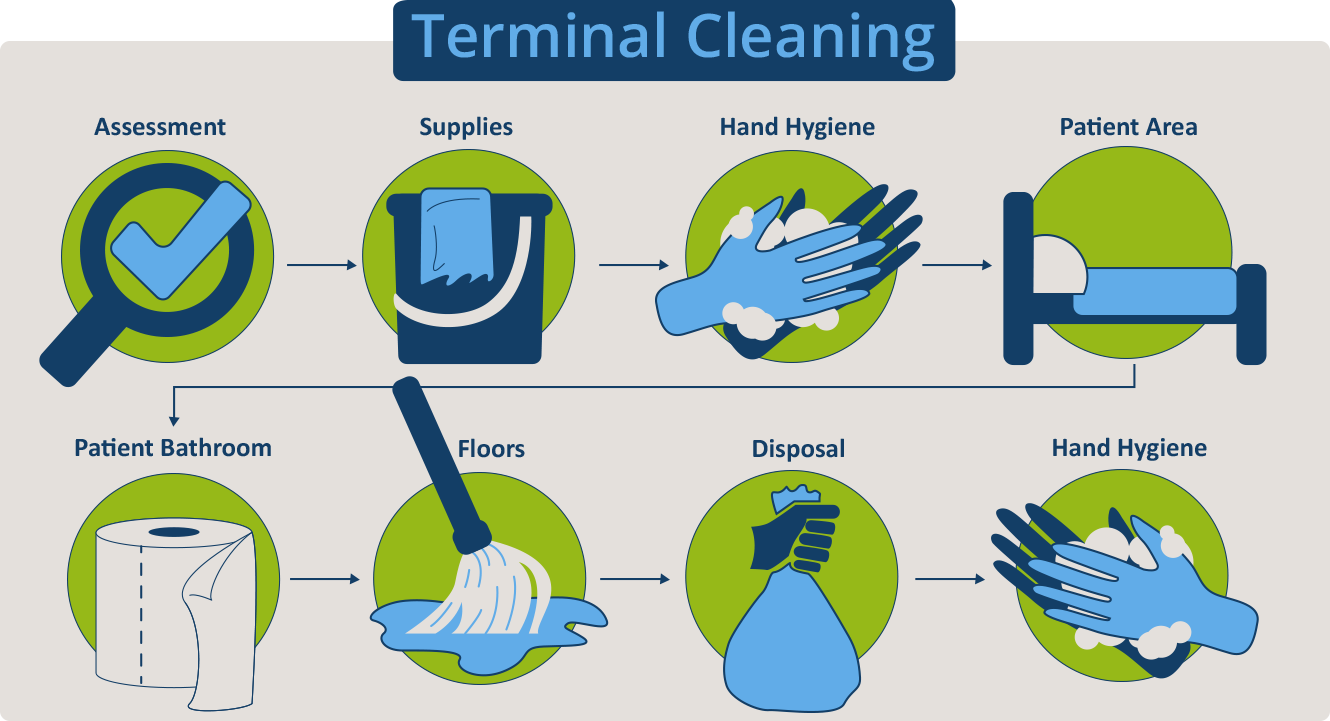
Assess
- Follow Transmission-based Precautions signage
- Visually inspect area to make sure there are no obstacles that could pose a challenge to safe cleaning, such as patient status, clutter, or worn-out or broken furniture or surfaces
Assemble supplies
- Ensure clean cloths are available
- Dilute cleaning (detergent) and disinfection solutions correctly
Hand Hygiene
Perform hand hygiene and put on gloves
Patient Area
Remove dirty linen as per local policy
- If any sheets on bed, roll sheets gently and carefully and put in soiled linen bag
Inspect window blinds and curtains (window, privacy); if soiled, clean blinds on-site and remove curtains and put into soiled linen bag
Clean and disinfect room or bed space, working from clean to dirty areas (toward the patient bed) and high to low.
- Check ceilings and walls for any visible soiling, and clean if required
- Clean any light switches
- Clean all furnishings in the area including chairs, tables, and desks. Pay attention to frequently touched surfaces.
- Clean medical equipment in area (IV pole and pump, monitors)
Clean and disinfect the bed
- Clean top and sides of mattress, turn over and clean underside
- Clean any headboard, footboard, bed rails, and bed controls; pay attention to frequently touched surfaces
Patient Bathroom
Clean and disinfect commode or other private bathroom space
Floors
Mop floor; clean and disinfect
Disposal
- Put soiled linen in designated area for laundering
- Put used clothes in container to be laundered
- Place waste in appropriate waste containers (general waste, infectious waste) as per local policy
Hand Hygiene
Remove gloves and perform hand hygiene with soap and water
Blood and Body Fluids
Now that you have seen how cleaning protocols apply to routine and terminal cleaning, let’s focus on how to clean blood and body fluid spills. Areas contaminated with these spills need to be cleaned and disinfected to prevent patient or healthcare personnel contact with infectious materials.
Manage spills by cleaning and then disinfecting using separate steps (combined detergent-disinfectant products cannot be used). Larger spills require a higher concentration of disinfectant because of the volume of the spill and a higher risk of transmission. Any staff managing spills of blood or body fluids should protect themselves by wearing appropriate PPE.
Click or tap the following tabs to read more about the steps for cleaning small and large spills.
Small Spills (splashes and drips)
Preparation: wear non-sterile gloves
- Wipe area immediately with paper towel or absorbent cloth (discard towels as infectious waste)
- Clean area with disinfectant solution
- Disinfect area with 500 ppm of hypochlorite (bleach) solution
- Dry surface with disposable paper towels
- Discard gloves and paper towels as infectious waste
- Send any reusable cleaning supplies (e.g., cleaning cloths) for reprocessing
- Perform hand hygiene, preferably with soap and water given exposure to body fluid risk
Large Spills
Preparation: wear non-sterile gloves; utility gloves may be preferred. If contamination of the front of the body is likely, wear a single-use plastic apron. Note: use of gown, mask, and goggles or face shield are not necessary unless there is a risk of splashes or sprays.
- If spill occurs in traffic path, block off area so others do not step through it
- Confine the spill and wipe it up immediately with absorbent (paper) towels, cloths, or absorbent granules (if available) that are spread over the spill to solidify the blood or body fluid (all should then be disposed as infectious waste).
- Pick up soiled paper towels/cloths and discard into infectious waste bag
- Clean the area with detergent solution
- Disinfect the area with fresh 5,000 ppm of hypochlorite (bleach) solution to disinfect; take care to allow the disinfectant to remain wet on the surface for the required contact time (e.g., 5-10 minutes)
- Rinse with water, as hypochlorite solution can be corrosive
- Dry surface with disposable paper towels
- Remove gloves and plastic apron and discard as infectious waste (in accordance with local policy)
- Send all reusable supplies and equipment (e.g., cleaning cloths, mops) for reprocessing after the spill is cleaned up
- Perform hand hygiene, preferably with soap and water given the body fluid exposure risk
-
Knowledge Check (5 min)
-
Contamination During Cleaning (5 min)
Cleaning should generate minimal dust or aerosols, so damp dusting and wet mopping is recommended over dry dusting and mopping.
Bucket solutions become contaminated almost immediately during cleaning. Continued use of the solution transfers more microorganisms to each surface that is cleaned. Some bacteria grow in both detergents and disinfectant solutions. Therefore, it is essential to make fresh detergent and disinfectant solution regularly and change it whenever visibly dirty, maintaining the appropriate concentration of solution. Discard any remaining solution after use.
Another source of contamination is the cleaning cloth or mop head, especially if left soaking in dirty cleaning solutions. It is important to disinfect cloths and mop heads, either with high heat in a washing machine or manually. A simplified approach is to replace soiled cloths and mop heads with clean items each time a bucket of detergent is emptied and replaced with fresh, clean detergent.
Mop buckets must be rinsed, dried, and stored upside-down to drain.
-
Protecting EVS Staff (5 min)
Environmental services staff should adhere to Standard Precautions when cleaning and follow any Transmission-based Precautions in place. This includes:
- Hand hygiene
- Use of personal protective equipment (PPE) when indicated
Hand hygiene is important during environmental cleaning activities. Click or tap each orange arrow to learn more about when hand hygiene is performed:
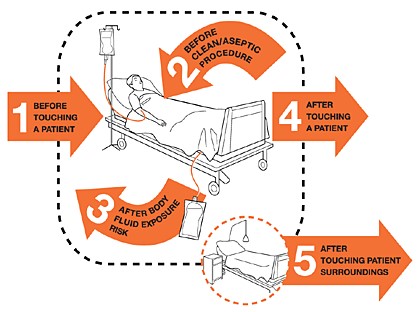
Moment 1. Before touching a patient
Clean your hands before touching a patient when approaching him/her to protect the patient against harmful germs carried on your hands.
Moment 2. Before a clean/aseptic procedure
Clean your hands immediately before accessing a critical site with infectious risk for the patient to protect the patient against harmful germs, including the patient’s own, entering his/her body.
Moment 3. After body fluid exposure risk
Clean your hands immediately after an exposure risk to body fluids (and after glove removal). This will protect both you and the health care environment from pathogens in blood and body fluids.
Moment 4. After touching a patient
Clean your hands after touching a patient and his/her immediate surroundings, and when leaving the patient’s side, to protect yourself and the health care environment from harmful microorganisms.
Moment 5. After touching patient’s surroundings
Clean your hands after touching any object or furniture in the patient’s immediate surroundings when leaving – even if the patient has not been touched – to prevent the spread of harmful microorganisms from inside the patient zone to the rest of the health care environment.
PPE
It is important to know what PPE is indicated when performing environmental cleaning activities. Click or tap the icons to learn more about the PPE used during cleaning:
 Wear gloves when handling hazardous materials such as cleaning solutions, disinfectants, or cleaning surfaces that are visibly soiled with blood or body fluids (such as large spills of blood).
Wear gloves when handling hazardous materials such as cleaning solutions, disinfectants, or cleaning surfaces that are visibly soiled with blood or body fluids (such as large spills of blood). Wear a gown if contamination of clothing or skin is anticipated (such as cleaning bed of incontinent patient).
Wear a gown if contamination of clothing or skin is anticipated (such as cleaning bed of incontinent patient). Wear a face mask and goggles (or face shield) when there is a risk of splashes or sprays of chemicals or blood or other body fluids.
Wear a face mask and goggles (or face shield) when there is a risk of splashes or sprays of chemicals or blood or other body fluids.
For patients on Transmission-based Precautions, PPE is required for environmental cleaning. For example, if Fatima, a cleaner, is about to clean the space of a patient on Contact Precautions, where a gown and glove are indicated for all persons entering the patient area, then Fatima should put on gown and gloves before cleaning that patient’s area. PPE is not indicated for cleaning non-patient care areas, such as offices.
-
Knowledge Check (5 min)
-
Chemicals (10 min)
Cleaning Solutions
Cleaning solutions contain detergents that remove dirt and debris (organic material) from surfaces. Detergents do not kill pathogens, but rather assist in removing them from surfaces. It is important to protect cleaning solutions from contamination as they can easily become contaminated during the cleaning process. Ideally, cleaning solutions used in a facility are hospital-approved detergents.
Disinfectants
Disinfectants inactivate or kill microorganisms on surfaces that have been cleaned. They are not intended for use as antiseptics. Like cleaning solutions, disinfectant solutions in buckets can easily become contaminated, which can transfer more microorganisms to surfaces. Replace these solutions frequently.
Commonly used disinfectants include:
- Alcohols (60-80% ethyl or isopropyl) for small surfaces
- Hypochlorites
- Disinfectants containing hypochlorite can easily be found in low-resource settings. If using hypochlorite, prepare a fresh solution every day using a standardized dilution and keep prepared solutions in a labeled container with a lid (to protect from sunlight and debris). Discard the hypochlorite solution at the end of the day even if it has not been used.
Less commonly used disinfectants include:
- Quaternary Ammonium Compounds (e.g., benzalkonium chloride)
- Hydrogen Peroxides (hydrogen peroxide that includes ingredients that improve its antimicrobial activity, cleaning efficiency, and material compatibility)
To be effective, disinfectants should be diluted to the correct concentration and remain on the surface for the appropriate contact time. Indications for use, dilution instructions, contact time, and safety information are found on the disinfectant label, which is provided by the manufacturer. Always check the product label to confirm the intended use of the chemical.
Contact time is the length of time a chemical needs to remain on a surface to inactivate microorganisms. Contact time varies by chemical.Indication for use (disinfectant for hemodialysis equipment)
Active ingredients
Health warnings
Biological activity/product claims
Manufacture date
Quantity
Notice that the dilution instructions, instructions for use, and contact time for disinfection are not on this label. Often, these instructions will be on the back label.
Selecting Chemicals
When selecting a cleaning agent (detergent) or disinfectant, consider the following:
- Intended use: Will it be used for cleaning (detergent), disinfection (disinfectant), or both?
- Efficacy: Does it kill microorganisms in the local environment? What is the recommended contact time?
- Acceptability: Does it damage surfaces, or leave a film or unpleasant smell?
- Safety: Does it have side effects for those who come in contact with it? What equipment is required for handling/use?
- Cost and availability: Does it fit the budget? Is it easy to obtain in the required quantity?
- Volume: Is it available in the amount needed, based on facility requirements?
-
Intro to Environmental Monitoring (5 min)
Monitoring and Assessing Environmental Cleaning
It's important to monitor and assess environmental cleaning to make sure that it meets best practices and is performed consistently and correctly. In later modules, you will learn that monitoring, feedback, and data will help you improve IPC programs in your facility.
Click or tap each method to read about monitoring for effective cleaning:
Observation
- Direct observation is watching an individual’s cleaning routine and giving feedback. Sometimes this method results in an individual changing their behavior because they know they are being observed.
- Indirect observation is visually inspecting an area after it is cleaned. This method is subjective—you can check for visible cleanliness but cannot tell if a surface is actually clean.
Environmental marking
This is the application of a colorless, ultraviolet (UV) visible (e.g., fluorescent) tracing solution to surfaces. After the surface is cleaned, UV light detects any remaining solution.
Here is an example of a sink handle in a patient room.
The left image shows the solution on the uncleaned handle.
On the right is the handle after cleaning. You can see that cleaning was inadequate because there are still fluorescent markings on the handle.
It's important to note that although visual markers can be helpful in identifying what has been cleaned, sometimes these solutions can be hard to remove. Also, visualization using these markers might not reflect actual cleaning practices.
Other Methods
Swabs for environmental culture and adenosine triphosphate (ATP) testing to assess the residual bioburden are available, but will not be discussed given the resources needed to implement and the limitations of these methods. Remember that routine swabbing of the environment for microbiological culture is not recommended unless in particular outbreak situations or at the specific request of the IPC team.
-
Knowledge Check (5 min)
3Omari, the cleaning manager, comes to you to consult. A disinfectant not previously used at the facility is now available for ordering. He asks you to help review the product label of the disinfectant. Answer the questions about the label below. (This is an example label, it is not a real product.)
-
Summary (5 min)
The healthcare environment can be a reservoir for potential pathogens. In this module, you have learned how environmental cleaning reduces the risk of potential pathogens in the healthcare environment. As the IPC focal person, your duties include collaborating with environmental services to ensure IPC is integrated in the daily workflow of cleaning staff. You also assist in reviewing and approving protocols for environmental cleaning throughout the facility. You will need to identify frequently touched and frequently contaminated surfaces in your facility to understand where risk of contamination is high.
Patient care areas have procedures for routine and terminal cleaning. Routine cleaning occurs when a patient occupies a bed or room. Terminal cleaning occurs when a patient has been discharged or transferred and is meant to remove microorganisms that could contaminate the next patient occupying that space. Precautions for patients on Transmission-based Precautions should be followed during cleaning activities.
Some patient care areas, such as the operating theatre, will require specific cleaning protocols given the risk of infection. If a blood spill occurs in any part of the facility, it needs to be cleaned and disinfected immediately according to protocol. Staff performing cleaning duties adhere to standard precautions, including hand hygiene and appropriate use of PPE.
As the IPC focal person, you also maintain awareness of the chemicals being used in the facility for cleaning and disinfection. You will need to understand the purpose and function of each chemical. This is another area where collaboration with EVS is important. Lastly, ensure that any environmental monitoring serves its intended purpose and is used to improve adherence to facility cleaning protocols.
You can also reinforce environmental cleaning through using a multimodal strategy:
- System change: having easily accessible products at the right concentrations
- Training and education: making sure that all relevant staff are trained on the importance of cleaning
- Monitoring and feedback: checking and providing feedback that cleaning has taken place and is of the right standard
- Reminders in the workplace: making it easy for EVS to implement protocols through posters and signage
- Institutional safety climate: having a culture in your facility that values the important role of cleaning


