Introduction to IPC
Infection prevention and control (IPC) is an applied discipline that affects all patient care activities in healthcare settings. IPC, including prevention of antimicrobial resistance (AMR), is an essential component of healthcare quality and patient safety. In this module you will learn how and why healthcare-associated infections (HAIs) occur and how IPC reduces their risk and spread. Effective IPC includes building a program with all healthcare personnel (HCP) playing their part to prevent the spread of pathogens and AMR.
Learning Objectives
By the end of this module, you will be able to:
- Identify possible causes of HAIs and describe how they are transmitted.
- Describe how risk recognition protects patients and healthcare personnel and identify risk factors associated with HAIs in healthcare settings.
- Describe the hierarchy of controls and how these controls reduce risk in healthcare settings.
- Identify how the IPC core components provide a blueprint for successful implementation of IPC programs.
Learning Activities
-
What Do You Know About IPC? (5 min)
IPC is integral to the safe delivery of health care. In this module you will learn why it is important to implement IPC programs and how they protect patients and HCP. First, test your knowledge of HAIs and IPC. Take your best guess by answering these true or false questions.
-
Defining Healthcare-Associated Infections (5 min)
Healthcare-associated Infections (HAIs) are infections that occur during the process of care that were not present or incubating at the time of admission. Microorganisms are found in many places, including air, soil, water, and our bodies. Some of them are helpful, but others can be harmful and cause infections.
An infection occurring in a patient during the process of care in a health-care facility which was not present or incubating at the time of admission. This includes infections acquired in the hospital but appearing after discharge, and also occupational infections among staff.In low- and middle-income countries, the burden of HAIs is high. Surveillance data suggest HAI prevalence is 2—3 times higher in low-income settings than in high-income settings. Vulnerable patients, such as those in intensive care units and those with invasive devices, are at a higher risk of developing an HAI. HAIs contribute to increased morbidity and mortality, length of stay, and healthcare costs.
Modern healthcare uses many types of invasive devices and procedures to treat patients and help them recover. Infections can be associated with the devices used in medical procedures, such as catheters and ventilators. These HAIs include central line-associated bloodstream infections, catheter-associated urinary tract infections, and ventilator-associated pneumonia. Surgical site infections can also occur.
An effective IPC program at a healthcare facility is essential for preventing and reducing HAIs and antibiotic resistance, and in preparing for, managing, and preventing infectious disease outbreaks.
-
How Diseases Are Transmitted (10 min)
To reduce the risk of harmful microorganisms, you must understand how different HAIs can spread. Microorganisms are found in air, soil, water, and in our bodies. Some microorganisms are helpful, others can be harmful and cause infections.
The diagram below represents the chain of infection. For an infection to spread, all steps in the chain must occur. The key to stopping the spread of infection is to break at least one link in the chain.
In a healthcare setting, the chain of infection refers to the numerous opportunities for pathogens to spread among patients, HCP, and the environment. Effective IPC aims to break the chain. You will learn more about this in the Standard Precautions and Transmission Based Precautions modules of this course.
Click or tap the boxes to learn more about each part of the chain of infection.
Infectious Agent
An infectious agent or microorganism, such as a virus, bacteria, or other microbe, that is capable of causing infection.
Reservoir
The reservoir is where microorganisms can be found. This can be a person (patient or HCP) or the environment. The healthcare environment contains diverse microorganisms. Environmental reservoirs include dry surfaces (bed rails and medical equipment), wet surfaces (faucets, sinks, and ventilators), indwelling medical devices (catheters and IV lines), and the environment around the patient.
Portal of Exit
Microorganisms must exit their reservoir to spread. For example, when someone coughs, microorganisms leave the reservoir (the person) through the respiratory tract. Portals of exit can include breaks in skin, mucous membranes (eyes, nose, and mouth), hands, blood, and the gastrointestinal and urinary tracts (as feces, vomit, and urine). Portals of exit can also be splashes from emesis (vomiting) patients or an exposed needle in an open sharps container.
Mode of Transmission
Microorganisms need a way to move (spread) from the portal of exit to the portal of entry. In other words, they need a way to get from point A to point B. Microorganisms usually depend on people, the environment, and medical equipment to move in healthcare settings.
Modes of transmission include:
- Direct
- Direct contact
- Droplet spread
- Indirect
- Airborne
- Contaminated equipment
In direct transmission, an infectious agent is transferred from a reservoir to a susceptible host by direct contact or droplet spread.
- Direct contact refers mainly to skin-to-skin contact, but it can also refer to contact with soiled surfaces.
- Droplet spread refers to spray with relatively large, short-range aerosols produced by sneezing, coughing, or even talking.
Indirect transmission refers to the transfer of an infectious agent from a reservoir to a host via suspended air particles and inanimate objects or equipment.
- Airborne transmission refers to infectious agents being carried over long distances through the air. Airborne particles include material that has settled on surfaces and become resuspended by air currents, as well as infectious particles blown from the soil by the wind. In contrast to droplets that fall to the ground within a few feet, airborne infectious agents can remain suspended in the air for long periods of time and can be blown over great distances.
- Contaminated items that can indirectly transmit infectious agents include food, water, biological products (blood), and fomites (inanimate objects such as bedding, surgical instruments, shared equipment such as x-ray and dialysis equipment).
Portal of Entry
IV catheters (and other devices) and surgical incisions can provide entryways for microorganisms to gain access to a susceptible host.
Mucous membranes (eyes, nose, and mouth) are an entryway for microorganisms spread by direct contact, sprays, and splashes. When healthcare personnel wear masks or face shields, this prevents microorganisms from coming in contact with the eyes, nose, or mouth.
Breaks in the skin, such as a puncture caused by a sharps injury, can also be an entryway. Notice that portals of entry can also serve as portals of exit and reservoirs for harmful microorganisms.
Susceptible Host
The final link in the chain is the susceptible host. When patients receive medical treatment, the following factors can increase susceptibility to infection:
- Patients who have underlying medical conditions such as diabetes, cancer, and organ transplantation are at increased risk for infection. These illnesses often decrease the immune system’s ability to fight infection.
- Certain medications, such as antibiotics, steroids, and some chemotherapy medications, increase the risk of some types of infections.
- Medical devices and procedures, such as urinary catheters, tubes, and surgery, increase risk of infection by providing additional ways for microorganisms to enter the body.
Understanding the chain of infections—infectious agents, reservoirs, modes of transmission, portals of entry and exit, and susceptible hosts—enables us to develop IPC measures to break the chain of infection.
- Direct
-
Standard and Transmission-based Precautions (5 min)
You learned that the role of IPC is to break the chain of infection. Standard and Transmission-Based Precautions are core IPC practices that healthcare personnel use to reduce transmission of microorganisms in all healthcare settings.
Standard Precautions aim to protect both HCP and patients from infectious agents—they are required in all healthcare settings. Standard Precautions are recommended for care of all patients in any healthcare setting, regardless of their suspected or confirmed diagnosis.
Standard precautions include:
- Hand Hygiene
- Environmental Cleaning
- Injection and Medication Safety
- Risk assessment with appropriate use of personal protective equipment (PPE)
- Reprocessing of Reusable Medical Equipment
- Waste management
- Respiratory hygiene/cough etiquette
You will learn more about each component in the Standard Precautions modules.
Transmission-Based Precautions are used in addition to Standard Precautions for patients who are suspected or confirmed to be infected or colonized with certain pathogens for which the mode of transmission is known.
Transmission-based Precautions include:
- Contact
- Droplet
- Airborne
The type of precaution assigned to a patient will depend on the mode of transmission of the suspected or confirmed pathogen. You will learn more in the Transmission-Based Precautions module.
For more information on core IPC practices, consult the CDC IPC Core Practices for Safe Healthcare Delivery in All Settings document.
-
The Importance of Recognizing Risk (10 min)
Risk recognition is a skill that every clinician and individual working in healthcare should be able to perform for both themselves and their patients: identifying sources of infection, or actions that can lead to infection. It relies on an understanding of why IPC is implemented, and not just memorization of what is needed. Risk recognition is a broad approach to IPC that includes both direct patient care and consideration of the surrounding environment.
All clinicians and healthcare personnel should constantly assess risk related to their activities. Real-time awareness enables immediate action to reduce or eliminate risk. A more formal assessment can be performed to assess and reduce risk related to environmental surfaces, new devices, or procedures, or factors related to physical layout and furnishings in the patient care area.
Below is an example of questions that can be asked for the purpose of assessing or recognizing risk and then taking appropriate action.
Click or tap the tabs below to read three scenarios about risk recognition:Questions to Consider Action to Take Decision 1: Do I need protection for what I am about to do because there is a risk of exposure to blood and body fluids, mucous I must follow Standard Precautions because there is a risk that I might expose myself to an infection that is transmitted via this route, or expose the patient to my microorganisms. Decision 2: Do I need protection for what I am about to do because the patient has undiagnosed symptoms of infection? I must alert someone about the patient showing symptoms so that a diagnosis can be made, and I must determine what precautions to perform to protect others and myself. Decision 3: What are the facility standards for a patient that has an identified infection? I must follow Transmission-based Precautions indicated for this infection to protect others and myself. Scenario 1
Phlebotomy is performed at a patient’s bedside. Yuri is an experienced phlebotomist. She spends much of her time performing repetitive tasks with her hands and bending to adjust her position to make the patient comfortable while she draws blood.
She knows that sharps injuries can cause transmission of bloodborne pathogens, such as human immunodeficiency virus, hepatitis B, and hepatitis C. She attends workshops annually to ensure that she is up to date on injection safety practices.
Scenario 2
Isaac cleans the operating room in the mornings. While wiping down the lights, he notices a stain on one of the ceiling tiles. He wonders how long the stain has been there, and if he should notify anyone. Surely someone other than he has seen it.
If there is water damage, it could indicate the presence of a larger problem. As environmental services staff, Isaac is unsure of his role in mitigating risk.
Scenario 3
Prior to a skin biopsy procedure, Salma, the nurse, sets up the necessary instruments and supplies.
-
The Hierarchy of Controls (5 min)
When risk has been recognized, do you know how to control it? The hierarchy of controls helps healthcare personnel determine the most reliable controls to reduce the risk from hazards during healthcare delivery. The image below represents this hierarchy: the most reliable methods do not rely on human behavior or memory. The best control is elimination or substitution of a hazard. When elimination or substitution are not possible, engineering controls can reduce potential exposure to hazards. Administrative controls and use of PPE at the bottom of the hierarchy require HCP to take specific actions to reduce the risk—they do not control the hazard itself.
Click or tap each control method on the image below to learn more: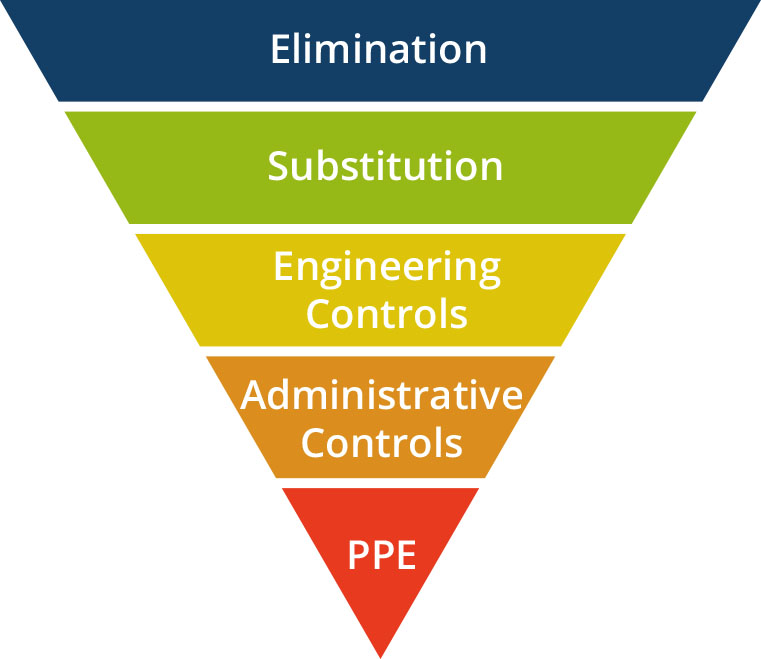
Elimination and substitution
Remove the hazard or substitute it with something with less risk. These methods are the most effective at reducing hazards; however, this tends to be the most difficult to implement. This is especially true if the risk is associated with an existing process.
Examples:
- Elimination: Using a suitable alternative instead of an injection
- Substitution: Using blunt-tip suture needles instead of sharp-tip needles
Engineering controls
This control method is designed to isolate healthcare personnel from hazards.
Examples:
- Prevent sharps injury by using safety-engineered syringes, needle shields, and sharps containers that prevent emptying.
- Use ventilation systems (e.g., negative-pressure room: pulling air from the hallway to the patient room and venting directly outside) that prevent airborne pathogens from leaving isolation room and exposing others in the hallway.
Administrative controls
These controls reduce risk by providing protocols and procedures for tasks. This type of control relies on people adhering to administrative rules.
Examples:
- Implementing contact precautions—for example, use of a single room, and of gloves and gowns—stops the spread of potential pathogens.
- A facility’s written IPC plans inform HCP of protocols.
- Education and training requirements for HCP enforce protocols.
- Screening assessment rapidly identifies infectious disease risk.
Personal protective equipment
PPE—gloves, gowns, surgical masks, respirators, eye protection, and other specialized clothing—plays an important role in IPC but requires consistent and correct use. It’s the least reliable control method because it does not control the hazard itself but relies on human decision-making and performance—meaning there is potential for human error. You can learn more in the Standard Precautions PPE module.
-
IPC Programs (5 min)
What is an IPC program?
An IPC program is a systematic, defined way to prevent HAIs and AMR and prepare for, manage, and prevent infectious disease outbreaks. An IPC program is a horizontal program, which means that it affects every aspect of patient care and is applicable in all patient care settings, from wound treatment to complex, invasive surgery. (A vertical program, like one for TB, deals with only a single disease.)
IPC professionals at healthcare facilities
Ideally, an IPC professional leads and oversees the development, implementation, coordination, and evaluation of the IPC program. The number of IPC professionals per facility depends on the acuity and complexity of the patient population. Greater acuity (severity of illness) and complexity will require more dedicated IPC staff.
Acuity, used here to refer to nursing care workload, is the complexity of care required for an individual patient or group of patientsFor facilities with limited or no IPC staffing, consider using a stepwise approach to implement IPC activities. As a starting point, a nurse or doctor might spend 1—2 days per week on IPC activities. Nurses on wards can be assigned to help expand the reach of IPC throughout the facility (i.e., link nurses or IPC champions). This approach can help build an IPC team while also increasing IPC awareness throughout a facility.
For further information on building an IPC program at a healthcare facility, refer to the WHO Interim Practical Manual on the Resources page of this course.
The core components of IPC programs
In 2016, the World Health Organization (WHO) released guidelines defining the elements of an effective IPC program. Known as the Core Components of IPC Programs, they serve as a roadmap for how IPC can prevent harm caused by HAIs and AMR. These components should be implemented together—all of them are required to build an effective IPC program. You will learn more about the core components and how to implement them in a later module.
The core components include:
- IPC program
- IPC guidelines
- IPC education and training
- Surveillance
- Multimodal strategy
- Monitoring/audit of IPC practices, and feedback
- Workload, staffing, and bed occupancy
- Built environment, materials, and equipment for IPC at the facility level
You can also reference the CDC’s Core Infection Prevention and Control Practices for Safe Healthcare Delivery in All Settings to learn more about IPC practices that are required in all healthcare settings. These are fundamental standards that are not expected to change based on emerging evidence and are applicable across the continuum of healthcare settings.
Implementing an IPC program
“Implementation” is another way to refer to the day-to-day activities of IPC. Implementation is a process, not an event, and does not happen overnight.
There are many ways to implement an IPC program. Each method depends on a strategy—a plan worked out in advance—to be effective. This can look different from one facility to another, depending on national, regional, or facility-level considerations. Implementing IPC also requires the support of key stakeholders and partner organizations. Each IPC professional or team works collaboratively to determine the best way to implement IPC.
At a minimum, the IPC program must clearly define roles and responsibilities, demonstrate administrative support, outline oversight and accountability, and ensure resources are provided.
A WHO implementation manual and a range of tools and resources have been developed for IPC staff in healthcare facilities. You can find links in the Resources section.
Multimodal Strategy
Implementation of IPC policies and practices is more likely to be successful with a multimodal strategy (using more than one method).
Let us look at an example of how to use a multimodal strategy in IPC.
Imagine that you are an IPC focal person and you notice that a significant number of injections in the medical ward are not being administered safely. Your first course of action might be to assess barriers to performing safe injections. Based on this, there might be a need to train relevant staff on how to perform safe injections. Training is an administrative control (in the hierarchy of controls), but it is only one activity, or strategy, that will influence implementation of this new practice.
So once training is complete, you decide to routinely observe staff, making sure to provide feedback (strategy No. 2). Then you could post job aids about safe injection practices in areas of the clinic where staff give injections (strategy No. 3). Purchasing safety-engineered syringes that reduce personal injury and prevent needle recapping would be strategy No. 4. These four activities combined—training, observation/feedback, posters/visual reminders, and purchasing safety-engineered syringes—constitute a multimodal strategy and give you a greater chance of successful implementation.
You can find more detailed information in the WHO Core Components and Multimodal Strategy module.
-
Knowledge Check (5 min)
-
Summary (5 min)
In this module, you have learned that HAIs are caused by microorganisms that can spread from person to person via direct or indirect contact. The chain of infection describes how infection and disease are spread. HCP should always use risk recognition to identify and reduce risk during healthcare activities. Facilities can make systematic and behavioral changes to reduce these risks. The hierarchy of controls describes these changes and specifies methods that reduce risk with varying degrees of reliability. The WHO core components and CDC core IPC practices help development and implementation of an effective IPC program. You will learn more in other modules.
