Implementation Approaches to Reducing SSI
Learning Objectives
Now that you have learned about the WHO recommendations and the importance of preventive measures in reducing SSI risk, let us look at ways you can successfully implement these recommendations in your facility. This third section in the SSI module will cover adaptive and technical approaches to improving and applying the WHO multimodal strategy. You will also learn about the Surgical Unit-based Safety Programme (SUSP) and how it has been used in various countries to reduce SSI rates.
By the end of this module, you will be able to:
- describe adaptive and technical improvement approaches and the role of process and outcome indicators, which form part of an improvement project applied to SSI prevention;
- explain how evidence-based recommendations on SSI can be implemented effectively in both the local context and real-life situations; and
- describe and explain the WHO multimodal improvement strategy designed to implement SSI prevention recommendations.
Learning Activities
-
SSI at Your Facility (10 min)
Take a moment to think about SSI where you work. In the boxes, list three ways in which patients may get a surgical site infection at your surgical service/facility. For each item, describe what you think can be done to prevent this.
How Patients Get SSI Prevention Measures This section will cover several approaches and tools that can be used to reduce SSI. Think about how you could use these approaches to implement your ideas for preventing SSI at your facility.
-
Technical & Adaptive Work (10 min)
IPC interventions will be most successful if they combine technical work with adaptive work. Using both approaches will help ensure that staff are supported to consistently perform tasks the right way, and that safe practices become the norm.
Click or tap on each circle in the diagram to learn more about each of these aspects.
Technical work
Technical work involves evidence-based interventions. It is work that we know we should do—that is, implementing recommended practices, such as appropriate surgical antibiotic prophylaxis dosing and skin preparation. This type of work lends itself to standardization (e.g., in the form of checklists and protocols).
Adaptive work
Adaptive work is the intangible work that shapes the attitudes, beliefs, and values of health care workers so that they consistently perform tasks the way they know they should. The adaptive approach specifically aims at creating or improving the local safety climate and motivating local teams to comply with prevention measures targeted by the technical work. It includes actions to explore and discuss local beliefs about patient safety, engage local leadership, identify and support local champions, improve communications, and promote accountability of frontline staff and teams. The Armstrong Institute for Patient Safety and Quality at Johns Hopkins University has developed a five-step programme that focuses on HAIs and improves communication skills (e.g., ensuring team members speak up with concerns) and teamwork (e.g., team members holding each other accountable) among other improvements. The approach focuses on a culture of safety and people-centred service delivery, which often involves patient participation.
This programme is known as the Comprehensive Unit-based Safety Programme (CUSP). It consists of five steps:
- educating staff on the science of safety
- identifying defects
- assigning an executive to the unit
- learning from one defect per quarter
- implementing teamwork tools.
For more information about adaptive work, see the Resources section on CUSP and the Leadership in IPC module.
Your overall aim should be to embed SSI evidence-based recommendations (covered in the previous section) as an integral part of the IPC improvement programme in your health care facility. This will also involve looking at aspects of the safety culture, which you will learn more about in the learning activities for the SUSP study.
The WHO’s five-step implementation cycle provides a validated process for systematically addressing improvement projects in your facilities. This cycle is covered in the Implementation Strategies and Quality Improvement section of the Leadership module.
Click or tap on each step to learn more about how undertake the five-step implementation cycle.
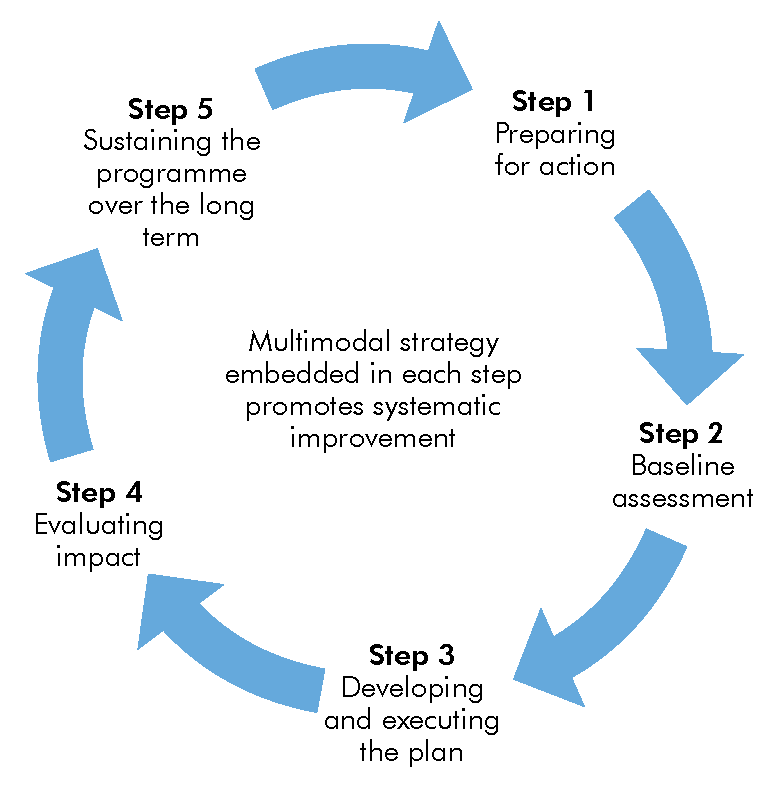
Step 1. Preparing for action
In step 1, you prepare to improve SSI prevention in your facility. In this step, a multidisciplinary team should be established to work on SSI prevention improvement. The team should include IPC focal points and teams, surgeons and surgical nurses, technical support staff, pharmacists, anaesthetists, and any professionals directly providing surgical care, as well as quality improvement leads. Clear roles and responsibilities should be progressively defined, and the team should start to plan the local intervention using a multimodal strategy (see the next reading, WHO Multimodal Strategy and SSI Prevention). The team might start by putting in place resources and measures that will support successful implementation of the interventions required to improve SSI processes and outcomes. The team should also identify and engage key leaders and stakeholders, and establish linkages with other key programmes; this will make your efforts more sustainable. You should start your communications and advocacy for SSI interventions throughout the facility as part of this step. Depending on the facility, this step can take months.
Step 2. Baseline assessment
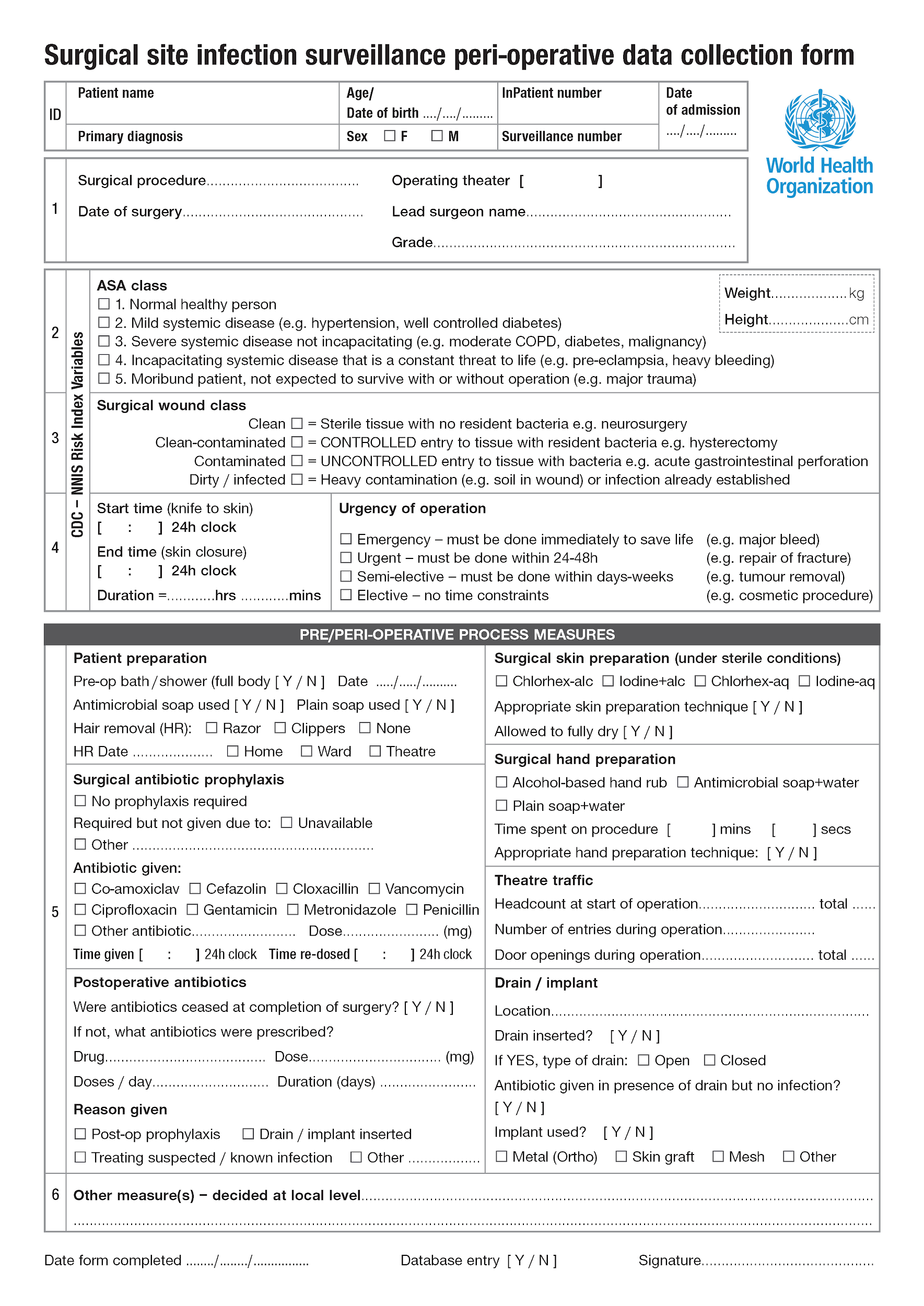
In step 2, an exploratory baseline assessment of the current SSI situation (as well as SSI prevention measures) at your facility should be conducted. If your facility does not have the necessary assessment tools, you could use WHO’s SSI surveillance peri- and postoperative data collection forms. Even if your facility conducts SSI surveillance and has implemented some SSI prevention activities, having a baseline report is still important. The team should agree to a timeline for baseline assessment and reporting.
The baseline assessment should clearly highlight strengths, weaknesses, risks, and needs, and may even highlight resource gaps that have not yet been addressed. Highlighting existing strengths and achievements is important in convincing decision-makers, surgical teams, and other stakeholders that further success and progress is possible. The WHO preoperative assessment tools can help you address process indicators important for prevention, and not just patient outcomes, of SSI.
This step will also help with engagement, communications, and advocacy.
‘Assessment fatigue’ is a risk. Figuring out ways to embed baseline assessment work as part of existing activities/facility goals will reduce this risk. So, if you are already collecting data for another activity, add SSI-related assessment questions to that data collection activity.
Step 3. Developing and executing the plan
In step 3, the team acts on the results of the baseline assessment to inform a plan of action, including setting SSI prevention intervention priorities for your facility. Further discussion and consensus with key leaders and other stakeholders may also be necessary. Be sure to create a realistic, priority-driven action plan based on your local context. It is important to focus initially on achieving short-term wins. Some testing of the intervention plans may be useful at this stage. (See the Implementation Strategies and Quality Improvement section of the Leadership module to learn about one kind of testing method: Plan, Do, Study, Act.)
The action plan should include updating or identifying responsibilities, timelines, budgets, and review/reporting dates, and establishing practical ways of implementing the SSI prevention programme in your facility. You might need to obtain special expertise (human resources) or other kinds of resources, such as a database for data collection, a budget for designing and printing new awareness-raising posters (related to the SSI interventions), or a budget for purchasing or producing alcohol-based handrub. Remember to get approval for your action plan.
Step 4. Evaluating impact
In step 4, the team makes critical decisions, evaluates the sustainability of the interventions, and modifies action plans. Collect and collate evidence to determine what interventions have worked. Your action plan can then be updated.
You should also conduct a follow-up assessment using the same tool or tools you used for the baseline assessment; using the same tools will ensure that same kind of information is gathered. All key leaders, stakeholders, and others who were identified in previous steps should review the follow-up assessment. Be sure to establish a regular schedule of evaluation.
Step 5. Sustaining the programme over the long-term
In step 5, the team determines how the SSI prevention interventions and improvements can be sustained and addresses gaps that may be hindering SSI prevention (which may include resources). At this point, your facility should be gradually integrating the improvements into routine clinical practices. Be sure to include all key stakeholders in discussions.
The team should consider which actions you might need to take to counteract fatigue, such as a campaign focusing on a certain aspect of SSI practices. You may face challenges, such as key leaders leaving the facility or moving to different projects.
Build on what you have learned, your current understanding of the local situation, and the organization of the overall IPC programme to ensure that prevention of SSI is considered a critical part of the business of your health facility. Be sure to build on the momentum of your work so far, celebrate success, and maintain engagement! Remember to systematically revisit all the steps to keep focused on the ongoing improvement plans.
-
WHO Multimodal Strategy and SSI Prevention (10 min)
The WHO Multimodal Strategy consists of using several elements or components in an integrated way (thus addressing both technical and adaptive aspects) with the aim of improving an outcome and changing behaviour. This practical improvement strategy should include tools—such as training materials, bundles and checklists, posters, standard operating procedures, assessments, and observation/survey tools—that are developed or adapted by multidisciplinary teams and take into account local conditions and potential for success. Many of these resources are already available at your facility. We will discuss other tools recommended by WHO (or used in other countries) later in this section.
Click or tap on each strategy to learn about how it can be applied to SSI prevention.
Build it
For any intervention to be successful, health care facilities must have the necessary infrastructure and resources. Having the right infrastructure and available resources can streamline SSI prevention activities so that delivery of care remains consistent and execution of these activities is easier and safer.
Your facility may need to address the following types of infrastructure and resources:
- allocated budget for the exact intervention (this may have already been addressed during the preparedness step)
- standard operating procedures/protocols/local policies and tools/mechanisms for training
- an IT or paper-based system for monitoring and feedback on infrastructure, resources, and other improvement steps
- surgical services/human resources, including a dedicated, competent team to ensure SSI prevention activities are working with an action plan
- laboratory services
- continual procurement of the following supplies, depending on the prevention measures prioritized:
- products for surgical hand preparation (procurement vs. local production)—ABHR, antimicrobial soap
- sterile drapes and gowns
- appropriate antibiotics for surgical antibiotic prophylaxis (that are easily stored and accessible for use when they are needed), and those needed to be given with mechanical bowel preparation (MBP)
- clippers (if hair removal is required)
- alcohol-based chlorhexidine solution (procurement vs. local production)
- Mupirocin 2% ointment
- oxygen
- antimicrobial-coated sutures
- negative-pressure wound therapy devices
- nutritional formulas
- warming devices
- fluid therapy
- aqueous povidone-iodine solution (when considering irrigation)
- standard postoperative wound dressings
Teach it
One barrier to improvement is insufficient knowledge on the part of health care workers and patients about SSI prevention measures and why they are important. Practical training and education can overcome this barrier. Activities under this component could include:
- onsite hospital courses
- bolus (that is single, relatively large training) sessions
- simulation sessions for skills training
- use of locally made or online videos
- online e-learning courses (often self-directed) and/or webinars
- focus groups and workshops
- bedside training
- in-person sessions, including ward rounds, grand rounds, town hall meetings, coaching visits
- pre- and post knowledge and perception tests
- training support materials (handouts, booklets, patient information leaflets, etc. This links with the Sell it component.)
Check it
This element is reflected in steps 2 and 4 of the implementation cycle and is essential for identifying areas that need improvement, which in turn informs local action plans (step 3). It is critical to measure improvements resulting from interventions to determine whether these efforts have been effective. Regular monitoring and feedback of activities and improvement projects should not be seen as separate from implementation or used only for scientific purposes. For example, imagine your facility is improving surgical hand preparation. Operating room staff should be assessed on when and where they perform this, correct use of the product and technique applied, and receive feedback about how well they do.
Monitoring SSI may include addressing:
- risk factors for SSI (as outlined in other sections of this unit)
- compliance with WHO-recommended procedures and practices
- infrastructures and available resources and supplies
- knowledge and perception of the problem
- SSI rates.
The following approaches may help:
- a clear plan to ensure monitoring commences before projects/improvements are implemented, so that progress can be clearly monitored
- direct observation (by a senior nurse or physician)
- targeted audit tools
- use of the WHO Surgical Safety Checklist
- different formats for providing feedback, agreed upon locally to ensure they engage all the right staff (including IT systems for support). Real-time and personalized feedback have proven beneficial, as has ensuring that reporting of results reaches diverse teams.
Sell it
The Sell it component is about promoting an intervention to ensure that there are cues to action at the point of care, and that messages are reinforced among health care workers and patients. These activities may include:
- reminding and prompting health care workers about the importance of practices to prevent SSI;
- informing patients and their visitors of the standard of care they should expect to receive;
- communicating to senior leaders and decision-makers which standards they should assure.
The following tools can help you “sell it”:
- posters
- leaflets
- banners
- stickers
- flowcharts
- infographics
- letter templates
- advocacy messages suitable to the local setting (e.g., social media messages, memos)
- manuals
- electronic reminders built into the hospital IT system
- telephone calls (for patient reminders).
Some of these tools are available from WHO, but tools developed locally by the SSI prevention programme team would be the best option. Posters can be a particularly effective tool to remind busy health care workers of proper IPC practices, including ways to prevent SSI. However, they need to be regularly reviewed to ensure they are still effective and still present in the right places in the health facility. Large-scale facility reminder initiatives, such as campaigns, can at times help support behaviour change. It is important that any reminder materials are both consistent with what is contained in policies and included in training and education sessions.
Live it
All levels of the health care system should support projects to prevent SSI. It is important to create an environment for raising awareness about SSI prevention and a climate that prioritizes surgical safety issues. Senior managers should encourage team spirit and cohesion. Staff should be aware that they have the capacity to make improvements, and should feel they have ownership of these projects. Culture assessment surveys can support progress.
Important aspects of this component may include:
- motivated, well-functioning multidisciplinary teams
- champions
- role models
- visible leadership (including rounds)
- morbidity and mortality meetings with participation by senior hospital staff—to learn from defects and facilitate a culture of sharing for improvement
- advocacy messages from leaders (delivered in a timely manner).
-
Overview of a Surgical Unit-based Safety Programme (5 min)
SUSP is one model that combines technical and adaptive approaches and uses a multimodal improvement strategy. It provides tools and resources to improve the safety culture and reduce SSI. SUSP aids tracking of valid performance measures and engages local frontline clinicians and hospital leaders to implement evidence-based interventions and improve patient care. It not only supports infrastructure development but also aims to improve teamwork and have staff learn from mistakes.
SUSP combines the CUSP approach (adaptive work) with IPC best practices (technical work) to achieve three goals:
- improve safety for patients undergoing surgeries;
- reduce SSI;
- reduce surgical complications.
An important part of SUSP is allowing the local facility/team to decide what needs to be improved, based on their knowledge of known or perceived gaps. Frontline staff identify local defects and, with managers and administrators, develop a detailed SSI prevention intervention to address these defects and issues.
Using the SUSP approach
The following recommendations for getting started with using an SUSP approach to reducing SSI in your facility are based on experiences in the US and in Africa. These factors contributed to the success of SUSP, and reflect aspects of the WHO multimodal strategy it is important to consider from the outset—specifically building a safety culture (Live it), monitoring and feedback (Check it), and reminders and communications (Sell it)
- Assemble a multidisciplinary team to include, as the core team, surgical staff, anaesthetists, and IPC staff.
- Engage a senior executive as part of your team.
- Implement with the intention of improving perioperative teamwork, communication, and the safety culture.
- Regularly meet as a team to implement interventions and monitor performance.
- Collect a minimal set of standardized surgical outcome data monthly.
-
SUSP in Sub-Saharan Africa (15 min)
Let us look at the experience of some hospitals in resource-limited settings implementing SUSP. From 2013 to 2015 a cohort study1 was done at five hospitals in four countries (Kenya, Uganda, Zambia, and Zimbabwe) to compare SSI rates before and after implementation of SUSP SSI prevention projects. (The projects described in this reading may help give you ideas of what you can do at your facility. Use the study results to convince staff that taking preventive measures will reduce SSI.)
A local multidisciplinary team was established at each hospital (as mentioned in step 1), with some supervision and remote support from an IPC team from WHO and Armstrong Institute for Patient Safety and Quality at Johns Hopkins University School of Medicine. Similar to how we asked you at the beginning of this module about how patients might contract SSI at your facility, local teams were given a tool asking about the most frequent ways in which patients may get a surgical site infection at their surgical service/facility.
Through this exercise they determined the following IPC practices were inadequate or inappropriate at their facilities:
They used the SUSP Perioperative Staff Safety Assessment Tool
See the Resources page for the SUSP Perioperative Staff Safety Assessment Tool.
- surgical antibiotic prophylaxis (SAP)
- patient bathing
- hair removal
- surgical hand preparation
- surgical skin site preparation
- discipline in the OR
- equipment use, including sterile gloves, sterilization, clippers, drapes, gowns
- training and education for staff and patients.
Based on this gap analysis, each site implemented projects to reduce SSI by doing technical work combined with adaptive work to improve the safety climate.
Click or tap on each topic to learn more about those projects/activities.
Promotional materials
Some of the hospitals created videos and posters to encourage behaviour change relating to consistently improving practices. Surgeons from hospitals recorded a video similar to one that was made to promote CUSP in the US. Having local health care workers adapt or create new tools means that they have ownership in the intervention, and can make sure the materials are applicable to their context, thereby ensuring that the right organizational culture or safety climate is achieved to influence and support local change.
Data collection
Some of the hospitals used or adapted surveillance tools to collect data on SSI, including standardized data against SSI definitions and process measures such as surgical hand prep and SAP administration. This allowed hospitals to understand what was working and what was not in relation to safe surgical care and preventing SSI. This information was critical for reporting to surgical staff and key teams and for creating new protocols.
Some countries have their own SSI protocols and surveillance forms; in some it is mandatory to collect SSI surveillance data. If your country does not already have surveillance collection tools, you can use the WHO surveillance forms protocol (see the Resources section), which are designed for low-resource settings.
The surveillance training module provides guidance on which data is important to collect, which will help you in adapting the forms.
New SAP protocol
One hospital adopted a new SAP protocol, which had information and instructions specific to their context and addressed behaviours that needed to be changed, using a multimodal strategy. This included:
- preparing and agreeing upon a new protocol at the local level with the multidisciplinary team, with visible signoff by senior leaders, based on available evidence of local antimicrobial resistance patterns;
- deciding on antibiotics affordable and available locally including strengthening procurement;
- placing the SAP protocol in a visible place in the operating room to help people adhere to the protocol;
- checking on the administration of SAP with feedback to staff.
Improving Surgical Hand Preparation
Another activity in this study looked at locally producing ABHR using the following modified WHO formulations suitable for surgical hand preparation. See the Resources section for the Guide to Local Production: WHO-recommended Handrub Formulations.
Formulation IFinal concentrations:
- ethanol 80% w/w
- glycerol 0.725% v/v
- hydrogen peroxide 0.125% v/v
Ingredients:
- Ethanol (absolute), 800 g.
- Hydrogen peroxide (3%), 4.17 ml.
- Glycerol (98%), 7.25 ml (or 7.25 x 1.26 = 9.135 g).
- Top up to 1000 g with distilled or boiled water.
Final concentrations:
- isopropanol 75% w/w
- glycerol 0.725% v/v
- hydrogen peroxide 0.125% v/v
Ingredients:
- Isopropanol (absolute), 750 g.
- Hydrogen peroxide (3%), 4.17 ml.
- Glycerol (98%), 7.25 ml (or 7.25 x 1.26 = 9.135 g).
- Top up to 1000 g with distilled water. WHO guidelines describe the benefits of using ABHR.
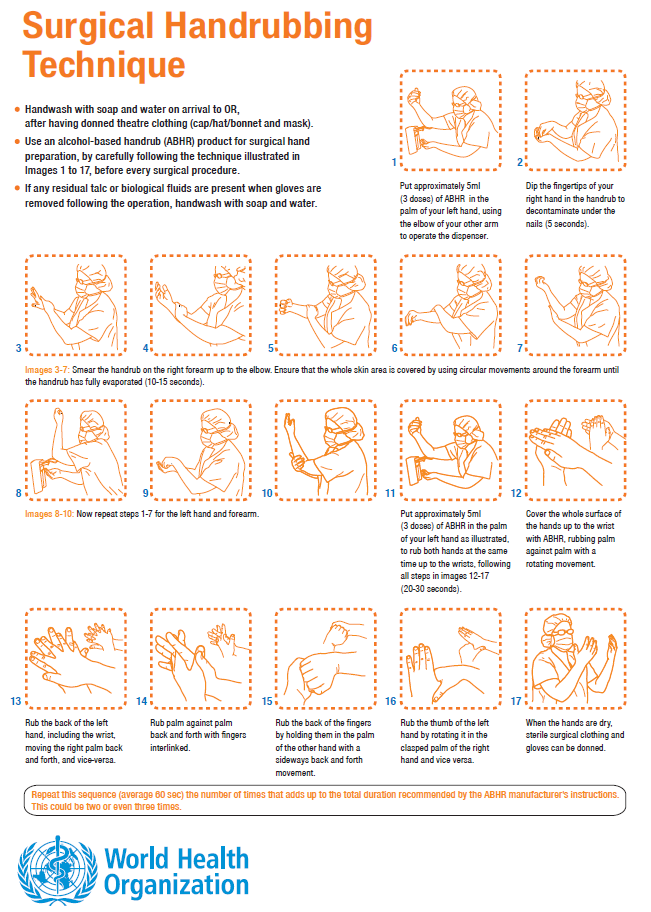
Additionally, posters and dissemination of messages in other formats agreed upon locally provided key information on use of ABHR for surgical hand preparation to make sure staff knew about the new procedures, and to encourage their commitment to changing practices. These new practices were:
- washing with antimicrobial soap and water or using ABHR as an alternative to soap and water for surgical hand preparation;
- ensuring the right technique in rubbing hands and covering all surfaces during the procedure (see the Resources section for the poster); and
- not using nail brushes.
Not only was ABHR readily available (because it was produced locally), but also surgeons consistently used ABHR. This success is due in part to fact that the whole team were involved in this process, not just the IPC leads, and training and reminders were provided (thus reflecting a multimodal strategy for improvement).
Surgical skin preparation
Another activity in the SUSP study was the local preparation of an alcohol- and chlorhexidine-based skin disinfection product for surgical skin preparation (according to the related WHO recommendation). One site coloured the solution pink to ensure it was visible (especially on dark skin) during the skin preparation process.
Formulation- isopropanol: 62.7% g/g
- chlorhexidine digluconate 18.8% g/g solution: 12.1% g/g
- and distilled water up to 100%
Study Results
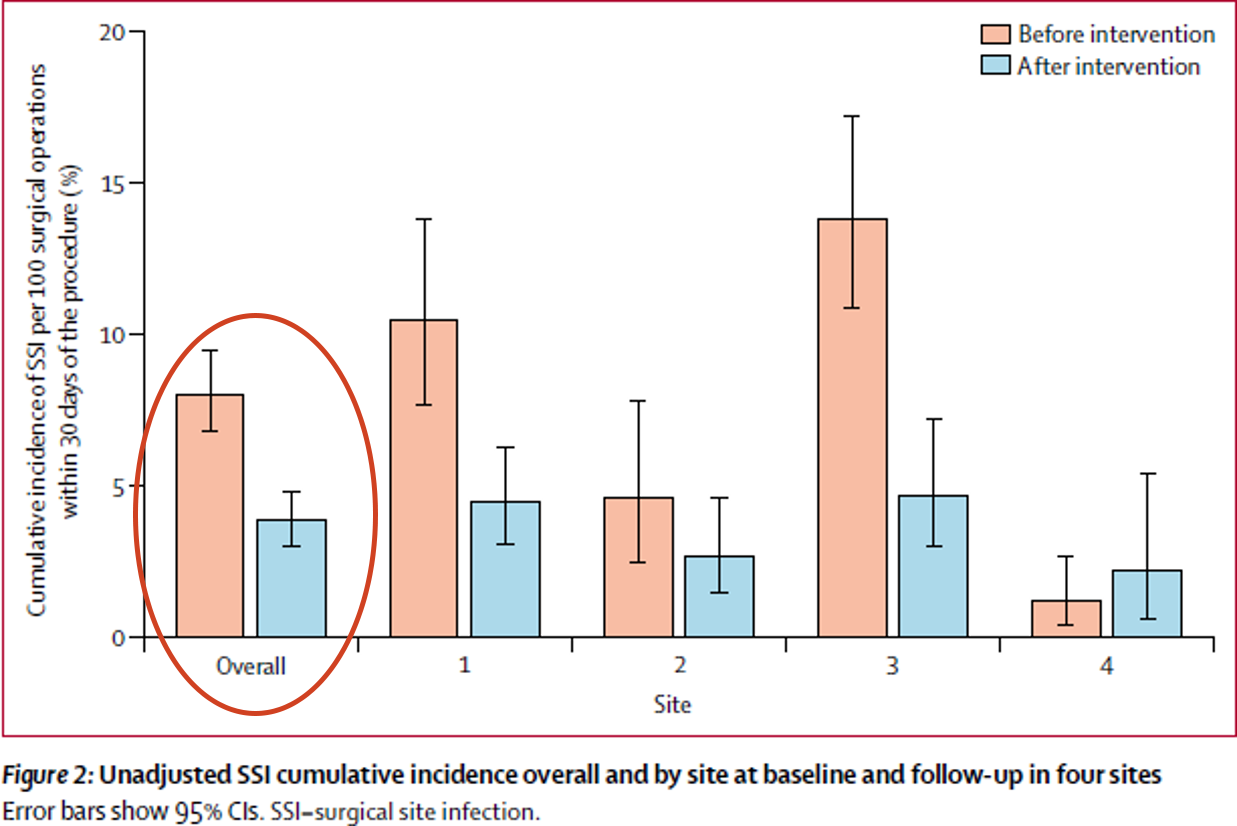
The teams at the five hospitals where SUSP was implemented evaluated the overall SSI risk and occurrence, as well as compliance with SSI prevention practices, at their hospitals before and after the projects (although one hospital had to drop out) to see whether there were improvements. As this table shows, the SUSP approach made a difference: there was a significant change in IPC practices. The key finding from these results is that all but two process measures improved significantly following implementation of the project, and a number of the practices were also sustained over time.
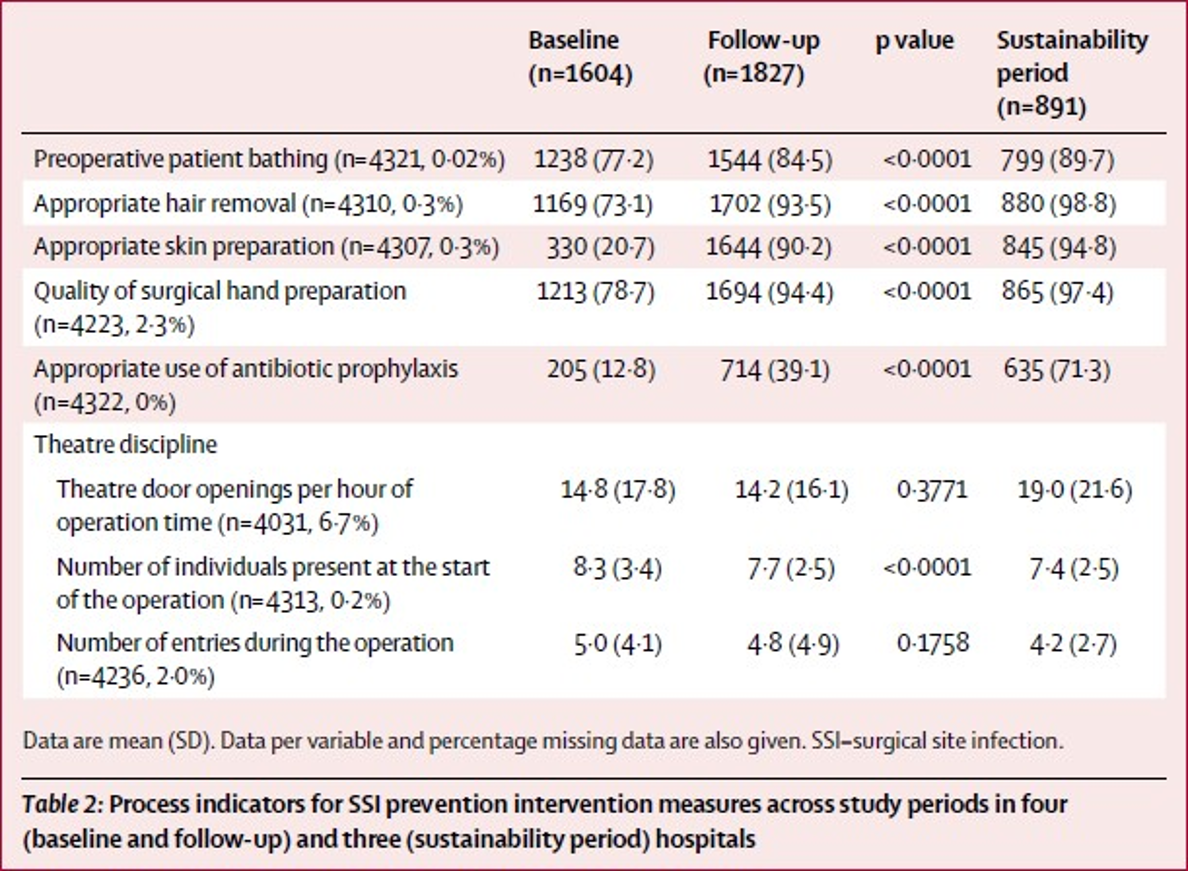
This figure and additional multivariate analysis (see published paper) shows that the intervention and related improvement in safe surgical practices were associated with reduced incidence of SSI overall (the study was not charged with measuring changes at individual hospitals).
Tips for Success
Here is a summary of tips for successfully implementing SSI prevention projects based on SUSP:
- Have a stepwise action plan.
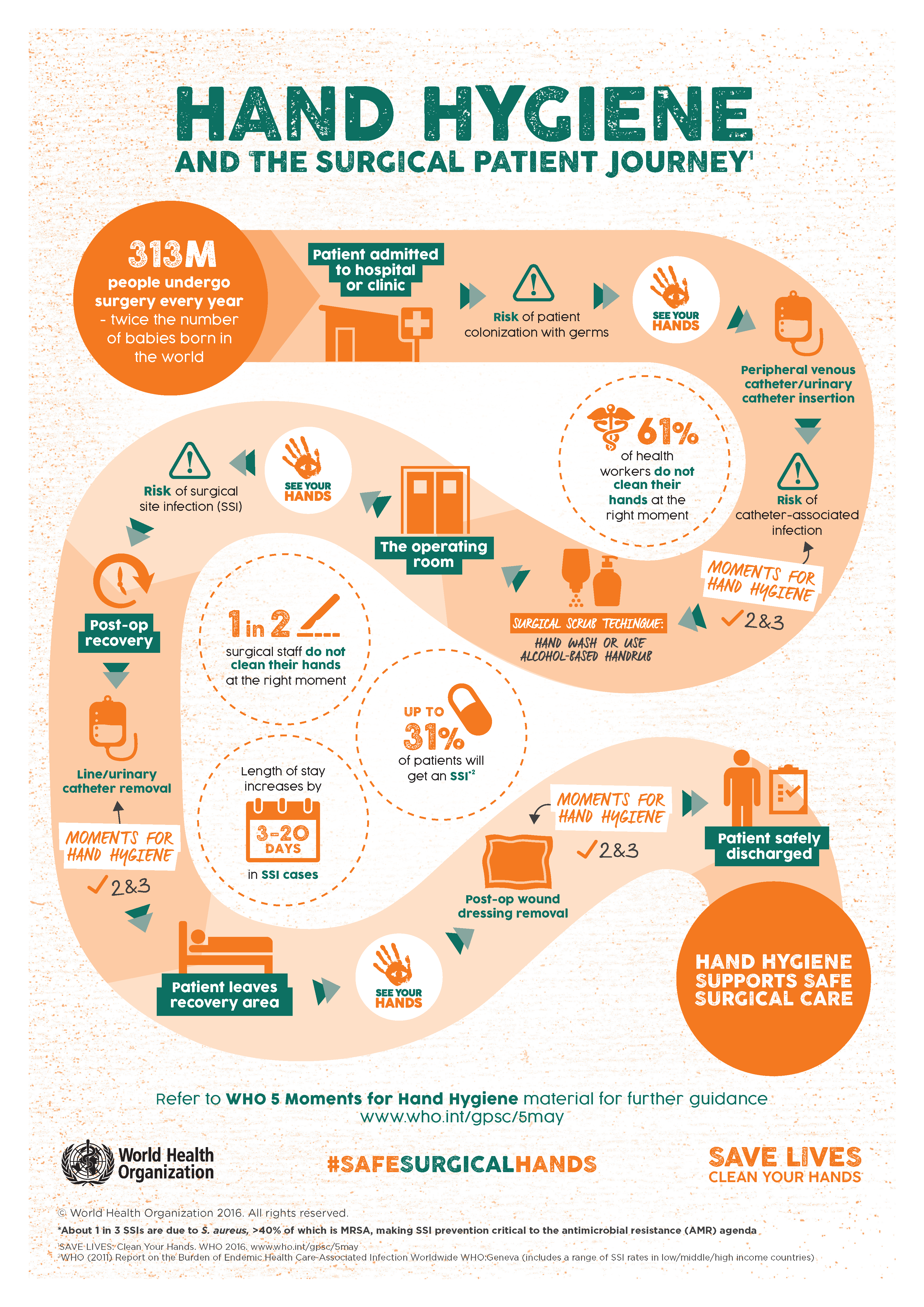
- Map the required recommendations according to the surgical patient journey so as to target the right people in the surgical team.
- Empower teams and involve frontline staff in decision-making.
- Engage leadership and ensure their commitment is visible to staff.
- Let teams take the lead on adapting existing tools and resources, while maintaining the focus on evidence-based recommendations.
- Catalyse collective and individual ownership of the interventions being undertaken.
- Use data to create awareness and understanding.
- Award teams and work with a positive safety culture spirit.
See the Resources section for the entire article Compliance improvement for all preventative measures.1
-
Starting SSI Prevention Plans at Your Facility (15 min)
Recall your list of ways patients get SSI at your facility. You also listed a way (or ways) to reduce that risk. Let us refine your ideas for improvement into concrete plans. In a notebook or on a piece of paper, for each SSI risk, list one or more improvement activity you would undertake to prevent SSI, plus 2–3 facilitators and 2–3 barriers.
Doing this activity will help you in planning projects that reduce SSI at your facility. You may want to refer to the previous section to ensure your ideas and plans are focused on one or more of the evidence-based recommendations for SSI prevention.
-
Hand Hygiene (10 min)
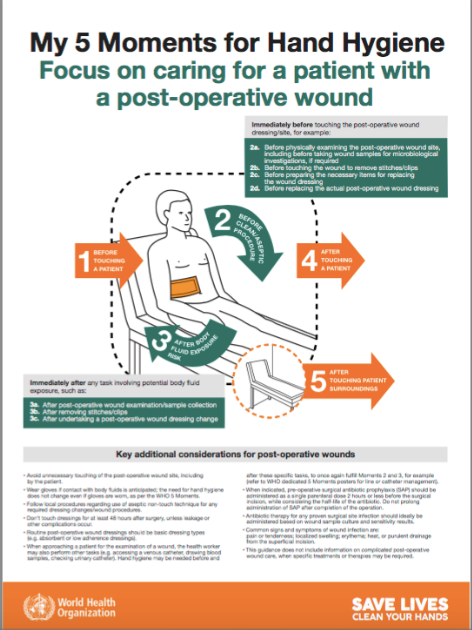
Here is an example of how to use a multimodal improvement strategy to reduce SSI—integrating proper hand hygiene (both regular hand hygiene and surgical hand preparation) into the surgical patient’s journey. Many of these examples are available on the Resources page.
Click or tap on each strategy to learn about what activities could be taken and what resources are available from WHO to perform these activities.
Build it
For system change, you might make sure there are adequate, reliable supplies of ABHR, and antimicrobial and plain soap, water, and clean towels, and that these are conveniently located according to their use (e.g., ABHR at the point of care; antimicrobial soap and ABHR in the scrubbing room). Depending on your situation, you may need to consider whether ABHR is even available. The SUSP study section includes modified formulations for surgical hand preparation and other tools (including surveys) you can use to assess and ensure reliable supplies.
Teach it
Several resources are available for staff education on hand hygiene. You can use updated slides for training sessions. One possible activity would be to use an infographic when training staff. For example, you could blank out some of the steps, then ask clinical staff where they think the moments for hand hygiene occur, or about other facts related to surgery.
Another way of engaging the surgical team in improving surgical hand preparation is to show them a video like this one:
Check it
To monitor whether staff are reliably performing surgical hand preparation, you can use a checklist, observe how closely they follow it, and provide feedback. For example, you could use this form to monitor whether staff are performing surgical hand preparation appropriately. This form, which is available in the Resources section, has a box dedicated to surgical hand preparation, and instructions on the back. The WHO SSI perioperative data collection form is an important tool for measuring adherence, which will improve patient outcomes and reduce SSI.
Sell it
Another strategy is to create posters and other tools to raise awareness of hand hygiene. These posters could include reminders about steps in surgical hand preparation, or creating awareness of the importance of hand hygiene. You could also post the infographic from the Teach it tab. Posters are just one way to communicate a message (and to support education). It is important to place these visual aids in prominent places, and to put new ones up periodically.

Live it
Technical tools alone will not help you address key organizational barriers that arise. The Agency for Healthcare Research and Quality (AHRQ) has created some adaptive tools that provide a useful start in addressing the institutional safety climate and culture, which is key to supporting a hand hygiene improvement effort. These tools can help a facility to identify both organizational and individual barriers; use them to enhance teamwork over time. It is important they are adopted and implemented from the outset of an improvement programme to create the awareness that missing hand hygiene action hampers patient safety, to help teams reflect on the local safety culture, and motivate them to engage in improving hand hygiene. These tools are available in the Resources section:
- Perioperative staff safety assessment tool
- A hospital survey on patient safety
- Learning from defects—perioperative setting
- Executive safety rounds kickoff template
- Understand the science of safety video
-
Surgical Hand Preparation (10 min)
Now that you have learned about using the multimodal strategy for hand hygiene improvement among surgical staff, let us review with a case study. Imagine the following scenario at your facility:
Not all surgeons are performing the recommended surgical hand preparation. After reviewing SSI data collection forms, you suspect that this is what could be causing SSI in patients. One of the problems you identify is a lack of products available for performing surgical hand preparation. In a notebook or on a piece of paper, list 2-3 activities your could take under each multimodal strategy component (build it, teach it, check it, sell it, live it) to ensure the improvement you want to see can happen successfully. When you are done with this exercise, click or tap on the compare answer button to see an expert's answer.
-
SSI Improvement Activities at Your Facility (10 min)
Pick one of the improvement activities you identified at the beginning of this section that you might implement to prevent SSI at your facility. On a piece of paper on in a notebook, for each multimodal strategy element (build it, teach it, check it, sell it, live it), list 2–3 activities that could help make this project successful. Here are some questions to think about as you do this activity:
- Does your facility need to procure, produce, identify, allocate, or prepare for the improvement?
- Depending on the activity selected, do you know where to deploy resources within the facility, including when the improvement is taking longer than expected?
- Does the facility have staff who are competent in delivering targeted training?
- Do you have the right materials to deliver the required training, and know which staff need to be trained?
- How can you ensure staff attend the training sessions?
- Has the system change been made so that the training delivered is realistic for the setting? For example, if you are training on use of negative-pressure devices, the actual devices need to be available for use.
- Is there, or is it possible to have, a valid and reliable surveillance system in place to collect data applicable to your setting (and based on published SSI definitions)? Are there resources to support this in your facility or at regional/national level?
- Does your facility have staff who are competent in undertaking monitoring and feedback?
- Which staff need to be trained to ensure effective monitoring and feedback?
- Are there forums where feedback can be delivered?
- Is your organization prepared to receive feedback and act on it?
- Which staff would benefit from reminders? Where is the best place to post these reminders?
- Do you have the right expertise and resources to develop effective communications?
- How will you engage leaders and frontline staff?
-
Summary (5 min)
In this last section of the SSI module, you learned about ways you can successfully implement prevention measures in your facility to reduce SSI. This section covered adaptive and technical approaches to improvement, and how to incorporate the WHO multimodal strategy in your interventions. You also learned about the SUSP and how it has been used in various countries to reduce SSI rates.
-
References
- Allegranzi B, Aiken AM, Kubilay Z, Nthumba P, Barasa J, Okumu G, et al. A multimodal infection control and patient safety intervention to reduce surgical site infections in Africa: a multicentre, before-after cohort study. Lancet Infect Dis. 2018 May;18(5):507-515. doi: 10.1016/S1473-3099(18)30107-5. Epub 2018 Mar. 5.
