Prevention Measures
In the first section of this module, you learned about the global burden of SSI and what you can do to learn about the incidence of SSI in your own facility or country. This section will cover risk factors for SSI, and prevention measures you can take to reduce SSI.
Learning Objectives
By the end of this module, you will be able to:
- list the risk factors that contribute to determine SSI,
- explain the content of the WHO SSI prevention recommendations, and
- understand the evidence supporting the recommendations.
Learning Activities
-
Lucian (5 min)
Lucian is anxious because he is going into hospital for surgery. A smoker for 30 years, Lucian has tried unsuccessfully to stop smoking. He is also a bit overweight. During preoperative preparation he is told that the surgery may take several hours, and that he may need a blood transfusion. The surgery team informs Lucian that he will have a postoperative wound site that may require care for a while.
In this unit, you will learn about how Lucian’s surgery team can understand common SSI risk factors, and how to prevent or minimize the risk of SSI.
Take a moment to think about what your facility is doing well in preventing SSI.
-
Risk Factors (10 min)
In the previous section, we discussed the importance of understanding the burden of SSI. Let us now look at what causes SSI. Often, SSI is the result of a lack of:
- understanding the frequency and burden of the problem
- awareness of what safe processes (effective prevention measures) are
- adherence to safe processes
- a culture of safety
Before we learn about prevention measures, let us go over the factors that increase the risk of SSI. Take a few minutes to brainstorm some risk factors for SSI. In the boxes below, list as many risk factors as you can think of for each topic, then click or tap the compare answer button to see an expert’s answer.
The risk of infection is lower when when minimally invasive surgery is required; it increases when the skin or mucous membranes are more extensively broken, or when a foreign object either is implanted or enters the patient’s body.
any object originating outside of the body -
How SSI Occurs (5 min)
How we manage the patient and the entire surgical environment is critical to preventing potential pathogens from entering the surgical site. Remember, a pathogen is a bacterium, virus, or other microorganism that can cause disease. An infection occurs when the pathogen enters the body, increases in number, and damages tissues. Surgical incisions and devices such as IV catheters can provide entryways for microorganisms to gain access to a susceptible host.
The sources of pathogens are both the patients themselves and external sources:
- endogenous flora: the patient’s skin, mucous membranes, and hollow viscera
- exogenous organisms: air in the operating room; the surfaces of surgical equipment, implants, and gloves/hands; and medications administered during operative procedures
Pathogens might gain access via routes of entry including hands, equipment, intravenous tubes, air (e.g., contaminated air and dust due to inadequate ventilation and cleaning), and the surgical patient environment/experience (e.g., skin preparation, including hair removal; intraoperative temperature affecting the patient’s body temperature). When thinking about the operating room, we can visualize where endogenous and exogenous flora will arise.
For example:
Endogenous infections: Patient’s own microflora (e.g., S. aureus from nasal carriage)
Staff in the operating room: Staphylococci from nasal carriage, skin on hand, and forearm via contact with punctured gloves or wet gown
Environmental source: Contaminated air and dust due to inadequate ventilation and cleaning
If you need to refresh your memory about transmission of disease, review the Introduction to IPC module.
-
Expert Considerations Regarding Recommendations (5 min)
WHO guidelines have recommendations for SSI prevention to protect patients from both endogenous and exogenous microorganisms. These recommendations come from evidence and expert consensus, including experience in different countries. They take into consideration the effectiveness of preventive measures, any harm that such measures may cause, the views of patients and professionals, and the resource implications of implementing the recommendations.
There are two types of recommendations. Click or tap on each tab to read more about them.
Strong
An expert panel has concluded that the benefits of these recommendations outweigh the risks. They consider the recommendations to be adaptable for implementation in most (if not all) situations. Patients should receive the interventions as the standard course of action.
Conditional
The benefits of these recommendations probably outweigh the risks. Experts agree that a more structured decision-making process should be undertaken locally, following stakeholder consultation and with involvement of both patients and health care professionals.
Read more about the methods behind the Global Guidelines for the Prevention of Surgical Site Infection.
You can read more about the methods behind the Global Guidelines for the Prevention of Surgical Site Infection in the Resources section.
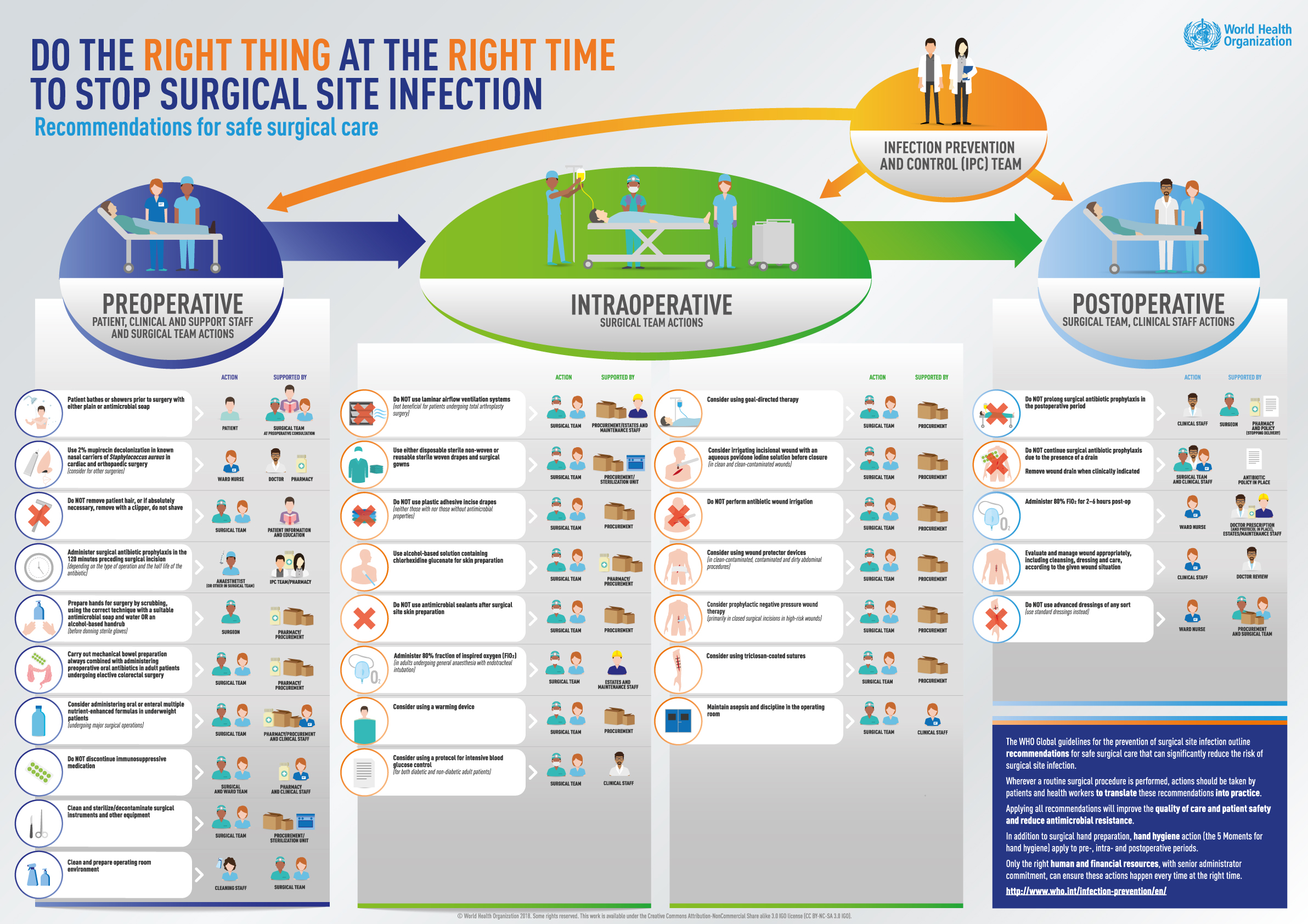
Different factors affect SSI prevention at different times. The recommended prevention measures cover the patient’s journey before, during, and after surgery. Part of the success of these measures hinges on practices adopted and internalized by surgical staff so that they are routinely and automatically performed, as well as being supported by the right culture and available resources within the health care organization.
-
The WHO Recommendations (5 min)
Now that you know more about how they were developed and categorized, here is a list of these recommendations. All the strong recommendations will be discussed in detail in this section. Click or tap on each tab to read the WHO recommendations.
Strong Recommendations Action Supported By 
Use 2% mupirocin deconolonization in known nasal carriers of Staphylococcus aureus in cardiac and orthopaedic surgery
(consider for other surgeries)Ward nurse Doctor, pharmacy 
Do NOT remove patient hair, or if absolutely necessary, remove with a clipper, do not shave Surgical team Patient information and education 
Administer surgical antibiotic prophylaxis in the 120 minutes preceding surgical incision
(depending on the type of operation and the half life of the anibiotic)Anathesthetist (or other in surgical team) IPC team/pharmacy 
Prepare hands for surgery by scrubbing, using the correct technique with a suitable antimicrobial soap and water OR an alcohol-based handrub
(before donning sterile gloves)Surgeon Pharmacy/procurement 
Carry out mechanical bowel preparation always combined with administering preoperative oral anibiotics in adults patients undergoing elective colorectal surgery Surgical team Pharmacy/procurement Conditional Recommendations Action Supported By 
Patient bathes or showeres prior to surgery with either plain or antimicrobial soap Patient Surgical team 
Consider administering oral or enteral multiple nutrient-enhanced formulas in underweight patients
(undergoing major surgical operations)Surgical team Pharmacy/procurement and clinical staff 
Do NOT discontinue immunosuppressive medication Surgical and ward team Pharmacy and clinical staff 
Clean and sterilize/decontaminate surgical instruments and other equipment Surgical team Procurement/sterilization unit 
Clean and prepare operating room environment Cleaning staff Surgical team Strong Recommendations Action Supported By 
Use alcohol-based solution containing chlorhexidine gluconate for skin preparation Surgical team Pharmacy/procurement Conditional Recommendations Action Supported By 
Do NOT use laminar airflow ventilation systems
(not beneficial for patients undergoing total anthroplasty surgery)Surgical team Procurement/estates and maintenance staff 
Use either disposable sterile non-woven or reusable sterile woven drapes and surgical gowns Surgical team Procurement/sterilization unit 
Do NOT us plastic adhesive incise drapes
(neither those with nor those without antimicrobial properties)Surgical team Procurement 
Do NOT use antimicrobial sealants after surgical site skin preparation Surgical team Procurement 
Consider using a warming device Surgical team Procurement 
Consider using a protocol for intensive blood glucose control
(for both diabetic and non-diabetic adult patients)Surgical team Clinical staff 
Consider using goal-directed therapy Surgical team Procurement 
Consider irrigating incisional wound with an aqueous povidone iodine solution before closure
(in clean and clean-contaminated wounds)Surgical team Procurement 
Do NOT perform antibiotic wound irrigation Surgical team Procurement 
Consider using wound protector devices
(in clean-contaminated and dirty abdominal procedures)Surgical team Procurement 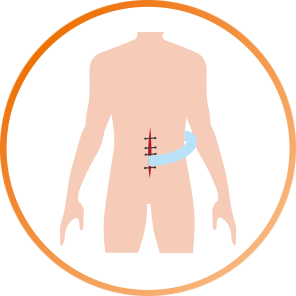
Consider prophylactic negative pressure wound therapy
(primarily in closed surgical incisions in high-risk wounds)Surgical team Clinical staff 
Consider using tricosan-coated sutures Surgical team Clinical staff 
Administer 80% fraction of inspired oxygen (FiO2)
(in adults undergoing general anaesthesia with endotracheal intubation)Surgical team Estates and maintenance staff 
Maintain asepsis and discipline in the operating room Surgical team Clinical staff Strong Recommendations Action Supported By 
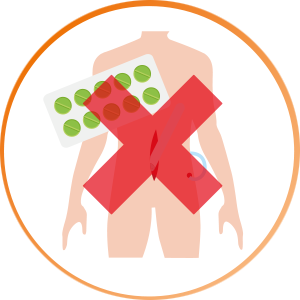
Do NOT prolong surgical anitbiotic prophylaxis in the postoperative period Clinical staff Surgeon, pharmacy and policy (stopping delivery) Conditional Recommendations Action Supported By 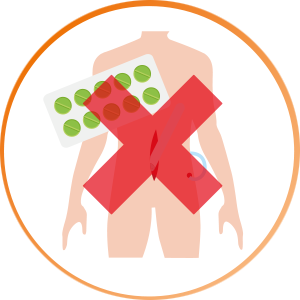
Do NOT continue surgical antibiotic prophylaxis due to the presence of a drain. Remove wound drain when clinically indicated
Surgical team and clinical staff Antibiotic policy in place 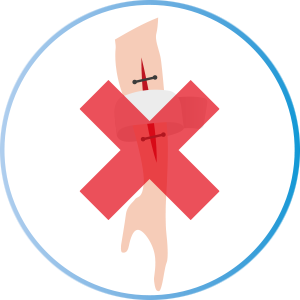
Do NOT use advanced dressings of any sort (use standard dressings instead) Ward nurse Procurement and surgical team 
Administer 80% FiO2 for 2-6 hours post-op Surgical team Doctor prescription (and protocol in place), estates/maintenance staff 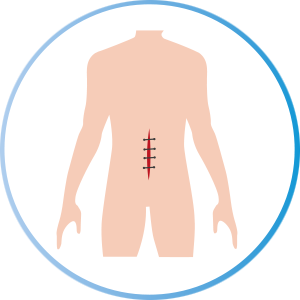
Evaluate and manage wound appropriately, including cleansing, dressing and care, according to the given wound situation Clinical staff Doctor review The next several learning activities will cover some of these recommendations in more depth. Strong recommendations will appear in orange boxes; conditional recommendations will be in blue boxes.
-
Treatment of S. aureus Nasal Carriers (5 min)
Strong recommendation: Patients undergoing cardiothoracic and orthopaedic surgery and who are known nasal carriers of S. aureus should receive perioperative intranasal applications of mupirocin 2% ointment, either alone or in combination with chlorhexidine gluconate (CHG) body wash.
This recommendation is not applicable to paediatric patients.
Along with this recommendation is a conditional recommendation that suggests that patients who are undergoing other types of surgery and who have S. aureus are also treated with mupirocin 2% ointment, either alone or in combination with CHG body wash.
As we saw in the first section, one of the most frequent causes of HAI worldwide is S. aureus, which is a known cause of postoperative wound infections. This pathogen imposes a high burden on the health system. Nasal carriage of S. aureus is a risk factor for subsequent infection in a patient; a large proportion of HAI due to S. aureus originates from the patient’s own flora. Mupirocin nasal ointment is considered a safe, cost-effective treatment to eradicate S. aureus nasal carriage and reduce rates of infection.
This recommendation is applicable to both pre- and perioperative periods. The usual application of 2% nasal mupirocin ointment is twice a day for five to seven days before surgery, or from the date of hospital admission to the day of surgery.
Involve patients by asking for their collaboration and compliance with this recommendation. For outpatients, provide clear instructions on how to correctly administer intranasal applications of mupirocin 2% ointment and, if advised locally, tell them to also perform a CHG body wash before the operation. CHG 2-4% soap body wash should be applied in combination with clean, running water. For inpatients, either provide the same instructions as for outpatients, or have clinical staff assist patients with these procedures.
It is important to investigate and document potential allergic reactions to mupirocin, and to record treatment information in patient records and surveillance monitoring forms.
Screening of patients for S. aureus carriage varies both between and within countries and is dependent on several factors, including cost-effectiveness and local epidemiology. This recommendation applies only to facilities where screening (nasal swabs sent to a laboratory) is feasible; it may not apply to settings with high prevalence of mupirocin resistance.
More information on this recommendation: Key facts on Decolonization of Nasal Carriers of Staphylococcus aureus
There is more information on this recommendation in Key Facts on Decolonization of Nasal Carriers of Staphylococcus Aureus in the Resources section.
-
Mechanical Bowel Preparation (MBP) and Preoperative Oral Antibiotics (5 min)
Strong recommendation: MBP alone (without the administration of oral antibiotics) should not be used with adult patients undergoing elective colorectal surgery.
Along with this recommendation is a conditional recommendation that suggests giving preoperative oral antibiotics combined with MBP to adult patients undergoing elective colorectal surgery.
Evidence has shown that preoperative MBP alone does not reduce SSI risk compared to not using MBP. However, some evidence has shown that preoperative MBP combined with oral antibiotics is effective in reducing SSI.
This recommendation applies to the preoperative period only, and should not be referred to as “selective digestive decontamination.”
Decisions about the type of MBP regimen, oral antibiotics, and the drug of choice for intravenous antibiotic prophylaxis should be based upon availability of medication, drug (antibiotic) resistance data, and the volume of surgical activity at your facility. The combination of drugs used should guarantee activity against both facultative gram-negative and anaerobic bacteria. In most studies that this recommendation is based on, oral aminoglycosides were combined with metronidazole or erythromycin.
-
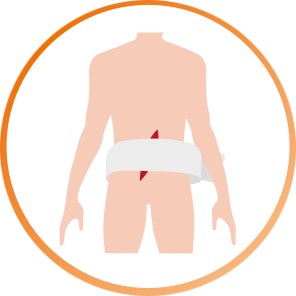
Hair Removal (5 min)
Strong recommendation: In patients undergoing any surgical procedure, hair should either not be removed or, if absolutely necessary, should only be removed with a clipper. Shaving is strongly discouraged preoperatively and in the operating room.
Removal of hair (by any method) has no benefit over no hair removal with respect to the incidence of postoperative infection. Furthermore, the incidence of SSI is higher when shaving with a razor than with clippers because shaving with a razor causes small abrasions to the skin. If hair must be removed (because the presence of hair will interfere with the operation), it should be done in the operating room immediately before surgery, using an electric clipper with a single-use head. If single-use disposable clippers are not available, clean and decontaminate clippers after each use before using them on another patient.
Evidence shows that use of depilatory creams has no benefit, and does not lower SSI risk compared with shaving. In addition, sometimes these creams produce hypersensitivity reactions. Therefore, WHO does not recommend their use.
Because of cultural norms, women may prefer shaving in the genital area before surgery; some may even come to the hospital having already shaved. To avoid this, explain to patients that hair removal, whether by shaving with a razor or any other method, increases the risk of SSI.
See the Key Facts on Patient Bathing and Hair Removal fact sheet for more information on this recommendation.
See the Key Facts on Patient Bathing and Hair Removal fact sheet in the Resources section for more information on this recommendation.
-
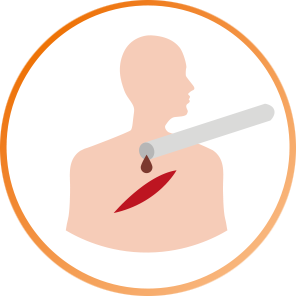
Surgical Antibiotic Prophylaxis (SAP) Timing (5 min)
Strong recommendation: SAP should be administered before the surgical incision, when indicated. In particular it should be administered within 120 minutes before incision, depending on the half-life of the antibiotic (closer to incision time for antibiotics with short half-life).
Administering SAP at the right time is critical to ensuring that there is adequate concentration of the drug at the incision site at the start of the operation (when risk of surgical site contamination is highest). Incorrect timing (more than 120 minutes before the incision, or after the incision) can lead to increased risk of SSI. Having the right type of antibiotic for the procedure and knowing the patient’s history helps destroy the bacteria most frequently found at the operation site, while also protecting the patient.
It is important to have the right antibiotic concentration at the operation site throughout the entire operation. Correct use of SAP is important not only to prevent SSI, but also to avoid the emergence of antimicrobial resistant pathogens that can cause more serious disease to the patient. See the Global Action Plan on Antimicrobial Resistance for more information.
It is important to have the right antibiotic concentration at the operation site throughout the entire operation. Correct use of SAP is important not only to prevent SSI, but also to avoid the emergence of antimicrobial resistant pathogens that can cause more serious disease to the patient. See the Global Action Plan for Antimicrobial Resistance in the Resources section for more information.
You may not be directly involved in adapting this recommendation to your facility, but you should make sure that those with anaesthesia, microbiology, and pharmacy expertise are part of the decision-making and prescribing processes. A list of SAP Timing Considerations.
You may not be directly involved in adapting this recommendation to your facility, but you should make sure that those with anaesthesia, microbiology, and pharmacy expertise are part of the decision-making and prescribing processes. A list of considerations for SAP timing can be found in the Resources section.
-
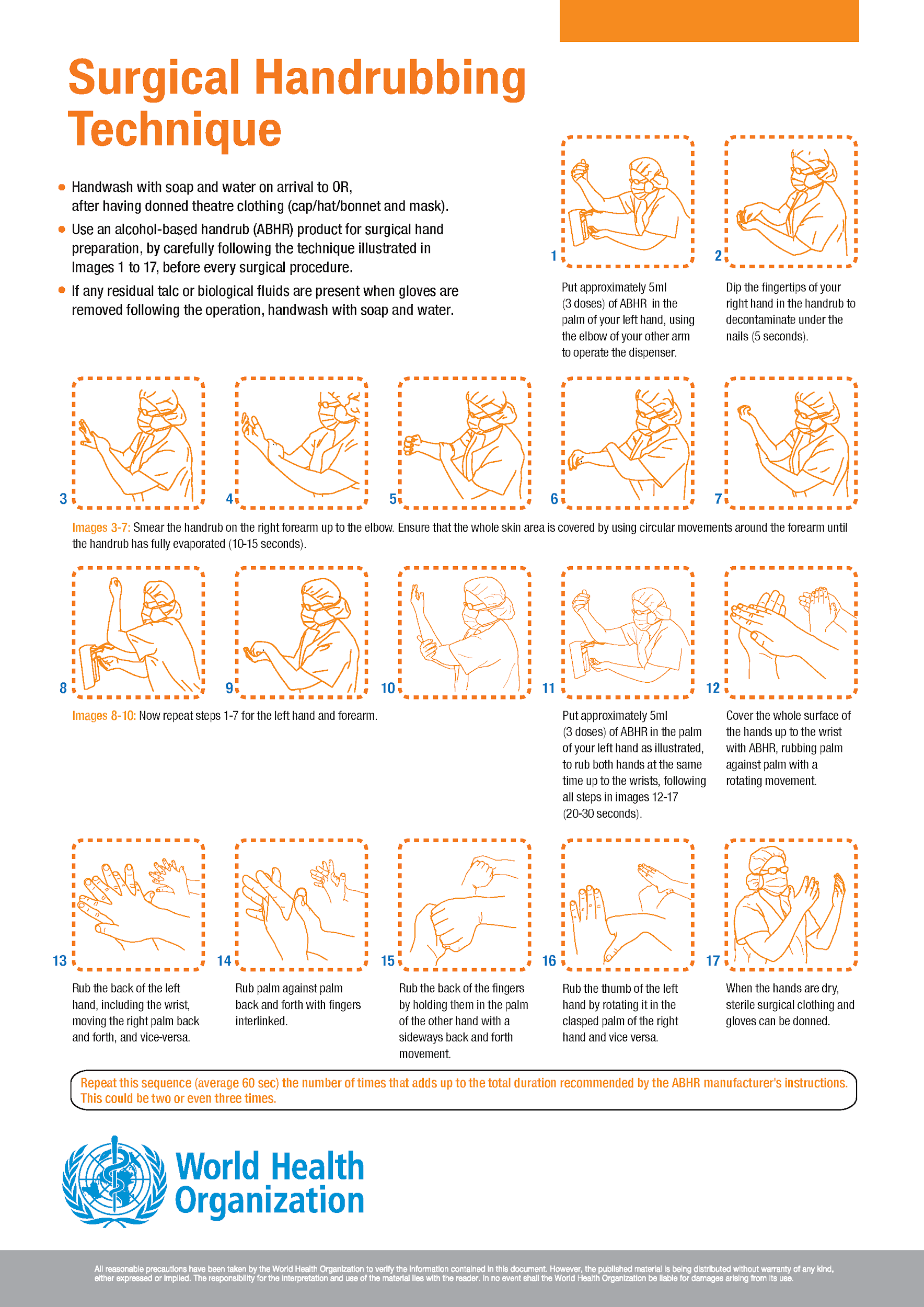
Surgical Hand Preparation (5 min)
Strong recommendation: Surgical hand preparation should be performed either by scrubbing with a suitable antimicrobial soap and water, or by using a suitable alcohol-based handrub (ABHR) before donning sterile gloves.
The hands of the surgical team should be clean upon entering the operating room. It is vitally important to maintain the lowest possible contamination of the surgical field. Even when sterile gloves are worn, punctures to the gloves can occur. Proper hand preparation reduces the transfer of skin bacteria from the surgical team’s hands to the open wound. Thus, appropriate surgical hand preparation is strongly recommended. Evidence shows that use of either ABHR or antimicrobial soap and water are equally effective.
Surgical hand preparation should eliminate transient flora and reduce resident flora. Click or tap on each type of preparation to learn more about it.
Surgical hand preparation
Surgical hand preparation refers to an antiseptic handwash or handrub performed preoperatively by the surgical team, using a specific technique for a specified duration, to eliminate transient flora and reduce resident skin flora. Such antiseptics often have persistent antimicrobial activity.
Surgical handrubbing
Surgical handrubbing refers to surgical hand preparation with a waterless, alcohol-based handrub.
Surgical handscrubbing/presurgical scrub
Surgical handscrubbing/presurgical scrub refers to surgical hand preparation with antimicrobial soap and water.
Once in the operating area, WHO indicates repeating surgical scrubbing or handrubbing without prior handwashing before switching to the next procedure.
Surgical handscrub and handrub with ABHR should not be combined sequentially, as skin irritation can occur. ABHR can be produced locally if necessary (how to do this is described in the next section).
If you need to refresh your memory about proper hand hygiene, refer to the Hand Hygiene unit of the Standard Precautions module.
The use of alcohol-based products for hand hygiene by patients or health care workers who may object for religious reasons has been addressed in the WHO guidelines on hand hygiene in health care. Cultural and religious leaders have provided supporting statements about the use of alcohol for this purpose.
-
Knowledge Check (10 min)
-
Surgical Skin Site Preparation (5 min)
Strong recommendation: Alcohol-based antiseptic solutions based on CHG should be used for surgical site skin preparation on patients undergoing surgical procedures.
This measure reduces the microbial load on the patient’s skin as much as possible before incision. Alcohol-based CHG is more effective than alcohol-based povidone-iodine in reducing SSI rates. The next section has information about producing alcohol/CHG-based skin preparation solutions at your facility.
Intact skin preparation should be done in the operating room prior to making the incision. In the operating room, position the patient to avoid movement after skin preparation, but be mindful of the skin that might be prone to breakdown from the pressure of being in one position for too long. Protect yourself and other health workers against splashing by wearing gloves. Be sure to change your gloves once the skin preparation is complete. Ensure that skin preparation is not removed or washed off before draping.
The effectiveness of this recommendation is not proven for paediatric patients. Alcohol-based solutions should not come into contact with mucosa or eyes, and should not be used on neonates. Ensure that surgical and ward staff are aware that CHG can cause skin irritation.
The use of alcohol-based products on patients or health workers who may object for religious reasons has been addressed in the WHO guidelines on hand hygiene in health care. Cultural and religious leaders have provided supporting statements about the use of alcohol for this purpose.
-
Surgical Skin Site Preparation (5 min)
Watch this video about surgical skin site preparation and respond to the questions below.
See the >Key Facts on Surgical Site Skin Preparation fact sheet for more information on this recommendation.
See the Key Facts on Surgical Site Skin Preparation fact sheet in the Resources section for more information on this recommendation.
-
SAP Prolongation (5 min)
Strong recommendation: SAP administration should not be prolonged after the operation has been completed.
Evidence shows that prolonged use of SAP postoperatively has no benefit over a single preoperative dose in reducing SSI after surgery (with intraoperative redosing if necessary). Discontinuation of SAP after surgery avoids unnecessary extra costs, potential side effects, and emergence of antimicrobial-resistant pathogens. In fact, continuing SAP postoperatively increases the risk of Clostridium difficile infection.
SAP should not be confused with antibiotic treatment, which should be given only when an SSI or another infection is proven or suspected (patient displaying signs and symptoms and ideally, based on wound sample culture and sensitivity).
-
Conditional Recommendations (5 min)
Consider WHO’s conditional recommendations as part of SSI prevention guidelines or improvement plans. Some of these recommendations cover important best practices, such as patient bathing before surgery. These recommendations are usually conditional because, although evidence proving their effectiveness to reduce SSI exists, it is not as strong as the evidence for strong recommendations. Their adoption may also depend on other local considerations. These conditional recommendations for SSI prevention are listed below. You can find more details here: Conditional Recommendations
Consider WHO’s conditional recommendations as part of SSI prevention guidelines or improvement plans. Some of these recommendations cover important best practices, such as patient bathing before surgery. These recommendations are usually conditional because, although evidence proving their effectiveness to reduce SSI exists, it is not as strong as the evidence for strong recommendations. Their adoption may also depend on other local considerations. These conditional recommendations for SSI prevention are listed below. You can find more details in the WHO guidelines in the Resources section.
Preoperative

Preoperative bathing Patient bathes or showeres prior to surgery with either plain or antimicrobial soap.

Decolonisation of S. aureus Consider treating patients with known nasal carriage of S. aureus who are undergoing other types of surgery with perioperative intranasal applications of mupirocin 2% ointment, either alone or in combination with CHG body wash.

Nutritional support Consider administering oral or enteral multiple nutrient-enhanced formulas in underweight patients
(undergoing major surgical operations)
Immunosuppressive agents Do NOT discontinue immunosuppressive medication.
Intraoperative

Laminar flow ventilation Do NOT use laminar airflow ventilation systems
(not beneficial for patients undergoing total anthroplasty surgery)
Drapes and gowns Use either disposable sterile non-woven or reusable sterile woven drapes and surgical gowns.

Plastic adhesive drapes Do NOT us plastic adhesive incise drapes
(neither those with nor those without antimicrobial properties)
Antimicrobial skin sealants Do NOT use antimicrobial sealants after surgical site skin preparation.

Warming devices Consider using a warming device.

Blood glucose control Consider using a protocol for intensive blood glucose control
(for both diabetic and non-diabetic adult patients)
Fluid therapy Consider using goal-directed therapy.
Incisional wound irrigation Consider irrigating incisional wound with an aqueous povidone iodine solution before closure
(in clean and clean-contaminated wounds)
Antibiotic wound irrigation Do not perform antibiotic wound irrigation.
Wound protectors Consider using wound protector devices
(in clean-contaminated and dirty abdominal procedures)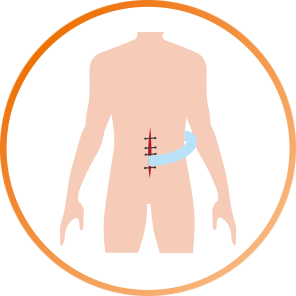
Coated sutures Consider prophylactic negative pressure wound therapy
(primarily in closed surgical incisions in high-risk wounds)
80% fraction of inspired oxygen Administer 80% fraction of inspired oxygen (FiO2)
(in adults undergoing general anaesthesia with endotracheal intubation)Postoperative
Wound drains Do NOT continue surgical antibiotic prophylaxis due to the presence of a drain.
Remove wound drain when clinically indicated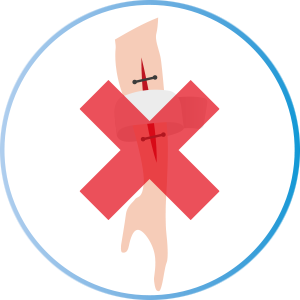
Advanced dressings Do NOT use advanced dressings of any sort
(use standard dressings instead)
80% fraction of inspired oxygen Administer 80% fraction of inspired oxygen (FiO2)
(in adults undergoing general anaesthesia with endotracheal intubation)For more information: Conditional Recommendations
For more information on the studies behind these conditional recommendations, see the Resources section.
-
Other Prevention Measures (10 min)
In addition to the strong and conditional recommendations included in the WHO evidence-based guidelines, there are other important prevention measures to consider when creating an SSI prevention plan. These include sterilization and decontamination, and environmental cleaning.
These topics are covered in more detail in other modules.
Sterilization and Decontamination
The WHO guide Decontamination and Reprocessing of Medical Devices for Health-care Facilities can aid you in addressing this important area of SSI prevention. Use this document when creating your plan, paying particular attention to:
The WHO guide Decontamination and Reprocessing of Medical Devices for Health-Care Facilities (see the Resources section for this document) can aid you in addressing this important area of SSI prevention. Use this document when creating your plan, paying particular attention to:
- Risk management
- Having a sterile services department
- Cleaning of medical devices
- Preparation and packaging equipment for reprocessing
- Chemical disinfectants
- Decontamination of endoscopes
- Sterilization of reusable medical devices
- Eliminating reuse of single-use medical devices
- Transporting medical devices
- Dental practice
Key messages
Do not soak instruments used in the operating room in disinfectant before the recommended decontamination process, as this may cause corrosion or other damage. The disinfectant may be inactivated by blood and body fluids, which could then lead to microbial contamination and the formation of biofilm. Soaking may also contribute to the development of antimicrobial resistance to disinfectants. Transporting equipment soaked in disinfectant may pose a risk to health care workers, and result in improper handling of, and accidental damage to, the equipment. Standard operating procedures for sterilization and decontamination are important.
Environmental Cleaning
In the operating room, hand-touch surfaces and surfaces that may have come in contact with patient blood or body fluids should be wiped clean first by using a detergent solution, and then disinfected according to hospital policy and allowed to dry. This figure shows an example of where to clean before and after each surgery.
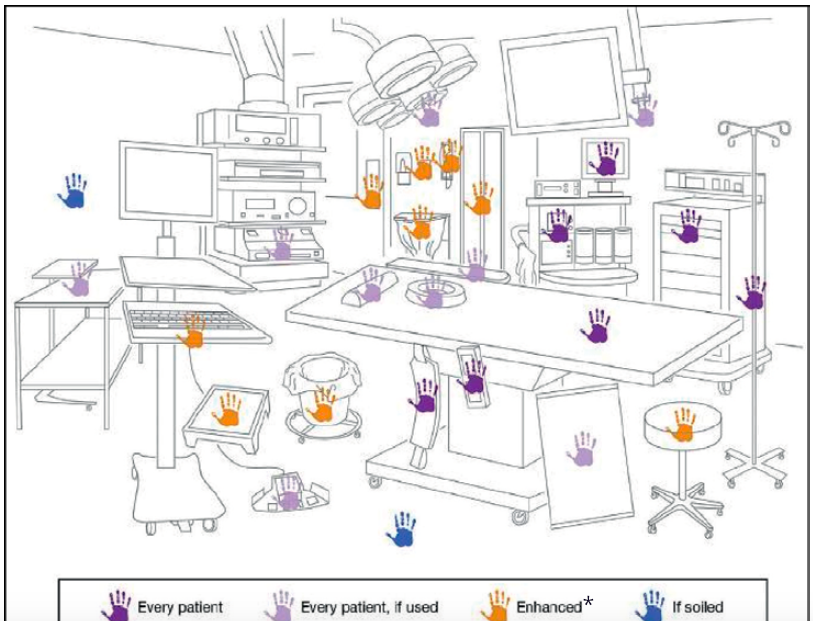
*Enhanced=appropriate disinfectant should be used to decontaminate these surfaces, after thorough cleaning with a detergent.
Click or tap on each surface type to learn about the recommended approach for cleaning and disinfection.
High hand-touch surface
This refers to any surface that frequently comes into contact with hands. These surfaces require special attention and more frequent cleaning. After thorough cleaning with a detergent, consider the use of appropriate disinfectants to decontaminate these surfaces.
Minimal-touch surface
These surfaces (such as floors, walls, ceilings, window sills) have minimal contact with hands. They are not in close contact with either the patient or their immediate surroundings. Clean these surfaces on a regular basis with detergent only, or when soiling or spills occur.
Key messages
Clean starting from the least soiled areas to most soiled areas (clean to dirty) so that microorganisms in the most soiled areas are not carried to less dirty areas. Cleaning should be performed from ceilings, walls, and other high areas to low areas (high to low), so that dust and other debris generated while cleaning falls to the floor.
It is important to discard items that cannot be decontaminated effectively. For example, if an item is torn, either discard it or find a way to resolve the problem, such as covering the bed with a plastic sheet until a replacement can be found.

For surfaces contaminated with blood and body fluids, be sure to wear appropriate personal protective equipment (PPE). Contain the spill using absorbent material (cloth, paper, etc.), and remove the materials as soon as possible. Clean with detergent and then disinfect the surface. Dispose of cleaning materials in a dedicated medical-waste container.
Be sure that cleaning staff are properly trained and wear appropriate PPE.
To review environmental cleaning recommendations, see the Environmental Cleaning module.
-
Knowledge Check (5 min)
-
Postoperative Wound Care (10 min)
Appropriate postoperative wound care is also crucial to reducing SSI risk, and should be part of your SSI prevention plan. This section does not cover wound healing and management in detail, but instead will highlight key considerations about postoperative wound management as part of the surgical patient journey.
Patients play an active role in wound healing, such as getting good nutrition to help maintain healthy skin and tissue. They should be discouraged from touching the wound site.
Routine postoperative wound dressings should use standard dressing types (e.g., absorbent or low-adherence dressings). It is not necessary to use any type of advanced dressing as it is not evidence-based and carries additional costs; a standard dressing is appropriate for a primary closed surgical wound.
Wear gloves if contact with body fluids is anticipated during wound management. Hand hygiene is critical for wound care; the need for hand hygiene action as per the 5 Moments for Hand Hygiene does not change even if gloves are worn.
Wear gloves if contact with body fluids is anticipated during wound management. Hand hygiene is critical for wound care; the need for hand hygiene action as per the 5 Moments for Hand Hygiene does not change even if gloves are worn per the WHO 5 Moments for Hand Hygiene (see Resources section for the poster on the 5 Moments for Hand Hygiene).
Postoperative Evaluation
When conducting wound assessment on a patient, the patient should be made comfortable and receive pain relief if necessary prior to dressing removal. Check patient notes for relevant information, such as medical condition and date of expected dressing removal.
Staff should avoid unnecessary touching of the postoperative wound site. After about 48 hours check the wound (perform dressing removal unless otherwise indicated); if it is dry and healing with no signs of infection, no additional dressing is required and the patient can shower as normal. If signs of infection are noted, a doctor/wound specialist should be consulted. A specimen sample may be necessary.
Common signs and symptoms of wound infection are pain or tenderness, localized swelling, erythema, and heat or purulent drainage from the superficial incision.
Do not continue administration of SAP after completion of the operation; if signs and symptoms of SSI are suspected, the decision to establish antibiotic therapy should be made by a doctor. Ideally, antibiotic therapy should be administered based on wound sample culture and sensitivity results.
Some health facilities have wound assessment forms that prompt for evaluation, such as doing a visual check, comparing and evaluating any smells, assessing the amount of blood or ooze (excretions) and their colour, and documenting the size of the wound if it is not healing. This approach is very useful.
Wounds may not always heal normally. In this case, the wound must be managed to ensure the best outcome. The process of wound assessment, cleansing, and care must suit the patient’s needs and limit additional infection risk, since there is a risk of introducing infection to a postoperative wound.
If a wound is not healed after the patient is discharged, it is vital to communicate to community/outpatient clinic health workers about how to manage the situation, including the process of ongoing wound assessment, cleansing, and care to suit the patient’s needs and limit further infection risk.
Dressing Removal
A decision should be made as to whether the dressing change will use a non-touch or full aseptic technique; this will determine the type of gloves to wear. For closed surgical wounds with no signs of complication, it is acceptable to remove the surgical wound dressing using a non-touch technique while wearing nonsterile gloves. Follow local procedures regarding use of aseptic non-touch technique for any required dressing changes/wound procedures.
Regardless of technique, gather all clean/sterile items before starting the wound assessment/dressing procedure. In some countries, premade packs containing all items needed for wound dressing removal/wound cleaning are available.
Hand Hygiene
Knowing when hand hygiene is necessary helps protect the patient and surgical wound from contamination that can lead to infection, even in the postoperative period. Practicing the 5 Moments for Hand Hygiene consistently and reliably ensures that both patients and health workers are protected from potential pathogens when care is being provided. If the flow of care is disrupted in daily routines (for example, if an item needed for dressing removal is forgotten or a nurse is called to do something else while removing a wound dressing), the 5 Moments indicate when to perform hand hygiene to ensure clean hands at the right times. Click or tap on each arrow to read about how the 5 Moments for Hand Hygiene apply to caring for a patient with a postoperative wound.
Knowing when hand hygiene is necessary helps protect the patient and surgical wound from contamination that can lead to infection, even in the postoperative period. Practicing the 5 Moments for Hand Hygiene consistently and reliably ensures that both patients and health workers are protected from potential pathogens when care is being provided. If the flow of care is disrupted in daily routines (for example, if an item needed for dressing removal is forgotten or a nurse is called to do something else while removing a wound dressing), the 5 Moments indicate when to perform hand hygiene to ensure clean hands at the right times. Click or tap on each arrow to read about how the 5 Moments for Hand Hygiene apply to caring for a patient with a postoperative wound.
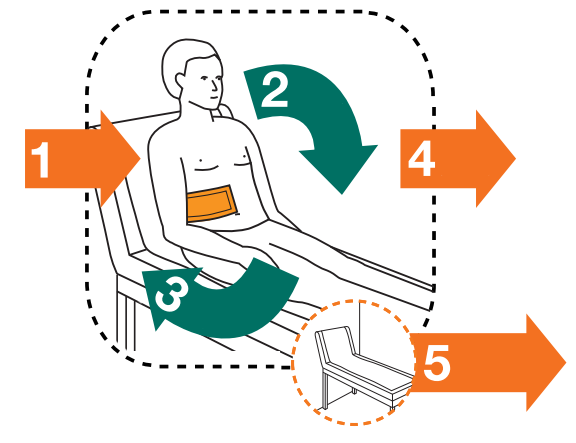
Before touching a patient.
Before clean/aseptic procedure
Immediately before touching the postoperative wound dressing/site. Examples include:
- Before preparing the necessary items for replacing the wound dressing
- Before physically examining the postoperative wound site, including before taking wound samples for microbiological investigations, if required
- Before touching the wound to remove stitches/clips
- Before replacing the actual postoperative wound dressing
After body fluid exposure risk
Immediately after any task involving potential body fluid exposure, such as:
- After postoperative wound examination/sample collection
- After removing stitches/clips
- After undertaking a postoperative wound dressing change
After touching a patient
After touching patient surroundings
-
Wound Management (10 min)
Watch this video on wound management.
-
In Your Setting (15 min)
Take a few minutes to think about the following questions:
- Do you have SSI prevention guidelines at your facility?
- If you have your own guidelines, how do they compare to the WHO recommendations? How can you make sure that that the key WHO standards for SSI prevention are included in your guidelines?
- If you do not have your own guidelines, how would you present the WHO recommendations in your facility?
- What is currently the most challenging recommendation to include in your guidelines or to implement?
-
Resource Considerations (5 min)
In some countries it may be challenging to implement some of the recommendations and other suggestions for SSI prevention, but that should not deter facilities from starting to implement those that are feasible. The cost of SSI prevention is lower than the cost of high SSI rates to the health care system. Many of the recommendation statements recommend not taking an action, which can save resources. However, it can still be a challenge to get people to change something they routinely do. In the next section we will discuss activities that will help overcome some of the challenges listed below.
Here are some factors that may cause challenges in implementing interventions to reduce SSI:
- Lack of availability of mupirocin, antimicrobial soap, ABHR, CHG, SAP, oxygen, and their related costs, which could place a financial burden on both the facility and its patients
- Poor technical laboratory capacity and other facility infrastructure (water, sanitation, and hygiene)
- High workload and a lack of organizational commitment, particularly with respect to required written procedures/instructions
- Need for staff training and specific expertise (e.g., increased oxygenation, glucose control)
-
Recommendations and AMR (5 min)
AMR is a global problem that requires input from everyone at all health care levels in order to preserve the effectiveness of antibiotics and stop their misuse. Four of the WHO SSI prevention recommendations specifically aim to improve antibiotic use in surgical services.
- Time SAP optimally: intravenous SAP should be administered prior to the surgical incision when indicated (depending on the type of operation). Given the half-life of antibiotics, SAP should be administered no more than 120 minutes before the incision (advice from microbiologists and pharmacists supports this decision).
- Do not irrigate a wound with antibiotics.
- Do not use antibiotic prophylaxis due to the presence of a postoperative wound drain.
- Do not continue SAP during the postoperative period.
-
Summary (5 min)
You have just learned about risk factors for SSI, and how SSI occurs. The section then described WHO recommendations (a number of which address AMR). All of the recommendations—both strong and conditional—are important, although the latter should be considered locally. Other prevention measures discussed included decontamination and sterilization procedures, and environmental cleaning. Finally, you learned about postoperative wound management.