Health-Care Associated Infection Surveillance Part 3
In this last part of the Health-Care Associated Infection (HAI) Surveillance module we will cover the remaining steps of conducting surveillance: communication, feedback and evaluation. You will learn how to prepare reports for different audiences and be able to identify who should know what information.
HAI surveillance systems should have a built-in, regular process for evaluation of their management, efficiency and impact. This process should include evaluation of whether interventions are successful and the surveillance programme itself needs any adjustments.
Learning Objectives
By the end of this module, you will be able to:
- prepare a report for HAI surveillance;
- identify how to communicate surveillance information to various groups;
- describe objectives and elements of HAI surveillance evaluation; and
- describe the need for continuous improvement of surveillance systems.
Learning Activities Estimated time:
-
Newsha’s Story Part 3 (5 min)
In the previous Surveillance module, the infection prevention and control (IPC) surveillance multidisciplinary team (which is a consolidated group with a mission now!) headed by Newsha discovered that infants may be acquiring methicillin resistant Staphylococcus aureus (MRSA) in the gynaecology ward run by Professor Dastaviz. The team brings the results directly to the hospital director. They ask for advice and support to convince Professor Dastaviz and his staff about the urgent need for performing HAI surveillance and implementing an IPC monitoring and improvement programme. On top of HAI surveillance, they want to monitor processes: they propose to use observational tools to measure hand hygiene, staffing levels, distance between beds, water, sanitation and hygiene (WASH) facilities and hygiene during deliveries. “More than 150 years since Semmelweis discovered infection transmission in a gynaecology ward in Vienna, we cannot accept that women deliver their babies in an unsafe environment!” Newsha firmly declared.
-
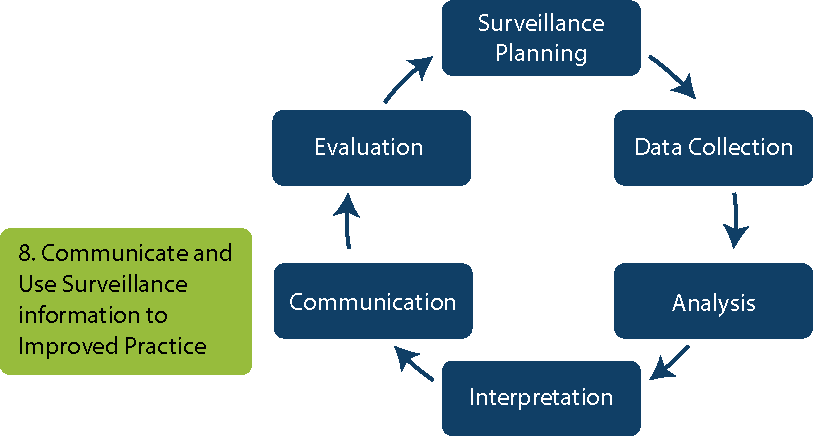
Step 8: Communication (5 min)
In this module, we will discuss the remaining two steps in the HAI surveillance process: communication and evaluation.
First, we will talk about how to prepare and communicate the data analysed and interpreted (data analysis and interpretation were covered in previous parts). To promote change, it is important to give feedback to the people whose behaviours you want to modify. Therefore, it is crucial to identify the appropriate audience and tailor the information you have learned from the surveillance data. “The demonstrable power of surveillance is in sharing findings with those who need to know and who can act on the findings to improve patient safety.”2
Then, we will talk about evaluating the surveillance system.
-
Preparing Reports (5 min)
Before drafting surveillance reports, it is important to identify who the recipients will be. Managers can use findings to identify and implement evidence-based IPC practices and improve outcomes. Health care workers (HCWs) can change their behaviour to provide better patient care, so it is essential that they be included and receive feedback.
IPC teams can use surveillance information to create awareness about defective behaviours and launch and inform prevention measures; management can use reports to gain additional support from senior executives.
When creating a surveillance report, be sure to include the following items:
- identify the author and date of the report;
- state the purpose for conducting surveillance;
- define the event, population, setting and period studied;
- state the criteria used for defining a case (i.e., the case definition);
- explain the methodology used to identify cases;
- identify which statistical methods and calculations were used;
- specify the results (e.g., the number of cases/events identified, the number of the population studied);
- interpret the findings in a way that the target audience will easily understand; and
- describe any actions taken and make prevention and control recommendations.
Your surveillance reports should be user-friendly and provide accurate, interpretable information that can lead to improvement. Displaying the data visually (e.g., line lists, graphs, charts, tables) may help the audience more easily understand the report. The report can be incorporated into formal or informal improvement efforts.
Sometimes there is pressure to underreport the number of cases so that a ward or facility appears to have lower rates of HAI, especially if targets are not being met. For most malpractice events, it is important to review and address the issue, outline the lessons learned and take steps to improve the system (rather than punish the person).
Be sure to use caution when submitting or interpreting surveillance data that will be used for external or inter-facility comparisons. These data are sensitive because they can determine the closure of a health care facility or the firing of a ward or medical manager, have political and societal implications, and produce media headlines such as “Hell Hospital of Death!”
-
Targeting Communication to Different Audiences (5 min)
Different people will have different levels of interest—some will need an extensive report, and some will need to know only a few key facts. When communicating to any key stakeholder, make sure you are:
- timely (otherwise the results will become obsolete);
- targeted (a full epidemiological analysis with many graphs will not likely be useful for some audiences, such as policy makers);
- systematic (regularly create and share reports); and
- specific.
Communication of surveillance information should be regular and systematic. Be sure to hold regular meetings to share results from surveillance data. Have direct discussions with individual HCWs to provide feedback. Another example of sharing information is using large printed or handwritten wallcharts in wards/theatres displaying monthly infection rates.
Communication should be targeted to those who can change current practices. Click or tap on the tabs to read about how, what and when to communicate.
Hospital staff
When communicating HAI surveillance findings to hospital staff, be sure to include senior staff. The following information should be included:
- a general view of the risk of HAI
- the current HAI situation and the impact on patient safety and costs
- changes in practice that can reduce risk of infection.
Specific patient areas
When communicating with staff in specific patient areas, include detailed analysis of specific types of infections. Let the report serve as a basis for discussion or use it to evaluate and plan interventions. Use a standard format with visual aids that display trends and make sure the report is clear and well organized.
Detecting outbreaks
Timely communication of alerts to health care providers is important because it is an opportunity to remind staff of IPC practices (e.g., hand hygiene and routine MRSA screening). Be sure to outline additional IPC precautions that should be taken in response to the outbreak. Present only key information using graphs and charts and focus on main messages and the impact of the outbreak on patient outcomes.
Surveillance data can be used to raise awareness of HAI. It quantifies the burden of HAI and describes the circumstances under which they occur. These data can also be used to provide feedback to HCWs, and motivate staff, administrators and policy makers to improve IPC practices. Finally, surveillance data can help evaluate interventions, such as educational campaigns on hand hygiene.
-
Knowledge Check (5 min)
-
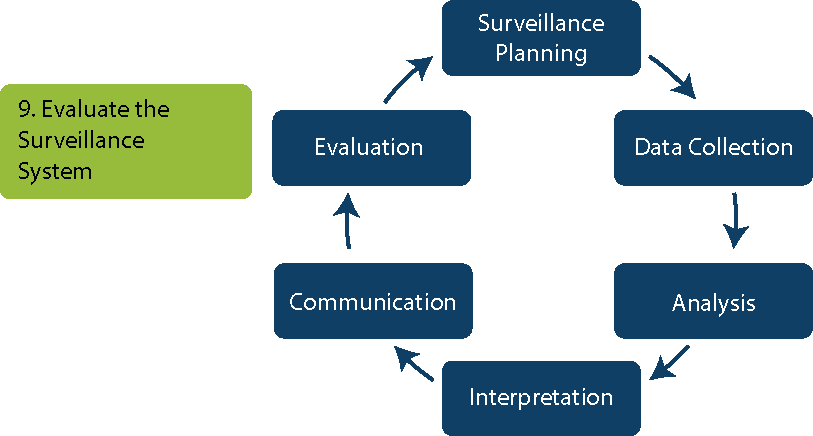
Step 9: Evaluation (5 min)
The last step in the HAI surveillance process is evaluation.
A HAI surveillance system should have a built-in, regular process for evaluation. As part of IPC committee meetings, regularly review case definitions, case finding methods (including number of potential cases missed) and other surveillance procedures to ensure standardization. At least annually, review surveillance objectives (and revise if needed).
The committee should also use the evaluation process to identify ways to improve surveillance in the facility. The surveillance system should undergo continual modification to ensure it is working towards improved IPC. Modifications to the surveillance system might include:
- reassessment of the infections monitored
- changes to the approach to case finding
- ways in which information is generated
- a change in objectives.
Internal or external reviewers can provide a helpful perspective and may be able to suggest new ideas to improve surveillance.
When evaluating the surveillance system and processes, be sure to:
- measure the completeness and representativeness of the system by calculating its sensitivity and specificity (we will cover this more in the next reading);
- review the checks in the system to assure data quality;
- assess how efficiently/effectively the surveillance system works (process evaluation); and
- assess how information is used to reduce HAI risk (outcome evaluation).
-
Sensitivity, Specificity and Validation (5 min)
Let us take a moment to discuss key elements of surveillance evaluation, namely: sensitivity, specificity and validation. You should know what these terms mean and how they are calculated, even if you will not be doing the calculations yourself.
Sensitivity is the ability to correctly include infections that are present (that is, the number of HAI that are correctly diagnosed). Here is the calculation:
Sensitivity=Number of true positive infections detected Number of true positives + False negatives detected by that methodSpecificity is the ability to correctly exclude infections that are not present (that is, the number of patients who do not have HAI). Here is the calculation:
Specificity=Number of true negative infections detected Number of true negatives + False positives detected by that methodSome data collection software will calculate sensitivity and specificity for you.
A validation study will determine sensitivity and specificity. A separate investigator audits ongoing surveillance, comparing the results with the reported cases. The investigator assesses the validity (false positives—specificity, false negatives—sensitivity), reliability (agreement, kappa) and inter-country comparability of the data collected.
Here is an example of a validation required by the European Centre for Disease Prevention and Control (ECDC) in the European Union. All participating countries are expected to perform validation to assess the reliability and comparability of data collection when performing a point prevalence survey (PPS).1 The validation must be done:
- at the same time as a national or regional PPS
- by a national/regional PPS validation team
- on a minimum sample of 5 hospitals and 250 patients
- on a recommended sample of 25 hospitals and 750 patients.
-
Evaluation Questions (5 min)
When evaluating a surveillance system, there are a few essential questions to ask.
- Is the methodology appropriate for the specific surveillance? Is it periodically evaluated and validated?
- Are data managed by qualified personnel? Is their quality and accuracy periodically evaluated and validated?
- Are appropriate statistical methods used for the analysis and when comparing data?
- Is information technology being used in data management?
- Are processes in place to regularly review data quality, including assessment of:
- case report forms
- integration of clinical microbiology results
- data accuracy
- denominator determination (i.e., total exposed population)
- Is supportive supervision or another related mentorship practice in place?
- Did the surveillance programme accomplish the following?
- detect HAI or other events in a timely manner
- identify trends signalling changes
- detect outbreaks and clusters of infections
- identify risk factors associated with HAI infection
- provide an estimate of the magnitude of the event
- assess the effectiveness of prevention and control efforts
- How is the surveillance system impacting IPC?
- How is the information produced from surveillance being used to reduce HAI in the health care setting?
- Did the surveillance system detect clusters or outbreaks?
- Which patient care practices were changed based on surveillance data?
- Were data used to make procedural changes to decrease the rate of infection and control outbreaks (if any)?
-
Knowledge Check (5 min)
-
Summary (5 min)
In this part of the module, you learnt about the last two steps in the surveillance process, which are communication and evaluation. Communicating the surveillance data to different stakeholders can raise awareness of HAI and motivate HCWs to change their behaviour and improve IPC practices.
The last step, evaluation, looks at not just evaluating interventions to reduce HAI, but also the surveillance programme itself to determine if any changes need to be made.
-
References
- European Centre for Disease Prevention and Control. Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals ECDC PPS validation protocol version 3.1.2. Stockholm: ECDC; 2019 Jan. doi: 10.2900/444036.
- Lee TB, Montgomery OG, Marx J, Olmsted RN, Scheckler WE; Association for Professionals in Infection Control and Epidemiology. Recommended practices for surveillance: Association for Professionals in Infection Control and Epidemiology (APIC), Inc. Am J Infect Control, 2007 Sep;35(7):427 40. doi: 10.1016/j.ajic.2007.07.002. PubMed PMID 17765554.