Module 7: Introduction to Interoperability at the Facility Level
Welcome to the module Introduction to Interoperability at the Facility Level. This is a beginning-level module meant for frontline healthcare workers, facility managers, and anyone interacting with health information systems. In this module, you will learn about the concept of interoperability with a focus on the facility perspective. We will cover what interoperability is, how it can be applied at the facility level, common concerns about patient data security, and basic maintenance of interoperable systems.
Learning Objectives
After taking this module, you’ll be able to:
- Define key interoperability terms: Interoperability, semantic interoperability, syntactic interoperability,
- Describe three different kinds of interoperability (human-intervened, point-to-point, standardized)
- Explain the importance of interoperability in the overall health information system
- Describe different applications of interoperability
- Outline three tactics for maintaining data security
- Describe three approaches to maintaining interoperable systems
Attributions
The description of the Bahmni project in this module comes from the presentation, “Experiences with Implementing Technologies and an Overview of Systems Integration”, by Craig Appl, used with permission under a Creative Commons Attribution 3.0 United States License.
The examples in the section “Levels of Interoperability” are adapted from “Three levels of health information technology interoperability” and “Semantic Interoperability”, by Doron Gutkind, posted January 2, 2015. www.lintechsoftware.com
DHIS2 examples are adapted from the DHIS2 website, section “In Action”: www.dhis2.org/
Learning Activities
Part 1: What is Interoperability
-
Activity: What is interoperability (10 min)
Imagine trying to get from one part of your country to a small village at the opposite end of it. You may drive or take an airplane most of the way. You may have to cross a river by boat. It is almost guaranteed that you will need to take multiple roads and byways to reach your destination. A major paved road will connect to a smaller gravel road, which may connect to a foot path in order to reach the small village.
Just as a single road cannot connect all destinations, one IT system cannot solve all problems. In the domain of healthcare, we build specialized systems to solve multiple problems. For example, a Laboratory Information System (LIS) has a specific set of problems that are not applicable to the Electronic Medical Record System (EMR), even though there is some overlap.
Instructions: Click or tap the four icons on the image to reveal additional information about how interoperability works. Then, continue to read the information below the image.
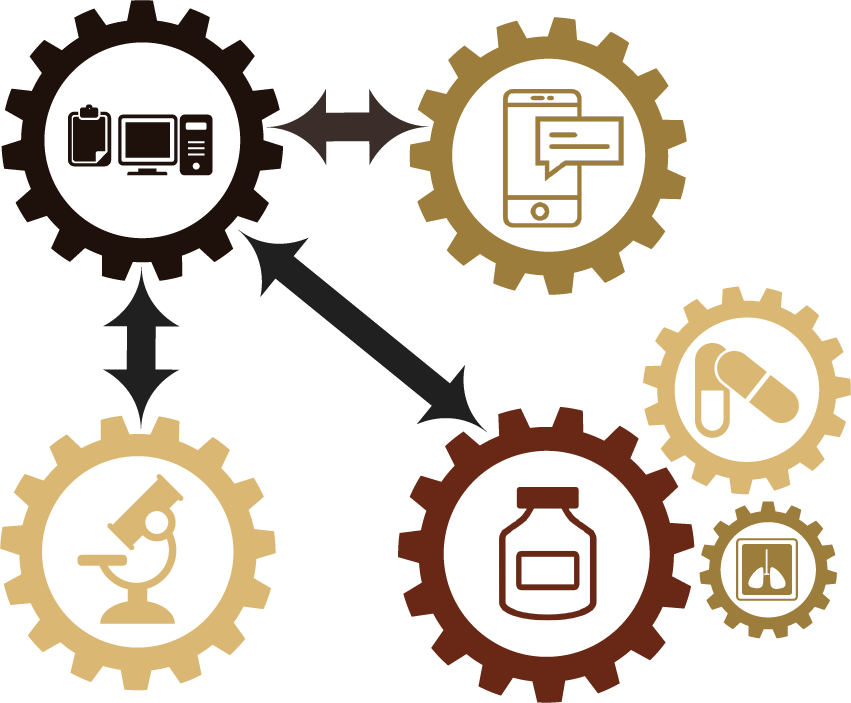
EMR System
An EMR can generate a lab order, but the EMR will not track that order as it’s processed through the lab. The lab should track that independently with their own information system.
Health Care Workers in the Field
The clinic’s EMR doesn’t need to manage the local community health worker team, but the data collected by the community health workers in the field should be available to a doctor if a local patient comes for a clinic visit.
Stock Management System
The stock management system isn’t responsible for tracking the patients that received vaccinations at the facility, but it needs to know how many vaccine doses are consumed so it can order more when there is an immunization clinic next month.
Laboratory System
A laboratory consumes reagents, but it should not be responsible for tracking the process of procuring those reagents. That should be the responsibility of the stock management system.
EMR System to Laboratory Information System
An EMR can exchange information with an LIS.
EMR System to Health Care Workers in the Field
A community health worker can access antenatal care records for a local family from her mobile.
EMR System to Stock Management System
A hospital’s clinicians can order and track laboratory and radiology tests and prescription information for their patients.
Interoperability is about connecting systems, just like roads of differing size, importance, and materials connect to serve many locations. Interoperability allows each system to do what it does best and share with other systems so they can do what they do best.
These connections provide a great asset by streamlining information exchange and supporting more complete data available to the right person at the right time, but they are also a liability. A problem with one system might lead to vulnerability in any system connected to it. We assume that the benefits of interoperability outweigh the risk.
Instructions: Next, click or tap the three arrows on the image to reveal how these systems are interconnected.
-
Reading: Three kinds of interoperability (10 min)
There are three basic kinds of interoperability: Human-mediated, Point-to-Point, and Standardized. To better understand the different types of interoperability, let’s work through examples. Each interoperability kind includes three examples to enhance your understanding.
Instructions: Click or tap the three buttons to learn more about the different kind of interoperability.
Human-Mediated
Human-mediated interoperability can be thought of as information moving between systems, based on human interventions, such as data entry. Read three example to enhance this definition.
Instructions: Click or tap the example buttons to the left.
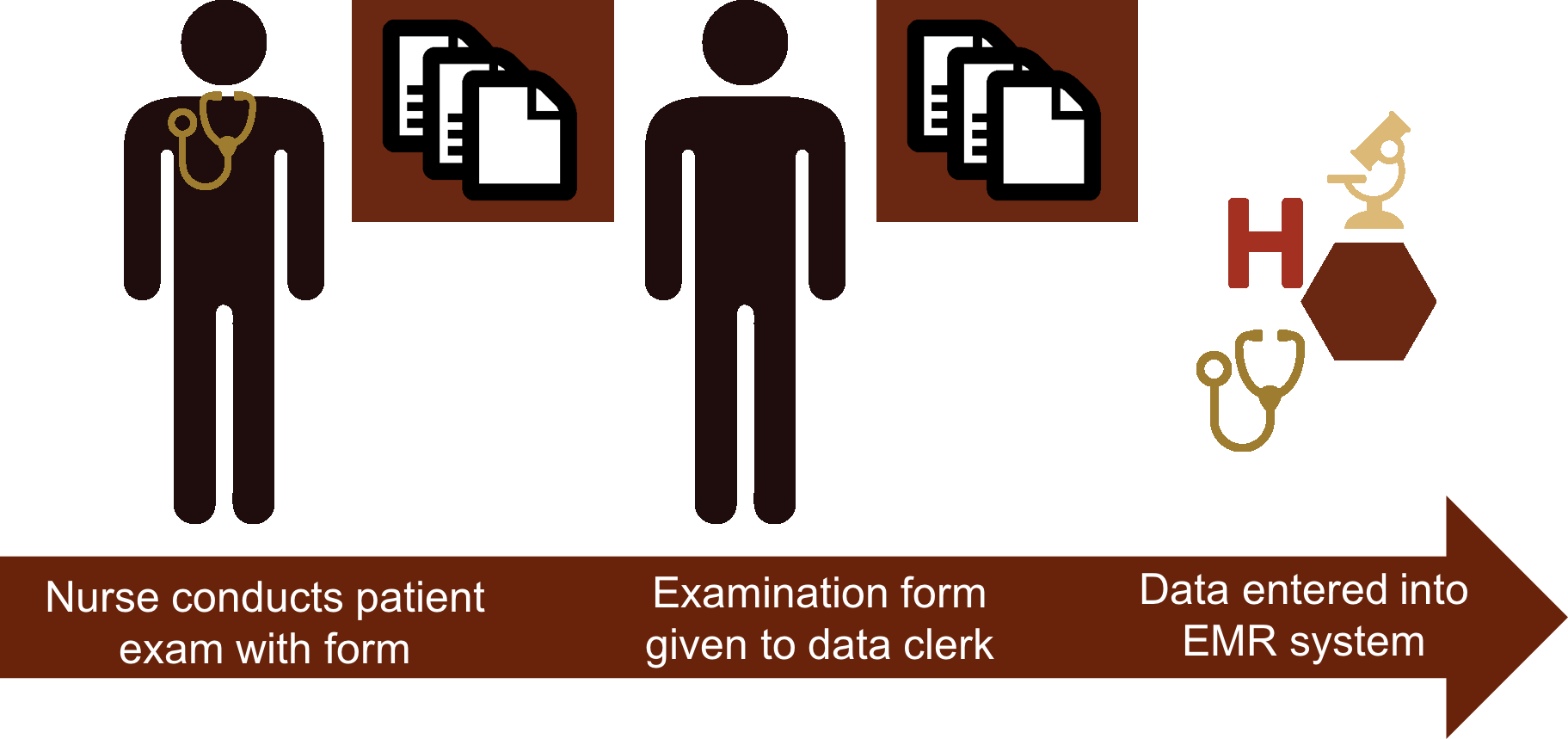
Example 1
Antony is a nurse at the regional hospital. During a patient examination, he takes notes on a paper form. At the end of the day, he sends all the examination forms to the data clerk, who enters the data in the hospital’s electronic medical record system.
This is interoperability between information systems at its most basic. The paper system—Antony’s paper forms—is interoperable with the electronic medical record. The data clerk is the human-mediated connection between the two systems.
Example 2
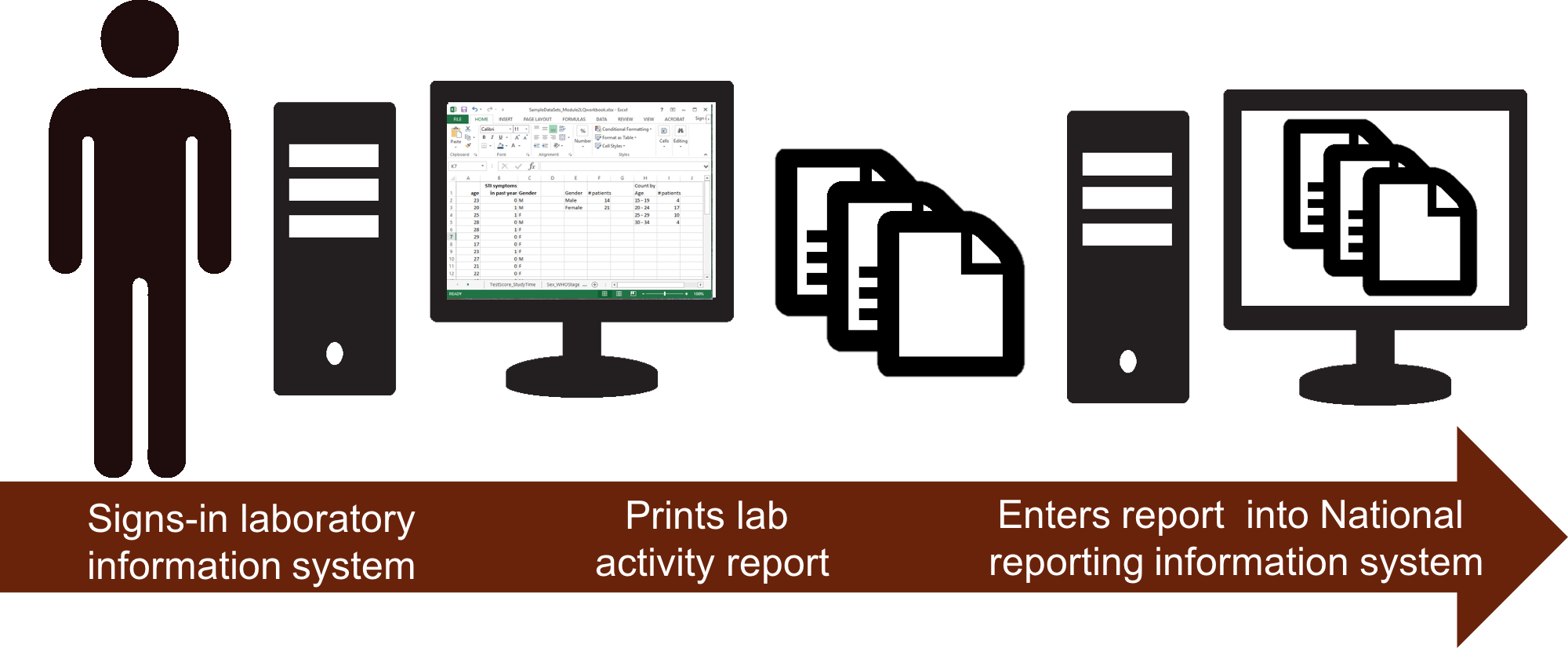
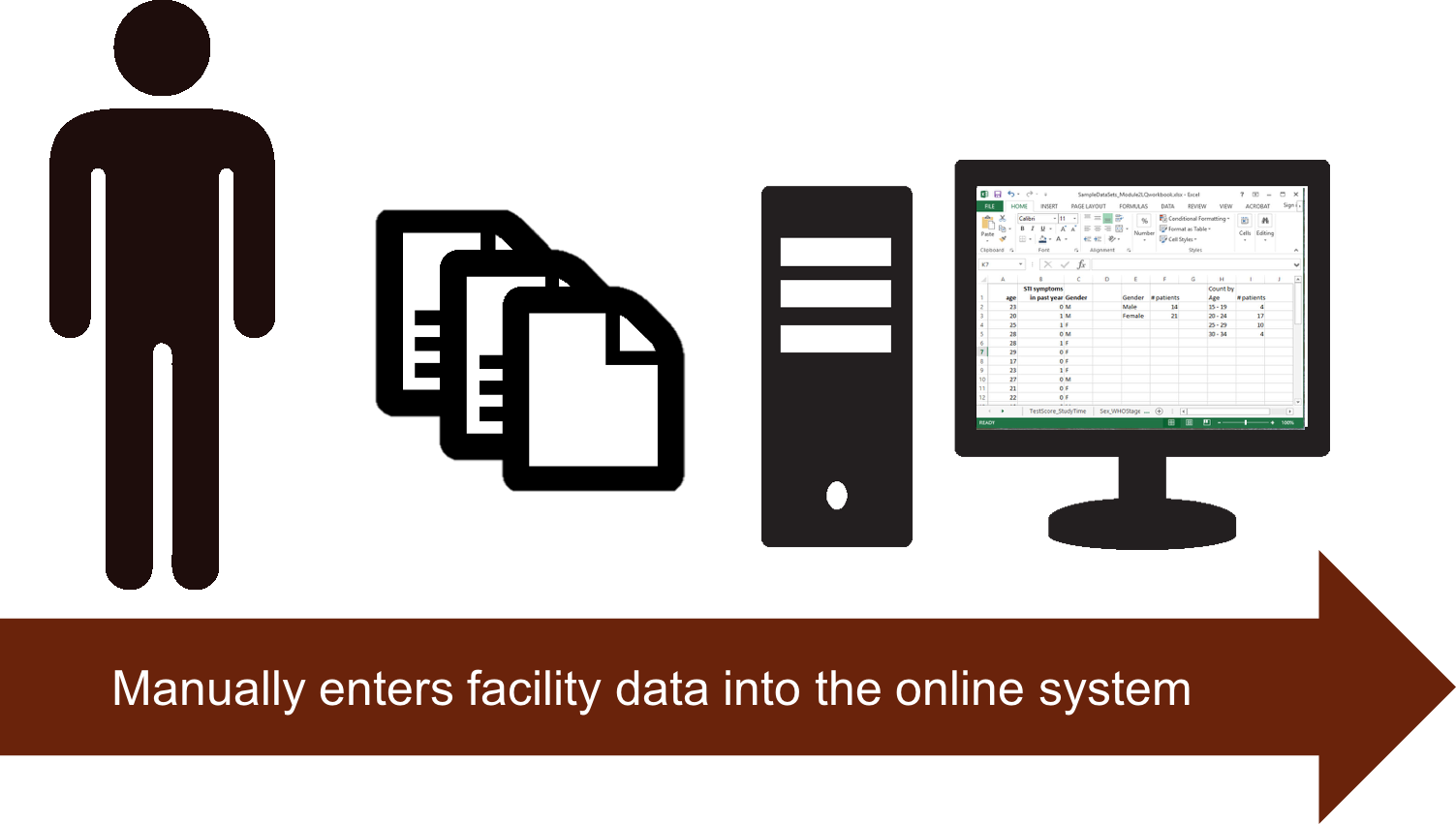
Let’s look at another example of human mediated interoperability.
Elisabeth is a manager at the district clinical laboratory. Each month, Elisabeth signs into the laboratory information system and prints out the lab activity report which gives the total number of HIV tests performed, along with their results, in an Excel-style spreadsheet. She then takes the printed report, opens the reporting software on the same computer, and enters the aggregate data into the reporting information system, which is based at the national level.
This procedure moves data from the lab system to the reporting system. A human, however, provides the connection between the two systems.
Point-to-Point or Exchange
Point-to-Point or Exchange interoperability means two or more systems can request and receive information from each other. The examples shown in this module involve a basic electronic movement or exchange of data between two systems. Now, read the three examples to enhance this definition.
Instructions: Click or tap the example buttons to the left.
Example 1
Thabiso, the data manager at Limpopo Anglican Hospital, receives a request for patient information from another hospital in the province. He generates the patient summary report from his hospital’s electronic medical record system. He then select the option to send the report electronically to the other hospital, which then uploads the report into their own record system using a specially-designed software feature. The systems have exchanged the patient information.
Example 2
Limpopo Anglican Hospital has an EMR. Its clinical laboratory also operates a Laboratory Information System (LIS). A physician can order a patient’s lab test from the EMR. Once the patient’s test results are recorded in the LIS, the system automatically send the report to the electronic medical record system. The lab results report appears in the patient chart automatically.
Example 3
Aggregate data from the health facility is collected by SMS on a mobile phone and sent from that system to DHIS2 because the end user can’t access the internet.
Standardized Interoperability
Standardized interoperability means two or more systems can exchange information that is usable without further transformation to the data within each system’s respective context. Read three examples to enhance this definition.
Instructions: Click or tap each example buttons to the left.
Example 1
A clinic’s reporting system aggregates the monthly reports and the user can click a button to automatically send the data to DHIS2.
This example uses the latest Aggregate Data Exchange Standard (ADX) that is being validated within HL7's FHIR standards. "The Aggregate Data Exchange (ADX) Profile enables interoperable public health reporting of aggregate health data. ADX will typically be used to represent routinely reported aggregate data such as the numerators and denominators which can be used in the construction of public health indicators."
(Source: http://wiki.ihe.net/index.php/Aggregate_Data_Exchange)Example 2
The real-life example of an integrated hospital information system in Nepal called Bahmni connects an EMR, a billing system, the laboratory and radiology departments, reporting to the national level, and a pharmacy management system. Updates occur for the system as a whole. The system permits seamless communication between each of the component systems.
Health standards are used in multiple workflows in this example. The EMR is able to integrate with the radiology department using PACS integration and the universal DICOM format to store and transmit images. In this integration, images are stored from the radiology devices, transmitted to the EMR and directly viewable by a provider through the DICOM viewer. Integrations with the laboratory and pharmacy include sending orders directly from the EMR to the laboratory or pharmacy. The orders are then filled by technicians in each department. In the case of the laboratory, the lab results are transmitted back to the EMR and support the clinician's decision to make a diagnosis. These messages use either HL7 standards or mature application programming interfaces to connect between these systems.
Example 3
Data sent automatically from the LIS triggers clinical decision support features in the patient record in the EMR.
This example utilizes health information exchange standards to return patient lab results to the EMR. However, there are other components of health care delivery that are being standardized through the decision support process. This example specifically includes triggering clinical decision support features in the patient record in the EMR. This process is defined by clearly reviewing and understanding common clinical actions when a particular lab result is returned. The software developers then build algorithms that surface in the user interface that can directly add value to the clinical encounter with the patient. This process of quality improvement aims to standardize one component of healthcare delivery at a time, injecting technology where appropriate.
-
Activity: Levels of Interoperability (15 min)
We have just seen three kinds of interoperability. These described the ways systems can be connected. Next, we will explore three levels of interoperability: or, how sophisticated the connection is. When considered together, the kind and level of interoperability give a clear picture of the scope and sophistication of an interoperable health information system network.
Levels of interoperability refers to the way in which you get information in two different systems to be understood.
Instructions: Click or tap each circle in the image to learn about the different levels and how to increase the capability of interoperation.
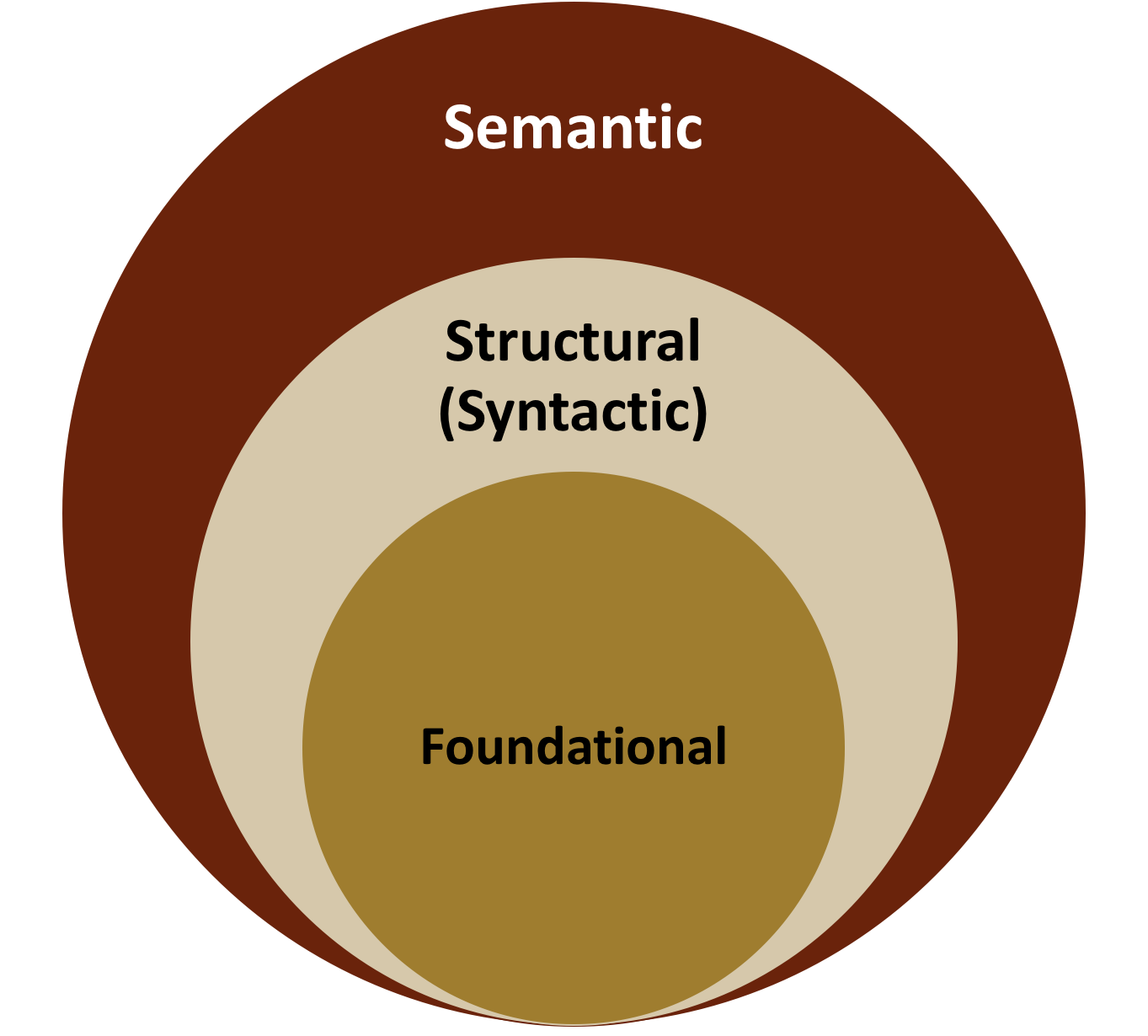
Foundational (most basic)
Also, called functional interoperability, this kind of interoperability simply means that data can be sent or exchanged from one system to another. The data moves from one system to the other through functional interoperability. However, even though the data moves, this level of interoperability does not address the issue of whether the data can be interpreted by the receiving system. The data moves, but without its context or meaning.
It is as if a friend sent you a letter. You receive the letter; however, the letter is in Wolof, a language you do not understand. You must translate the letter in order to understand it.
For example, a laboratory could electronically send test results in PDF format to the clinic using a secured messaging feature. Someone at the clinic can receive the results—in PDF form. However, that person would need to open the message, download the PDF attachment, read the document, understand its meaning, and communicate the information to appropriate care providers in order to make the information usable.
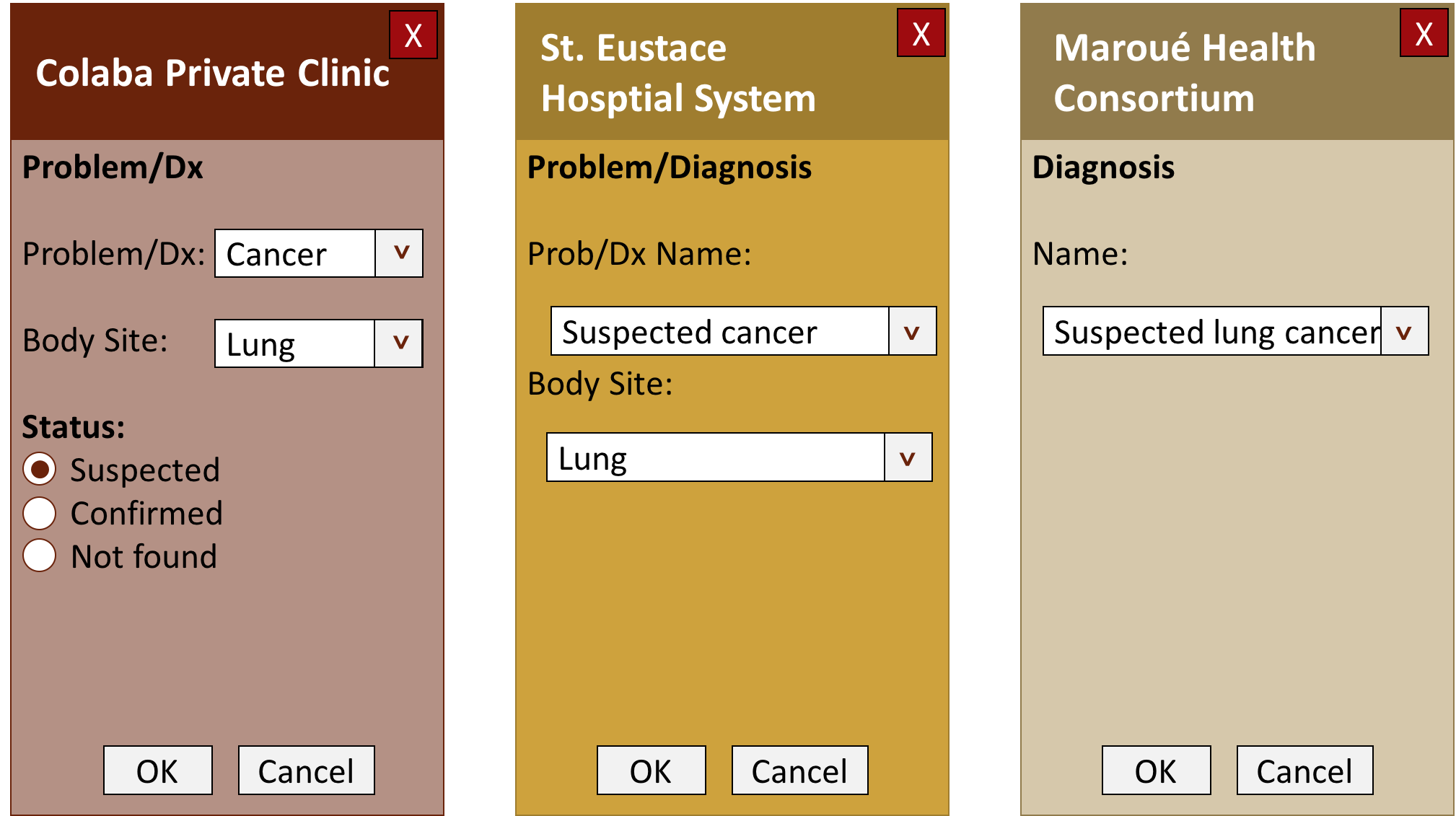
Level 2: Structural (intermediate)
Also called syntactic interoperability, this kind of interoperability preserves the original context and meaning of the data sent from one system to the other. It preserves this meaning because the data is exchanged with a standard structure or format that both the sending and receiving systems “understand”. The mutual understanding occurs at the level of the data field. They share the same syntax.
For example, a patient transfers into a clinic from a facility in another county that uses a different medical record system. The two medical record systems are structurally interoperable. While the patient chart in one has a field called “Main Complaint” and the other has a field called “Primary Complaint” the connection between the two systems recognizes that these two fields are the same in meaning. Therefore, when the patient’s record is transferred to the new facility, the receiving system can identify the correct fields in the old record and populate the new record with the transferred data.
Level 3: Semantic (most sophisticated)
The most advanced kind of interoperability is semantic interoperability. It means that two or more systems have the ability not just to send information, identify and match data, but also seamlessly permit each system to use data from the other systems. The systems must all be able to integrate and support overall workflow of information and tasks. To continue the previous example about a transferred record, the receiving system not only recognizes the data sent from the previous system and maps it into the new patient record, but the shared information can automatically trigger an alert about a pharmacy stock out of the patient’s medication at the new facility.
This kind of interoperability relies on codified standards to allow systems to exchange, interpret, and use information. HL7 standards for messaging, LOINC standards for laboratory vocabulary, and SNOMED standards for medical practice vocabulary are all standards that serve interoperability in the healthcare domain.
Semantic interoperability is the gold standard; however, it is difficult to achieve and requires the cooperation and collaboration of many stakeholders.
-
Activity: More Examples of Interoperable Systems (15 minutes)
Instructions: Click or tap the three buttons below to work through examples of interoperable and integrated systems. After you read each example, you will be asked two questions: what kind and what level of interoperability is described in the scenario.
DHIS2
Zambia, Tanzania, and Uganda have set up DHIS2 as a national data warehouse, with all healthcare facilities reporting into the system. This aggregate data is used by the Ministry of Health to track operations, monitor processes, and communicate with stakeholders. In Tanzania, DHIS2 is also used to for infectious disease surveillance; outbreaks and weekly summary data are collected directly from health facilities using a standard protocol (USSD, or unstructured supplementary service data) for cellular telephones to communicate with the mobile service provider's computers. In addition, Zambia and Uganda have set up related modules that link DHIS2 with mobile tools like ODK to collect facility- and community-level information via mobile phones and transmit the data to DHIS2 using SMS and other technologies. In Uganda, they are tracking mother-child continuum of care while in Zambia this is being used in a malaria eradication program. Outreach workers for the malaria eradication program report data into DHIS2 via their mobile phones and can access trend analysis charts and other reports.
What might be the advantages and drawbacks for your facility if it were to implement a project like the ones just described?
OpenSRP
In Bangladesh and Pakistan, a tool called OpenSRP is being adapted so that healthcare workers can use a mobile application on mobile phone or tablet to collect immunization and family planning data at the community level. This application has the potential to be connected to health facility electronic medical record systems to help provide seamless transitions in care and more complete patient records. The application could also be connected to a national data warehouse like DHIS2 to track immunization and family planning service provision at the national level.
What might be the advantages and drawbacks for your facility if it were to implement a project like the one just described?
LIS
In Haiti, laboratories throughout the country used a variety of electronic lab information systems (LIS). A project to connect the local LIS to the LIS at the national reference laboratory aimed to streamline referral testing and improve sample tracking. A lab tech at a regional laboratory could refer a sample to the national lab with the click of a button. The referral test order would be automatically sent to the national reference laboratory. The regional lab would then prepare the sample for transport. Once the sample arrived at the national lab, the reception could look up the order in their own system and proceed to test the sample. The results would be recorded in the national lab LIS and automatically sent back electronically to the referring regional lab.
What might be the advantages and drawbacks for your facility if it were to implement a project like the one just described?
Part 2: Success, Security and Maintenance
-
Reading: Benefits of interoperability
In the module on system architecture, you saw that while it may appear to be convenient to have one system that can fulfill all of the functions needed by a national health system, the complexity of such a system has drawbacks. It takes longer to develop a system that addresses a wide variety of needs and the complexity of such a system makes it harder to diagnose and resolve problems.
As stated earlier, Interoperability is about connecting systems. Each separate system specializes in its area—laboratory, billing, patient record, human resources, commodities tracking, equipment maintenance, etc. Specialization allows each system to do what it does best. Interoperability allows each specialized system to share needed information with other systems so that they can do what they do best as well. Through data and information exchange, interoperable systems can address the needs of both the facility and the national Ministry of Health, for example.
Instructions: Click or tap the three buttons to learn how interoperability can benefit the health facility, the overall health system, and policy making.
The Health Facility
Different departments within a facility can share patient information across programs and through time. A patient may come one month to be treated for TB in the TB program and another month attend the antenatal clinic in the Maternal and Child Health program. A system that shares patient information across departments or programs mean that the provider does not have to collect the same information, like the patient’s height or date of birth, over and over again with each visit. A physician can order a lab test through one system, have it automatically received at the laboratory, and receive the results back in the patient record system. Meanwhile, the lab has been tracking details about the specimen, the lab test equipment, reagents, and controls that the physician has no need to know. Information can be shared between facilities as well; as patients and staff move and transfer, their information moves with them.
Benefits can include:
- Reduced data entry time
- Information presented is relevant to the task at hand
- Less human error during documentation and transmission of orders, results, and reports
- More complete medical records for transferred patients
- Standardized data
- Automatic link between stocks (medication, reagents, supplies, etc.) and use
Potential Impact can include:
- More time spent on the clinical encounter with the patient rather than collecting unchanging routine data and assembling patient data from multiple sources every visit
- Better care coordination between providers through improved information sharing
- Reduction of unnecessary tests or treatment through information sharing and better decision-support
- Increased employee productivity
- Cost savings on communication and coordination
- Improved patient outcomes
Overall Health System
When seen from the national level, the overall health system is made up of care providers at hospitals and clinics, laboratories and dispensaries, supply vendors and transporters, drug warehouses, trainers, surveillance systems, and specialized programs and initiatives. At the health system level, sharing timely and accurate data to provide a more comprehensive picture of population health and health system performance is the key purpose of using interoperable information systems.
Benefits can include:
- Standardized data
- Less human error during documentation and transmission of data and reports
- Automatic reporting
- Automatic link between stocks (medication, reagents, supplies, etc.) and use
Potential Impact can include:
- Better care coordination between providers through improved information sharing
- Increased employee productivity
- Cost savings on communication and coordination
- Improved patient outcomes
- Improved logistics planning
- Improved planning for training healthcare workers
Policy-Making
Service-level systems like an EMR, LIS, etc., contain a lot of information about individual patients and facility needs. Policy makers at the regional or national level do not need to know an individual’s blood type or the date their prescription was last filled. Policy makers need the following:
- aggregate data
- trends over time or over geographical areas
- rates of commodity usage
- rates of patient retention in specific programs
- disease events (surveillance)
- stock out patterns
- distribution of diseases and interventions across various population groups (health disparities)
Benefits can include:
- Standardized data
- Less human error during documentation and transmission of data and reports
- Automatic reporting
Potential impact can include:
- Improved policy selection
- Improved alignment of policy to implementation
- Improved planning in logistics, training, infrastructure
- Improved disease outbreak response
- Improved financial analysis
-
Reading: Common Challenges (5 min)
Common challenges to successful implementation of interoperable systems at the facility level include:
- Internet connectivity at the facility
- Electricity/power
- National level internet service coverage
- Staff turnover
- Training needs or resources for training of system users
- Computer literacy of system users
- Computer administration skills and capacity
Reflection Questions: Do any of these apply to your facility? What are other potential obstacles to effective interoperable systems at your facility?
-
Quiz: Addressing Challenges (10 min)
Effectively addressing these types of challenges requires an investment of time and resources. Solutions vary depending on the specific situation.
-
Reading: Patient data security (15 min)
A common—and important—concern around interoperable systems that are exchanging patient data is the security of that data. How do we protect patient information from improper use, security breaches, and breaches of confidentiality?
Most security measures remain the same whether systems are interoperable or not. Protection of data, whether digital or paper-based, during collection and storage in one system, and transmission from one system to another are key measures for maintaining data security and confidentiality.
System Level
- Use secure messaging standards for transmitting data
- Encrypt sensitive data
- Limit access to authorized users
- Organize authorized access around “Need to Know” access levels
Environment Level
- Use antivirus, anti-intrusion software and firewalls
- Have a trained data security focal point at each facility
- Develop, disseminate, and enforce clear security policies at the facility level
- Develop, disseminate, and enforce clear guidelines, policies and regulations on data security, privacy and confidentiality at the national level
User Level
- Do not share passwords or user accounts
- Log off when leaving a computer work station
- Keep the computer or device software up-to-date
Glossary of Terms
If you need to refresh your memory on select terminology in this activity, please review the definitions below.
- Encrypt: to put computer data into a coded form that only an authorized user or system has the key to decode and put back into readable form.
Source: Encrypt. (n.d.). Collins English Dictionary - Complete & Unabridged 10th Edition. Retrieved April 17, 2017 from Dictionary.com website: http://www.dictionary.com/browse/encrypt
- Secure message: Secure messaging refers to an electronic messaging system where the contents of the message are encrypted between the sender and recipient in a manner that doesn't allow anyone other than the sender and the recipient to read it. Secure messaging is often provided as an online, server-based application that stores the data centrally and in one secure location.
Source: U.S. Centers for Medicare and Medicaid Services, cms.gov, and Wikipedia.org
-
Reading: How to identify problems related to interoperability (15 min)
Troubleshooting interoperable systems can be complicated. At the user and manager level, it is important to follow the same steps as you would for any technology troubleshooting. Start with the basics, ruling out the easy things like an unplugged cable, a mistyped password, or an unavailable remote system. With interoperable systems, it is even more critical to be specific and comprehensive in noting and documenting any issues you encounter.
- Try to reproduce the problem.
- Describe in a step-by-step fashion what you were doing when you encountered the problem: “First I navigated to the patient summary page, then I clicked on Get Lab Results…”
- Note when and where in the system the problem occurred.
- Be detailed and specific when data elements are part of the error, for example, patient lab results that don’t appear correctly, or incorrect dates for previous clinical visits; knowing what data element is involved can provide a clue to the system in which the problem originates.
Instructions: To better understand how these rules work, click or tap the scenario button to walk through an example of identifying a problem related to interoperability.
-
Reading: Roles in Maintenance and Use of Interoperable Systems (15 min)
Each person in the facility who uses or otherwise interacts with the HIS has a role to play in its effective and secure use.
Instructions: Click or tap the images on your screen to reveal additional information about the different roles in the maintenance and use of interoperable systems.
Facility Manager
- Know which systems are operating and what information can be obtained through each
- Plan for and ensure adequate training and mentoring of staff in system use
- Know who should use which system and ensure that system user accounts up-to-date with staff changes
- Promote routine security measures like securing one’s work station, protecting one’s user name and password, and prompt reporting of irregularities
- Incorporate system use and security measures into routine supervision. HIS tasks are as critical to job performance as clinical tasks
IT Personnel
- Keep system user accounts up-to-date with staff changes
- Ensure that staff regularly change their passwords
- Know which systems are operated in which departments of the facility
- Know the Help Line and issue reporting protocol for each system
- Know the basic architecture of the interoperable systems in the facility
Frontline HCWs
- Commit to using each system correctly by seeking training, mentoring, and support
- Know the account security requirements for each system to which you have authorized access
- Never use another person’s account ID and password to gain access to a system, even if you have authorized access to that system with your own account
- When you encounter a problem, troubleshoot first, before calling in IT support. Troubleshooting can include:
- Is CAPS LOCK on?
- Did you mis-type your user ID, password or other information?
- Are you using the correct password for this system and not for your email or another system?
- Is the computer/device and other hardware properly plugged in?
- Did you try restarting the application or the computer/device?
- Know the issue reporting protocol for your facility. This may include a specific form to fill or just be a list of information regarding the issue tha you are required to report, such as
- A description of the issue—what is the problem?
- A description of what you were doing in the system when the issue occurred
- The version of the system or hardware you were using when the issue occurred?
- Any troubleshooting steps you have already tried
-
Reading: Putting It All Together (5 min)
The value of a health information system is to get the right information to the right person at the right time. Interoperability is a powerful tool for connecting systems and facilitating timely and efficient flow of accurate information.
This module just presented three kinds of interoperability: human-mediated, point-to-point, and standardized. You may already be using one or more of these kinds of interoperable systems.
There are three levels of interoperability, with semantic interoperability — the ability to exchange, interpret, and use data amongst systems — being the gold standard.
As a healthworker, you may interact with only one health information system component, such as the EMR or the LIS, or you may use multiple systems to perform your routine tasks. Each person has a role to play in protecting patient information and maintaining the effective functioning of any health information system.
-
Reading: Summary (5 min)
Congratulations! You just completed this module. You’ve just learned about interoperability at the facility: what interoperability is, different examples of interoperability in action, and the role you play in using interoperable systems. Now go on to the final quiz.