Session 1: Introduction to Providing KP-Friendly Services
Welcome to the first self-study session in the Key Populations Service Provision Training course. In this session you will learn about some general practices to keep in mind when working with various key populations (KPs), and we will define relevant terms.
Getting Ready For This Session
- Remember to have your workbook and a pen or pencil handy.
- On average, you will need about 85-100 minutes to complete the session.
Learning Objectives
By the end of this session, you will be able to:
- Explain personal attitude and values about key populations
- Describe how stigma can influence working with key populations
- Define terminology often used when working with specific key populations
- List the key populations we work with in Zimbabwe
- Explain what it means to provide quality healthcare for key populations
Learning Activities
-
Introduction (2 min)
Working with key population (KP) groups can pose challenges for healthcare workers who are not familiar with the varying needs of different KPs. As you gain a better understanding and become sensitized to issues that KPs face, along with becoming more aware of your own feelings and actions, your ability to provide quality and compassionate health service will improve.
In this session we will explore your personal values around working with KPs and define some of the terminology used to better understand some of the language used, specifically around gender and sexuality.
-
Pre-Session Assessement (5 min)
Let’s start off with a quick check of your knowledge and comfort about providing KP services. Each question will have a score for you to track in your workbook. Please track your scores as you go through this assessment and make note of any content areas that you answered incorrectly. This exercise will help in identifying gaps and areas that need more attention as you go through the session content.
-
Values Clarification (10 min)
In this section, we will be exploring some of your opinions about KPs. Be honest as you consider your beliefs and values around the statements below. Note that many of the statements may be somewhat controversial and may provoke strong feelings.
Respond to each of the following statements by tapping ‘agree’ or ‘disagree’:
-
Reflecting on Values (10 min)
-
Stigma (5 min)
 We hear about stigma often in our work. Stigma is defined as
a set of negative and unfair beliefs that a society or group of people have about something.[1] Stigma often comes from the shame
or blame caused by false, unfair, or negative beliefs that people have about something they don’t
understand. The consequences of stigma can be serious, as stigma may cause people who need to be seen
for health services to feel too uncomfortable to seek treatment.Source: Merriam-Webster Dictionary
We hear about stigma often in our work. Stigma is defined as
a set of negative and unfair beliefs that a society or group of people have about something.[1] Stigma often comes from the shame
or blame caused by false, unfair, or negative beliefs that people have about something they don’t
understand. The consequences of stigma can be serious, as stigma may cause people who need to be seen
for health services to feel too uncomfortable to seek treatment.Source: Merriam-Webster DictionaryStigma can be experienced in different ways. It can be attached to one or more aspects of a person’s identity, such as HIV status, gender, or sexual orientation. It is important to recognise where stigma occurs most often for KPs.
What happens when we stigmatise clients from KPs?
- Clients may not want to come to the clinic, and thus may not receive needed treatment for HIV, STIs, or mental health disorders.
- Clients may not disclose important information about their sexual behaviours.
- Clients may feel shame and blame, which can lead to low self-esteem and engaging in risky behaviours.
Remember, as healthcare workers we strive to provide people-centred care that is focused on human rights and dignity, non-discrimination, participation and empowerment, access and equity, and a partnership of equals. Our role as healthcare workers is to care for people, not hurt them.
-
Stigma We Have Experienced in Our Lives (5 min)
Think about a time in your life when you felt lonely or rejected for being seen to be different from others. It does not need to be related to HIV or key populations; it can be any form of stigmatisation for being seen to be different. If you cannot think of a personal experience, think about when you may have witnessed stigmatising behaviour towards people living with HIV, and imagine how they felt.
-
Providing Healthcare Services for KPs (10 min)
Let’s watch this short presentation given by Abisha Jonga, Senior Program Manager at Zim-TTECH, on some of the issues that we need to be aware of while providing services to KPs.
This presentation was adapted from I-TECH Trinidad Key Populations Preceptorship training.
TranscriptTranscript
In this lecture I am going to discuss some overarching issues that should always be considered when working with key populations. I will share some definitions and give a short overview about the key populations, or KPs, that we’ll be covering in this training. And finally, I will provide some practical tips that should help you get more comfortable working with KPs.
The WHO defines KPs as populations who are at higher risk for HIV irrespective of the endemic type or local context and who face social and legal challenges that increase their vulnerability. They include sex workers, men who have sex with men, transgender people, people who inject drugs, and people in prison and other closed settings. In addition to experiencing elevated HIV risk and burden and facing legal and social issues, these populations historically have not received adequate priority in the response to the HIV epidemic. Often these populations lack quality services due to pervasive stigma, discrimination, and disapproving attitudes of providers. And providers are often ill-equipped to address the health needs of these specialized groups.
“The Zimbabwe Constitution Amendment (No. 20) ACT 2013 (under Chapter 2 Section 29 and Chapter 4 Section 76) recognises every Zimbabwean citizen and resident’s right to access healthcare, not to be turned away from any facility regardless of race, colour, religion, sexual orientation, gender identity and expression or sexual behaviour.” KPs are often marginalized, and we hope that we can help service providers become more sensitive to their unique needs with this training. It is important that health service providers see members of key populations as human beings who deserve fair treatment.
When we talk about key populations in Zimbabwe, they have been identified in the KP Handbook as including male and female sex workers; men who have sex with men, including men in prisons and in other closed settings; people who use and/or inject drugs; transgender and intersex people.
Key populations often face a number of barriers when they need healthcare:
- They have inequitable access to safe, effective, and quality HIV services.
- They face disproportionate levels of stigma, discrimination, violence, human rights violations, and criminalization. Stigma and discrimination against KPs often stems from social upbringing, culture and religion that only recognize males and females and the gender roles attributed to them. We will cover stigma in more depth later in this session.
- Significant barriers, such as police harassment, societal discrimination, and insufficient community-based services prevent them from getting the care they need.
Key populations friendly healthcare is healthcare that is accessible, affordable, and acceptable to key populations. It is also healthcare that is provided in a way that is respectful of their rights and dignity. Key populations friendly healthcare is essential to ensuring that all people have access to the healthcare they need. By providing healthcare that is respectful of their rights and dignity, we can help to reduce stigma and discrimination, and improve the health of key populations. Some elements that make a facility “KP friendly” include
- Making sure that healthcare facilities are welcoming and inclusive of key populations
- Providing culturally appropriate healthcare services
Making sure that your facility is KP friendly requires you to be set up as a safe space. Some of the elements that are necessary include:
- Creating a welcoming and enabling environment, from the minute the client walks through the gate they should be able to feel comfortable interacting with facility staff. This includes security, clerks, and medical staff.
- Respect all clients, treat them with dignity and sensitivity.
- Protect the human rights of clients. All clients should be treated like a person, be able to make informed choices, and feel safe.
- Provide non-judgmental health services including:
- Care
- Treatment
- Prevention
- Education
- Support
There are a few things to keep in mind when working with key populations. Many individuals can relate to more than one key population, that is to say that many people from key populations engage in more than one high-risk behaviour (e.g., injecting drugs and sex work, or a man who has sex with other men who also injects drugs). Therefore, they are likely to have higher HIV prevalence rates than those with only one type of risk. Key populations experience significant HIV burden, and they influence the dynamics of HIV epidemics.
Adolescents and young people from key populations are at significant high risk of HIV, higher than that of their older peers in these populations. Their rapid physical, emotional and mental development, complex psychosocial and socio-economic factors and poor access to and uptake of services increase their vulnerability and risk. Particularly for those under age 18 years, policy and legal barriers related to age of consent often prevent access to a range of health services, including HIV testing and counselling, harm reduction and other services provided specifically for key populations.
Without addressing the needs of key populations, a sustainable response to HIV will not be achieved.
AbishaReflection: Take a moment to think about the facility you work in:
- Is it an environment that is welcoming and enabling to KPs?
- What can you do to help make it friendlier?
Write your responses to the questions in your workbook.
-
KP-Friendly Health Services (5 min)
We heard from Abisha about what providing ‘KP-friendly’ health services entails. Let’s look a little deeper, especially at those elements that make a facility KP-friendly. Tap on the boxes for a description of each element.
Welcoming and inclusive environment
 A welcoming, inclusive environment is one that
focuses on removing barriers, making accommodations, and being deliberate in the provision of
informed and sensitive care. All staff at the facility should be part of this
culture of inclusion. The waiting area should reflect inclusiveness through diversity in the
posters and pamphlets displayed. Language should be inclusive and encouraging.
A welcoming, inclusive environment is one that
focuses on removing barriers, making accommodations, and being deliberate in the provision of
informed and sensitive care. All staff at the facility should be part of this
culture of inclusion. The waiting area should reflect inclusiveness through diversity in the
posters and pamphlets displayed. Language should be inclusive and encouraging.Respect
Showing respect for clients goes a long way towards establishing a positive relationship. Respect can take many forms including:
- How you speak—avoid using terms that could be offensive or stigmatising.
- Providing a setting that makes people feel comfortable discussing their health concerns.
- Listening to the client to understand what they want and need.
- Working together with the client to meet their needs.
- Being aware of your own biases and attitudes (and not sharing them).
- Being compassionate, supportive, and non-judgemental.
Appropriate services
Providing appropriate KP services can help to improve client trust and satisfaction, increase adherence to treatment, reduce stigma and discrimination, and improve the client’s quality of life. Components include:
- Clinical care that is tailored to the specific needs of the population. We will be covering those needs in more detail in subsequent sessions.
- Integrated health services that include information, counselling, diagnostics, treatment, and care. This also includes services that address such comorbidities as HIV, TB, STIs, and mental health issues.
- Confidentiality allows clients to receive care without fear of discrimination or retaliation. Health workers should not just keep health information confidential (unless necessary to share as part of patient care), but should also educate the client about their rights to confidentiality.
- Non-coercive care ensures clients are treated without the use of threats, force, or manipulation. It involves respect for client autonomy and their right to make decisions about their healthcare.
- Health education
- Referrals and linkage to other service providers, including counselling, legal, and self-empowerment projects.
Safe space
 A place where KP clients feel comfortable and
accepted, regardless of their background or identity. This includes not only the physical
environment, but also a culture of respect and non-judgement. Clients should also have access
to health information and education.
A place where KP clients feel comfortable and
accepted, regardless of their background or identity. This includes not only the physical
environment, but also a culture of respect and non-judgement. Clients should also have access
to health information and education.Staff trained and sensitised
 Both training and on-the-job support and
supervision should be provided to address the attitudes and skills needed to provide
KP-friendly services.
Both training and on-the-job support and
supervision should be provided to address the attitudes and skills needed to provide
KP-friendly services.Community support and participation
Inclusion of peer communities in the planning, monitoring and evaluation of services, and in applicable areas of service provision.
Key points about KP friendly services
- Individuals in KPs need to know the full range of services to which they are entitled, so that they can hold their healthcare workers and facilities accountable for providing them.
- Promoting access and identifying demand for quality comprehensive services is just as important as the supply and provision of those services.
- Healthcare workers have a duty to provide the best quality services they can to all people, regardless of what they may personally think about the actions, age, identities, or health conditions of their clients.
- Specific, comprehensive services are required to meet individual needs, and should follow international human rights principles and quality standards.
- Healthcare workers must orient services to the unique health needs of young key populations and the added barriers young people experience in accessing services. They also need to keep in mind that the term ‘young people’ covers a wide age range of people with varying levels of knowledge and experience, and adjust services accordingly.
Note that when working with adolescent KPs, you need to take special considerations to ensure that they fully understand their rights to confidentiality, provide health services in a safe space, and see that they have access to psychosocial support.
-
Testimony (2 min)
Let’s listen to Marcia Mwale, a primary counsellor, as she explains to us what she sees as important aspects to providing services for KPs.
Transcript
My name is Marcia Mwale, I am a primary counsellor. It is important to provide quality healthcare services to key populations in order to reduce the burden of HIV and STIs among the key populations. It also helps in identifying specific healthcare needs for key populations due to the frequent stigma and discrimination that the key populations face in our societies. It also addresses the mental health problems that KPs face and experience.
I would advise a new healthcare worker to first understand the key populations society. I would also advise the healthcare worker to respect human rights, inclusive of the KP rights too—especially that of their own sexuality. The healthcare worker should create an environment that is friendly and accommodates the KP family. The healthcare worker should learn to offer healthcare services without discrimination and being judgmental.
Marcia -
Gender and Sex Terminology (10 min)
Several terms are specific to working with KPs. Tap on each of these terms to learn more.
Gender
Gender is a concept constructed by society. Notions of gender tend to interact with other social norms relating to sexual orientation. Gender (male or female) is assigned at birth; and society has created norms that the two genders are expected to follow.
Gender can also be expressed as non-binary–that is, neither male nor female. Gender non-binary, or gender non-conforming, individuals reject social expectations based on the gender assigned to them at birth. It is often assumed that your gender is determined by your biological sex. The separation of gender and sex is most clearly seen in people who feel that their gender identity is not aligned with their biological sex.
Sexual orientation
This is who you are attracted to, with ‘heterosexual’ meaning you are attracted to people of the opposite sex (or considered straight), ‘homosexual’ meaning you are attracted to people of the same sex (gay or lesbian), and ‘bisexual’ meaning you are attracted to people of both sexes. There is also ‘asexual’, meaning you have a lack of sexual attraction to others.
Gender identity
This is who you think you are, how you have determined whether you fit more into the societal role of ‘woman’, ‘man’, both, neither, or somewhere along the spectrum.
Transgender
These are people whose gender identity is different from the gender they were thought to be at birth. ‘Trans’ is often used as shorthand for transgender. A transgender woman lives as a woman today, but was assigned male at birth. A transgender man lives as a man today, but was thought to be female when he was born. Some transgender people identify as neither male nor female, or as a combination of male and female.
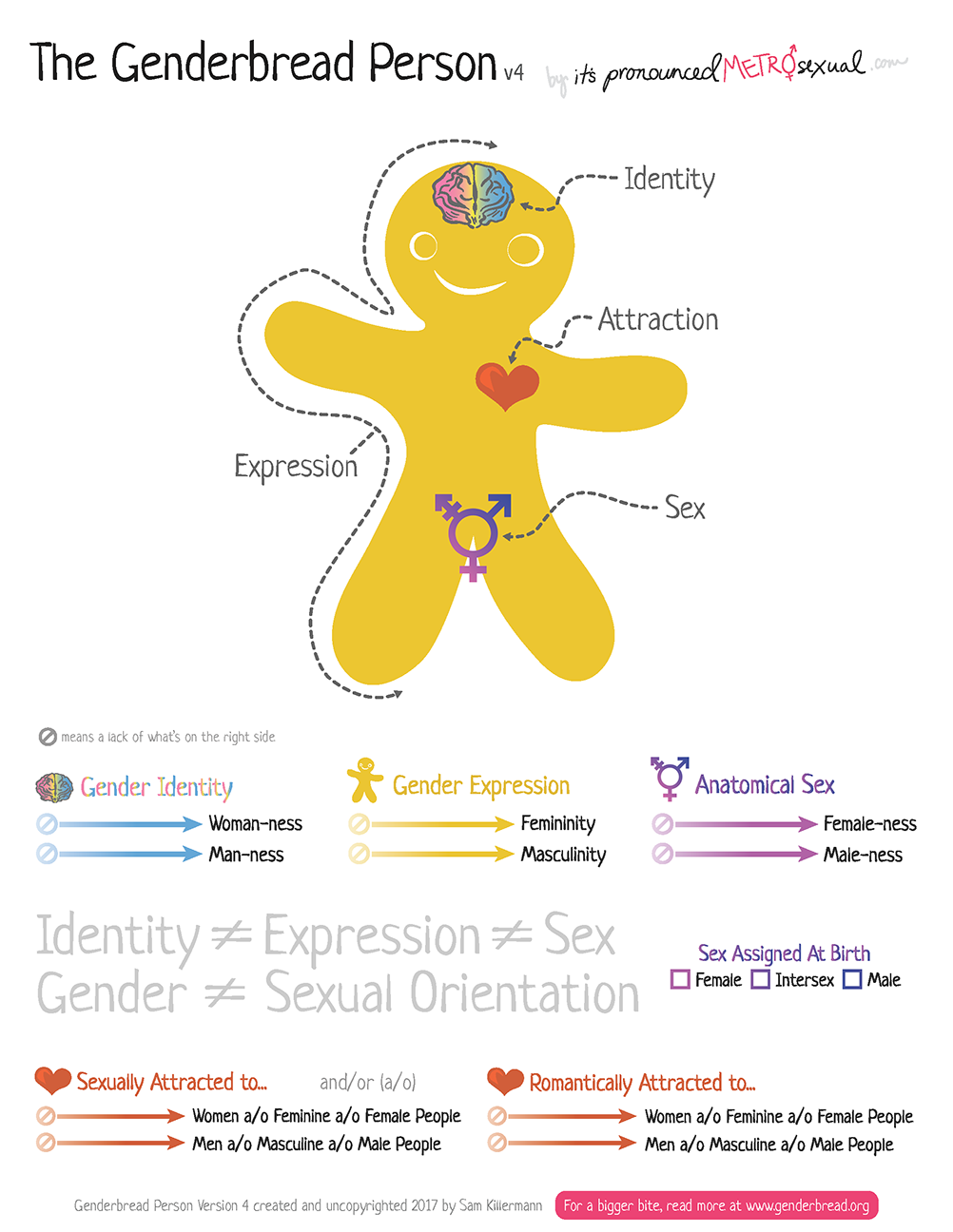
The Genderbread Person: In this model by Sam Killermann, you will see four main elements: identity, expression, attraction, and sex. The model shows how each of these continuums exist independently from one another. Tap on the image below to enlarge it and read through to help you see each of the continuums.
Sexual orientation and gender identity shape every aspect of our lives. Social expectations and legal definitions regarding men, women, and reproduction influence how we organise our medical, legal, education, and political systems.
We cannot make assumptions about the sexual orientation of those whose gender identity does not match their biological sex. Biological males who live as females may be attracted to males, to females, or to other transgender individuals. In many instances, people who do not conform to society’s gender norms are discriminated against and experience violence and abuse because they challenge the idea that gender identity is directly related to biological sex.
Note that there are many more definitions under the KP umbrella. The MoHCC KP Handbook has a glossary (pages 8-25) that will help you become more familiar with terms used when working with KPs.
-
Mercy and Chiedza (15 min)
Note that the clinic and people in this case study are fictitious.
Mercy is a 19-year-old woman who is coming to the Canterbury clinic for services. She is a sex worker, who is also studying to be an accountant. She is dressed in a very short skirt and low-cut top; as she walks through the gate, she sees the security guard pointing at her and whispering to the groundsman. As she proceeds to go check in with the clerk, the clerk looks her up and down and asks why she is here. Mercy says that she would like to discuss her issues with the healthcare provider and is not comfortable sharing them here. The clerk clicks her teeth, looks the other way, and then completes the check in.
Chiedza is a nurse at Canterbury clinic. She is walking past the reception area as Mercy is being checked in and sees how the clerk is treating Mercy.
Chiedza brings Mercy into the examination room to begin the assessment. Mercy discloses to her that although she is a sex worker, she is in school and the work is supporting her studies. She states that she sees how people look at her when she comes into the clinic, and often feels uncomfortable coming in for services.
When Chiedza asks what brought her in today, Mercy said that she is having some discharge and discomfort ‘down there’.
Bear in mind that there are a lot of stereotypes and myths about sex workers. Many different people engage in sex work, including women, men, men who have sex with men (MSM), and transgender people. Because sex work is considered a criminal activity, clients may not disclose that they engage in it. Sex workers may have primary relationships with one partner and may have children that they are supporting. They may be distrustful in healthcare settings because of past negative experiences of stigma, discrimination, and breaches of confidentiality from healthcare workers.
‘Male, female and transgender sex workers may face violence because of the stigma associated with sex work, which in most settings is criminalized, or due to discrimination based on gender, race, HIV status, drug use or other factors. Most violence against sex workers is a manifestation of gender inequality and discrimination directed at women, or at men and transgender individuals who do not conform to gender and heterosexual norms, either because of their feminine appearance or the way they express their sexuality.’[2]
World Health Organization, United Nations Population Fund, Joint United Nations Programme on HIV/AIDS, Global Network of Sex Work Projects, The World Bank. Implementing comprehensive HIV/STI programmes with sex workers: practical approaches from collaborative interventions. Geneva, World Health Organization, 2013.Sex workers often must survive in a very dangerous environment—they are vulnerable to being raped, robbed, beaten, and exploited by their clients, and arrested by the police. Sex workers feel they lack rights and are powerless to assert their rights and demand fair treatment—i.e., safe sex with fair payment and no violence. Many people believe that sex workers lose their rights when they start selling sex. But sex workers have the same rights as other people—such as the right to healthcare and freedom from inhumane treatment—and they should be able to access those rights.
Sex workers are as fully human as anyone else and entitled to be treated in the same way. Stigmatising sex workers does not help us to fight HIV. Instead of stigmatising sex workers, we need to show care and compassion—so that they can lead healthy lives and act in their own and other people’s interests.
-
Considerations for Providing Healthcare Services to
KPs (5 min)
It can be challenging to put your opinions and beliefs to the side when you are working with clients. Tap on each box to read some tips to help you be a KP-friendly provider:

Develop Your Own Self Awareness
You may have internal biases that can affect the way you talk or behave with certain clients. Staying aware of your own behaviours and attitudes allows you to acknowledge and change to be less judgemental.
Ask Yourself Questions
Pay attention to when you notice any stigmatising or prejudicial attitudes or beliefs coming up. When such thoughts or feelings arise, ask yourself:
- How does this belief serve me?
- What are the costs of keeping this perspective?
- How could change benefit me?
Remain Open and Compassionate
Set your assumptions aside to get to know who your client is. Try to imagine what your client might be experiencing.
Think About the Words You Use When Speaking
Be mindful of how you phrase your questions and don’t ask unnecessary questions. Stay professional and use simple, non-offensive language.
Pay Attention to Body Language
You communicate with more than words; take notice of whether you are smiling or grimacing, whether you make eye contact when you speak, and the tone you use when speaking.
Encourage Respect for All Clients
If you see peers or others engaging in stigmatising or discriminating behaviour, speak with them in private and let them know that such behaviour is disrespectful.
-
Action Plan (5 min)
Take a few minutes to think about what was covered in this session. Using the Action Plan form in your workbook, list two or three things that you will do differently in your job.
-
Post-session Assessment (5 min)
Now that you have completed this session, let’s take time to check your knowledge and comfort about providing KP-friendly services. Please track your scores as you go through this assessment, compare them with your pre-test scores, and make note of any content areas where you answered incorrectly.
-
Summary (2 min)
Human rights apply equally to everyone, regardless of their sexual practices, how they dress, and whether they use drugs or exhibit other behaviours that are not considered mainstream. As healthcare workers, it is our responsibility to provide appropriate, quality services. We need to remember that clients who are members of KP groups are also members of the community.
It is time to shift the paradigm:
- We need to acknowledge that KPs exist in Zimbabwe
- We need to sensitize all healthcare workers to the needs of KPs
- We need to advocate on behalf of the KPs we serve
-
Resources
Below are links to resources relevant to this session.
Title/Source File MoHCC KP Handbook Click to open file.