Session 4: Providing KP-Friendly Services for People Who Inject Drugs
Welcome to session 4! In this session we will talk about providing healthcare services to people who inject drugs (PWID). We will discuss what we can do locally, and look at best practices for risk reduction being used in other countries.
Getting Ready For This Session
- Remember to have your workbook and a pen or pencil handy.
- On average, you will need about 90-100 minutes to complete the session.
Learning Objectives
By the end of this module you will be able to:
- Describe the vulnerabilities of PWID in relation to accessing healthcare services
- Explain clinical considerations for working with PWID
- Discuss recommended prevention strategies for PWID
Learning Activities
-
Introduction (2 min)
In this session we will discuss some of the challenges and strategies involved in working with PWID. We will also explore some of the issues around intersectionality and the impact of stigma on PWID.
-
Pre-Session Assessment (5 min)
Let’s start off with a quick check of your knowledge and comfort about KP-friendly services for PWID. Each question will have a score for you to track in your workbook. Please track your scores as you go through this assessment and make note of any content areas that you answered incorrectly. This exercise will help to identify gaps and areas that need more attention as you go through the session content.
-
Interview (10 min)
Here is an interview that was conducted with Langton (pseudonym), an active PWID who receives clinical services at a public facility. He was asked the following questions:
- As a person who injects drugs, what is the biggest barrier you face when seeking healthcare services?
- What assumptions are made about you when people find out you are a person who injects drugs?
- Have you felt judged or discriminated against by a healthcare provider?
- Have you ever had difficulty accessing healthcare because of your drug use?
- What is it you would like healthcare professionals who are providing care for PWIDs to know?
- What are you able to do to prevent HIV as an active PWID?
- What harm or risk reduction approaches are you familiar with?
- How can facilities better provide healthcare services for PWID?
Let’s listen closely to Langton as he describes some of his experience in seeking health services, as well as some of his recommendations for improvements.
Transcript
As a person who injects drugs, what is the biggest barrier you face when seeking healthcare services?
Good morning, everybody.
As a person who injects drugs, the biggest barrier that I face when seeking health services is stigma and also discrimination, once the health workers are aware of my situation.
What assumptions are made about you when people find out you are a person who injects drugs?
So, the assumptions made about me is that I’m a criminal, simply because I inject drugs. And some label me as “junkie”, depending on what I’ll be putting on on that particular day. But the assumptions are that I’m a very, very dangerous person.
Have you felt judged or discriminated against by a healthcare provider? Have you ever had difficulty accessing healthcare because of your drug use?
So, I’ve felt judged—so discriminated against by most health workers where I go, especially if I have any challenges, like any opportunistic infections. We have never been given that treatment that we think might be good or treatment that is provided to everybody else.
So, in this way I have found it very difficult to go to healthcare services because of my drug use.
What is it you would like healthcare professionals who are providing care for PWIDs to know?
If the world health workers could possibly understand us, possibly it could have been very easy for us to really seek full healthcare. So, in most cases we go for private doctors where there’s no judgement.
So, what I would like health professionals to know when they are providing care for people who use injected drugs: first and foremost, these are people just like them and us. We all have the same human rights. We are capable. Some of us, we are professionals, you know?
Some health professionals should know that we are just normal. All we need are services.
What are you able to do to prevent HIV as an active PWID?
So, what we are capable of doing in regards HIV prevention as an active PWID is not to share needles with anyone. So, what we would need is possibly a supply of needles so that we get clean needles which are not used and this way it’s actually—it helps prevent HIV. We also need condoms, just like anybody else.
What harm or risk reduction approaches are you familiar with?
Harm reduction or risk reduction approaches that I’m familiar with is ART, condoms, and naloxone, and also methadone services, although the country does not yet have that. So those are some of the harm reduction programs I’m familiar with, which we think the country will be in a position to implement.
How can facilities better provide healthcare services for PWID?
And lastly, facilities—we believe should have trained medical staff that is aware of the needs for PWIDs and this way, we think, the issues to do with stigma and discrimination can be less. And we can have more PWID coming for treatment.
On another note, I would also appreciate if they could be a law that really encourages people who use and inject drugs to come for treatment. The current laws they do criminalize people who use drugs, so it becomes very difficult to reach too many of the PWIDs who really need treatment services in our country. Thank you so much.
Langton -
Working with PWID (5 min)
-
Providing Healthcare Services to PWID (20 min)
There are some considerations that need to be taken into account when you are providing services to PWID. Jacqueline Gavhera, Program Officer at Zim-TTECH, shares some foundational concepts to keep in mind. Watch her presentation.
Transcript
In this session, Providing Health Services for People who Inject Drugs, we will discuss some skills and information for working effectively with this key population.
Let’s review our learning objectives for this session. By the end of this session, participants will be able to:
- Discuss common barriers that people who inject drugs face when seeking health services.
- Explain HIV and STI prevention activities for people who inject drugs used in Zimbabwe.
Why are people who inject drugs considered to be a key population? People who inject drugs are one of the groups who are considered at high risk for contracting HIV and STIs. People who inject drugs are often involved in certain behavioural patterns which make them prone to contracting HIV. These behavioural patterns are often illegal and/or socially unacceptable and they are often stigmatised and discriminated against. As a result of discrimination, they are afraid of disclosure and are reluctant to seek HIV services designed for the general population and are vulnerable to contracting HIV.
As I mentioned, people who inject drugs are one of the high-risk key population groups. They experience a higher risk of HIV acquisition than other key populations. There are some reasons why people who inject drugs have a higher prevalence than average. There are certain behaviours that are known to increase HIV and other infections risk such as:
- People who inject drugs may directly share needles or other equipment used to prepare and inject drugs.
- There may be use of amphetamine-type stimulants which can lead to engagement in higher risk sexual practices. Also, people who inject drugs may be more at risk of acquiring HIV as a consequence of using drugs, such as engaging in commercial sex work or exchanging sex for drugs, money, accommodation, and other things.
- Poor access to healthcare, which can be due to a number of factors, including poverty, lack of insurance, and discrimination. Without access to healthcare, people who inject drugs are more likely to suffer from health problems, including HIV, hepatitis C, and overdose.
- They may not be empowered to use condoms or be given education about their risks and ways to reduce that risk.
Along with the risk factors I just talked about, people who inject drugs face several challenges. They include:
- High rates of HIV and hepatitis C infection, which are common.
- Stigma and discrimination can make it difficult for people who inject drugs to access healthcare and other services. They may be afraid to seek help because they fear being judged or rejected. Stigma can also lead to isolation and loneliness, which can make it more difficult to stay healthy.
- Unsafe injection practices are also a challenge faced by people who inject drugs. This includes sharing needles and syringes, reusing needles and syringes, and not cleaning needles and syringes properly. These practices can lead to the spread of HIV, hepatitis C, and many other infections.
- Lack of access to harm reduction services, such as needle and syringe programs, that can help to reduce the risks associated with injection drug use.
People who inject drugs encounter quite a few barriers when it comes to getting health services. Some of the most prevailing barriers are:
- There may be a lack of health literacy, people who inject drugs may not be aware of the health services that are available to them, or they may not know how to access them.
- They may have had poor experiences with healthcare providers or the healthcare system and do not feel safe to return to those healthcare centers.
- They may have had poor experiences with healthcare providers or the healthcare system and do not feel safe to return to those healthcare centers.
- They don’t have money to access services, get transportation, or spend the little money they have on food or drugs.
- Fear of stigmatization, people who inject drugs are often stigmatized and discriminated against by society, including by healthcare providers. This can make them reluctant to seek care, even when they are sick.
- In terms of location—health services may be located far away from where people who inject drugs live, making it difficult for them to travel or to get there.
- Fear of arrest—people who inject drugs may be afraid of being arrested if they seek care, especially if they are using illegal drugs.
These barriers are very real. People who inject drugs may also worry that they will be stigmatised after disclosing that they take drugs or that they might be denied medical help because they take drugs. Any of the barriers mentioned here, as well as other barriers, can stop people who inject drugs from contacting healthcare facilities for health services.
Let’s look at some considerations that need to be made when providing health services to someone who injects drugs.
Stigma is an issue that comes up in every aspect of care for people who inject drugs. Because people who inject drugs often face stigma from healthcare providers and the general public it can make them reluctant to seek care, even when they need it. It is important for healthcare providers to be aware of this stigma and to create a non-judgmental environment where people feel comfortable seeking help.
Harm reduction is an approach to healthcare that focuses on reducing the negative consequences of drug use, rather than on abstinence. This can include providing sterile needles and syringes, naloxone for overdose prevention, and counseling on safer injection practices. Harm reduction is an important part of providing care to people who inject drugs, as it can help to prevent the spread of disease and improve overall health.
Mental health: People who inject drugs are at an increased risk of mental health problems, such as depression, anxiety, and post-traumatic stress disorder. It is important for healthcare providers to screen for mental health problems and to provide appropriate treatment.
Access to care: People who inject drugs often have difficulty accessing healthcare. This can be due to a number of factors, including cost, transportation problems, and fear of discrimination. Healthcare providers should be aware of these barriers and work to make sure that people who inject drugs have access to the care they need.
Women are known to be more susceptible to HIV infection because of gender-based violence. Women may be pressured to share needles and engage in high-risk sexual activities. Women are also more likely to conceal their drug-taking behavior because of societal discrimination and the threat of losing custody of their children. This discourages them from accessing medical care and HIV services.
We want to break down barriers, and create a compassionate environment that supports every individual, regardless of their key population identity.
Now let’s talk about prevention. As part of a harm reduction focus, we want to do everything we can to ensure that our clients who inject drugs are provided with prevention services. Some of the prevention measures that we can take are:
- HIV counseling and testing services, and for those who test positive, access to HIV treatment to achieve viral suppression, which will lead to better individual outcomes and reduce onward transmission.
- For those who are negative, offer PrEP.
- Provision of condoms and lubricants, latex condoms are highly effective at protecting against HIV. They also protect against other STIs and unintended pregnancy.
- Screening for health conditions such as HIV, hepatitis, TB, skin conditions, mental health issues.
- Providing the client with information and educating them on safer practices such as not sharing needles, learning how to clean their needles and equipment, helping them understand what health risks they face. These education sessions need to happen in a non-stigmatizing, non-judgmental way.
- Discussions around the risk of overdose. These are difficult discussions to have, and it is important to build trust and rapport before initiating.
As healthcare workers we mustn’t let our own issues and feelings get in the way of providing quality care for people who inject drugs. We should see every connection with them as an opportunity to promote health and discuss ways to reduce risk.
People who inject drugs are interested and capable of making changes to improve their health and safety. The aim is to provide a client with information, tools, and support to attain their self-defined goals. Conversations about health promotion or safe drug use do not condone drug use but demonstrate compassionate pragmatism.
Meaningful therapeutic relationships with people who inject drugs are possible and important to care. Each people who inject drugs has a unique and complex pathway to substance use and misuse. There are many possible contributors to an individual’s initiation of substance use (for example curiosity, family norms, stress, trauma, mood disturbance, and so many more). Minimizing assumptions and being open to each client’s unique experience can promote candid conversation about substance use/misuse. Readiness is key to substance use treatment efficacy. Healthcare providers often wrongly assume that every people who inject drugs wants to quit. Focusing on recovery as the only goal can alienate people who inject drugs.
The primary goal of a conversation is for the healthcare provider to establish themself as a resource and ensure people who inject drugs are comfortable returning for care or additional resources. Feeling judged or condemned is a major barrier to disclosing drug use. In healthcare experiences, people who inject drugs often experience betrayals of trust, denial of appropriate care, or engagement of security or police that make them wary.
Health care providers can promote candid disclosure and meaningful goal setting. People who inject drugs who have good rapport with their care provider are more likely to discuss their drug use, adopt provider recommendations, maintain continuity of care, and seek timely care before it is too late.
Remember, there are things that you should remember when working with people who inject drugs. Like with all clients, we want to use good communication skills and treat people who inject drugs clients with dignity. Here are some additional points to keep in mind and remember as you go:
- Be respectful and non-judgmental when providing services.
- Use person-first language, describing what the person “has” rather than what they “are”. For example, using the term “person who injects drugs” rather than calling someone a “drug addict” is less stigmatizing and encourages a more empathetic and supportive approach.
- Provide information about harm reduction strategies. Your client may not have received information before and it will be helpful for them to understand ways that they can reduce their risk of contracting HIV, STIs, or other health issues.
- Screen for mental health problems. There is often a link between mental health issues and injection drug use.
- Refer the patient to other resources, as available.
Let’s review some of the key take-aways from this presentation.
- People who inject drugs are at a high risk for contracting HIV, STIs, hepatitis, and other infections.
- Stigma and discrimination from healthcare workers, and the general public can cause people who inject drugs to avoid accessing healthcare services.
- People who inject drugs deserve to be treated with dignity and respect, we need to ensure that staff is educated and stigma reduction is addressed.
- We need to provide education on prevention and risk reduction to people who inject drugs as part of their healthcare service.
Self-Reflection
-
PWID and HIV (5 min)
PWID are one of the groups most affected by HIV; they are more likely to have HIV than the general population.
-
Clinical Care for PWID (5 min)
 PWID are a population who often have unmet healthcare needs,
which puts them at increased risk for a number of health issues. Key healthcare services that should be
addressed with clients who are PWID include:
PWID are a population who often have unmet healthcare needs,
which puts them at increased risk for a number of health issues. Key healthcare services that should be
addressed with clients who are PWID include:- HIV testing and counselling
- HIV and STI prevention
- PrEP
- Condoms and lubricant
- Latex condoms are highly effective at protecting against HIV. They also protect against other STIs and unintended pregnancy.
- Using a water or silicone-based lubricant during sex can help prevent condoms from breaking or slipping, and help prevent traumas that cause breaks in the skin, which can increase the risk of HIV transmission.
- ART and viral load monitoring
- Diagnosis and treatment of TB
- Prevention, diagnosis, and treatment of hepatitis (vaccinate when available)
- Prevention and treatment of STIs
- Prevention and treatment of skin conditions
- Targeted information, education, and communication
- Discussion around the risk of overdose
- Mental health screening
If the client is incoherent and unable to participate in their clinic visit, you may be faced with a situation that requires a transfer to emergency care. In such cases, follow your facility’s client transfer protocols. Always be compassionate and keep the client’s best interest in mind.
-
Harm Reduction Services for PWID (8 min)
The term ‘harm reduction’ has its roots in drug use (particularly injection drug use), but its scope has broadened to include other risk behaviours that may be associated with drug use or sex work.
Harm reduction uses practical strategies that reduce negative consequences associated with drug use and other risky behaviours. Harm reduction incorporates a spectrum of strategies, including safer use, managed use, and abstinence. Harm reduction strategies meet people where they are.
-
Harm Reduction
- Accepts that some ways of using drugs are safer than others and applies evidence-based interventions (e.g., syringe access, overdose prevention) to reduce the negative consequences of drug use or sex work (e.g., overdose fatalities, HIV/HCV transmission, injection-related wounds).
- Moves past judgement of another person to instead address their drug use and the harm it causes them.
- Recognises a continuum of use, modelling the stages of change theory.
- Does not make drug use acceptable; instead, it takes a more pragmatic/realistic approach, accepting that people use drugs.
- Works to ELICIT POSITIVE CHANGE.
- Provide linkages to additional services.
-
Clean Supplies
- Recommend never sharing needles, instead always use a new syringe and needle. If needles must be shared or reused, HCV can be reduced, and HIV eliminated, by using bleach to clean them:
- Fill the syringe with cold water; shake it and push the water out. Repeat until no blood is visible.
- Fill the syringe with undiluted bleach and let it sit for 2 minutes ideally (or at least 30 seconds).
- Rinse with fresh clean water.
- Advise the client to use clean, single-use supplies (cottons, cookers) and clean water (sterile). Water, cottons, and cookers are often used to prepare a drug for injection; they can carry hepatitis C or HIV if they come into contact with a used syringe. They should be used once and not shared. If reuse is required, disinfect cookers with bleach to reduce the risk of infectious disease.
-
Ask: “What steps do you take to keep yourself
safe when using?”
- Advise the client to not use alone, only in the presence of trusted people who can provide care if needed.
- Encourage using caution with all drug supplies and new sources, especially if the source or supply is associated with overdoses or other problems.
- Recommend avoiding taking all the drug at once and not rushing.
- Starting with a small amount (‘test shot’) may help prevent overdose as a drug cannot be withdrawn once it has been injected.
- Together, come up with ways to create a safer environment during use and/or opportunities to decrease the frequency of drug use.
In many communities, harm reduction strategies are focused on drug use and sex work. Sex work includes prostitution, sex for drugs, and stripping.
 When directing harm-reduction strategies targeting PWID
involved in sex work, keep these points in mind during your discussion:
When directing harm-reduction strategies targeting PWID
involved in sex work, keep these points in mind during your discussion:- Discuss both safer sex work AND safer sex.
- PWID and sex workers may share networks.
- All clients should be offered condoms.
- Share STI prevention messaging.
- No one should feel singled out for being offered safe sex information.
Harm reduction does not encourage drug use or continuation of unsafe behaviours. At its core, the approach demands a non-judgemental attitude, a radical love for another person who is choosing to live in a way you may disagree with, or that may threaten their own life—or that is just a different lifestyle, a different way of living that is likely to hurt only themselves.
Harm reduction does not provide drugs, but it can help a person find safer ways to use them so that they can avoid HIV, hepatitis C, or other infection. The idea is to keep the person alive so that they can find recovery for themselves. A person who is physically very sick has much more to deal with than just their addiction; it can also be overwhelming and costly. By meeting a person where they are (whether they are using drugs or engaging in sex work, etc.), we can provide care to keep them as safe as possible while providing options, resources and a warm hand to help, and additional care.
-
Harm Reduction
-
Principles of Harm Reduction (8 min)
There are some basic principles to keep in mind when you are providing any type of harm reduction services. Let’s review them here.

Health and Dignity
Establishes quality of individual and community life and well-being as the criteria for successful interventions and policies. Our goal is to focus on the health and dignity of individuals and provide them with the resources they need at any stage. The vision of health and wellness is a person’s own.
Client-Centred Care
Calls for non-judgemental, non-coercive provision of services and resources. Some examples of this are providing linkage to hepatitis treatment even if the client wants to continue using, providing health tests even while they are using, offering treatment for only the substances they want to stop abusing, and offering condoms and safe sex equipment.
Client Involvement
Ensures that persons who use drugs have a real voice in the creation of programmes and policies designed to serve them. Examples:
- Having peers and clients on committees that monitor programmes and services.
- Asking a team or individuals about changes or improvements they would like to see in services offered and how those services are delivered.
- Asking people what they are comfortable with and what they really don’t want.
- LISTENING.
Client Autonomy
Affirms people who use drugs as their own primary agents of change. Encourages autonomy through client involvement, client-centred services, and self-efficacy—that is, the individual’s belief in their innate ability to achieve goals.
Clients can:
- Choose whether or not to participate in harm-reduction strategies and programmes.
- Voice what helps them and what hurts them.
- Help develop programmes and decide whether or not to participate in them.
Sociocultural Factors
Recognises that social inequalities affect both people’s vulnerability to potential harm and their capacity for effectively dealing with it. Sociocultural factors include the effects and limitations of poverty, class, education, social isolation, trauma, and sex discrimination.
Realism
Does not attempt to minimise or ignore the real and tragic harm and danger that can be associated with illicit drug use or other risk behaviours. Although we may be coordinating and delivering harm-reduction techniques and services, we cannot cover up, mislead, or deny the real and potential dangers and health risks involved with drug use and other risky behaviours.
-
Case Study (10 min)
Quality is a young person who injects drugs. He has heard from his friends who receive healthcare services from the nearby clinic that young people are offered PrEP for free. He decides to come to Shoreline Clinic for services. Clara, a nurse at Shoreline, begins the screening process with Quality. While asking questions, she notices that Quality is looking up at the corner of the room and only engaging with one-word responses.
Quality begins to open up and shares that he injects drugs. Clara had suspected this, but did not want to make any assumptions. They complete the screening and determine that Quality is a good fit for PrEP.
Quality returns for a follow up appointment four weeks later. Clara meets with him and sees that he is much more communicative. She takes the opportunity on this visit to discuss risk reduction related to his drug use.
-
Intersection of PWID with Other KPs (5 min)
 Key populations may experience intersectional stigma when
they belong to more than one of the defined key population groups. For example, it is not uncommon to
see a sex worker, an MSM, or a person of trans experience who is also PWID. This intersectionality can
have a negative impact on health and healthcare, making it even harder for the client to come in for
services.
Key populations may experience intersectional stigma when
they belong to more than one of the defined key population groups. For example, it is not uncommon to
see a sex worker, an MSM, or a person of trans experience who is also PWID. This intersectionality can
have a negative impact on health and healthcare, making it even harder for the client to come in for
services.Beyond the stigma faced by PWID, there is the potential for gender-based violence and other forms of violence against PWID. Women who inject drugs face a higher risk of violence. Violence is a human rights violation!
As discussed in previous sessions, stigma and discrimination are often barriers to services for KPs. Think about how much harder it becomes for a client to seek care when they are facing intersectional stigma.
When working with intersectional clients who are PWID, here are a few additional practices to employ that address human rights and employ gender-sensitive programming:
- Sensitise clinical teams working with PWID on intersectional stigma, discrimination, and violence against PWID to help them understand and question negative attitudes (both their own and those of others).
- Reach out to PWID with information and resources.
- Fully integrate violence response services as part of PWID services.
- Work with the police to prevent violence against PWID and to document incidences of violence experienced by PWID.
-
Risk Reduction for PWID in Other Countries (10
min)
Harm reduction services, substance use treatment programmes, and HIV services targeting PWID are not widely available across Africa. However, there has been a concerted effort to implement comprehensive interventions, including programmes that incorporate HIV prevention and treatment. Methadone has been introduced in several African countries with large PWID populations (e.g., Tanzania, Kenya); research has demonstrated that methadone treatment programmes serve as an effective mechanism through which HIV prevention, treatment, and care services can be delivered to improve the health of PWID. Additionally, law enforcement has become recognised as a critical agent in diverting PWID from the criminal justice system to health and social services.
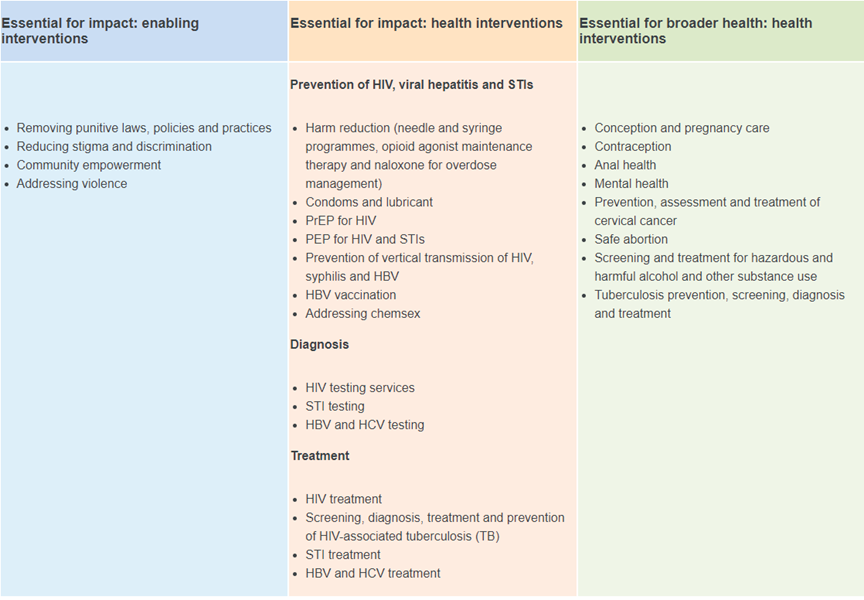
There are programmes being encouraged and implemented in other countries that are showing some success towards addressing the health issues of PWID. The WHO has shared the following overview and recommendations:[1]
Source: People Who Inject Drugs. Global HIV, Hepatitis and STIs Programmes. WHO."People who inject drugs are at increased risk of HIV, tuberculosis (TB), and viral hepatitis B and C (HBV and HCV), in addition to overdose. Globally, around 11 million people inject drugs. Approximately 1 in 8 (or 1.4 million) of these people are living with HIV,[2] while 39.4% have viremic HCV infection.[3]
"Injecting drug use accounts for approximately 10% of new HIV infections globally.[4] And an estimated 23–39% of new HCV infections occur among people who inject drugs. Globally, 1 in 3 HCV deaths are attributable to injecting drug use. In some regions, such as Eastern Europe and Central Asia, prevalence rates for both HIV and HCV are particularly high. Furthermore, there are approximately 2.3 million HIV–HCV co-infections worldwide, of which more than half (1.3 million) occur in people who inject drugs.[5]
Source: UNODC World Drug Report, 2020.Source: Grebely et al., Addiction, 2019.Source: UNAIDS, 2020.Source: WHO, 2016."WHO recommends a package of harm reduction interventions to reduce transmission of HIV, HCV and HBV, as well as deaths due to overdose, among people who inject drugs. These interventions also allow people who inject drugs to access the health-care system and engage with TB care and mental health services. Harm reduction—including needle/syringe programmes, opioid substitution therapy and community distribution of naloxone—is an evidence-based approach to HIV and HCV prevention, treatment and care for people who inject drugs. It is strongly supported by other United Nations agencies. Harm reduction interventions are essential to achieve the global targets for viral hepatitis elimination and control of HIV/AIDS epidemics.
"However, criminalization of drug use and stigma and discrimination against people who inject drugs contribute to ongoing epidemics of HIV, viral hepatitis and TB. This is because people who inject drugs fail to access harm reduction and other health services. In many settings, harm reduction programmes are simply not available, or are extremely limited in accessibility and availability due to restrictive and ineffective policies and laws. Global coverage of harm reduction interventions is extremely low—less than 1% of people who inject drugs live in settings with sufficient, combined and high-coverage services."
A comprehensive package of services is recommended to address these infectious diseases in people who inject drugs.
-
Tips for Working with PWID (2 min)
 Although we want to always practice effective communication
skills, stay open-minded, and keep our own assumptions in check, here are some tips for working with
PWID:
Although we want to always practice effective communication
skills, stay open-minded, and keep our own assumptions in check, here are some tips for working with
PWID:- Always begin by building rapport with the client.
- Be aware of potential stigma, including intersectional stigma.
- Be patient and understanding.
- Give honest information, using clear, respectful language.
- Provide resources with no pressure or judgement.
- Teach safe practices.
- Inform the client about dangerous situations.
- Refer to treatment and recovery supports.
- Help with taking the next right step today.
- Identify strengths (everyone has them!).
- Protect others from unnecessary harm.
- Be kind.
- Encourage testing for greater awareness of one’s health.
-
Action Plan (5 min)
Looking at the WHO-recommended comprehensive package above, pick out a few items that you will work towards implementing in your facility. In your workbook, list the action you will take, a timeframe for doing it, and what support you will need.
-
Post-Session Assessment (5 min)
Now that you have completed this session, let’s take time to check your knowledge and comfort about providing KP-friendly services for PWID clients. Please track your scores as you go through this assessment, compare them with your pre-test scores, and make note of any content areas where you answered incorrectly.
-
Summary (2 min)
Congratulations on completing this session where we learned about some of the issues and considerations to factor into our work when we meet with clients who are PWID. We covered the unique risk factors for PWID, along with the intersectionality of the stigma they face, and we reviewed clinical concerns and harm reduction strategies.
-
Resources
Title/Source File Operational and Service Delivery Manual for the Prevention, Care and Treatment of HIV in Zimbabwe Click to open file.