Session 1: HIV Prevention
Voluntary Medical Male Cicumcision (VMMC)
In this session, we will discuss the importance of practicing preventive health behaviors, the universal standard precautions to prevent occupational exposure to bloodborne pathogens, including HIV and how to treat exposure with post-exposure prophylaxis (PEP).
In this section, we’ll look at how male circumcision decreases the risk of HIV transmission and discuss Zimbabwe’s voluntary medical male circumcision programme.
Learning Objectives
By the end of this session, you will be able to:
- Describe the evidence linking Male Circumcision (MC) with a reduction in HIV prevalence.
- Define voluntary medical male circumcision (VMMC).
- State the methods and service delivery models used in VMMC.
- Describe the benefits and risks of VMMC.
- Describe follow-up care regarding wound care, adverse events, counseling issues, referral and linkage to care post circumcision.
- Recognise adverse events that require clients to be referred urgently/immediately post circumcision.
Learning Activities
-
Introduction (5 min)
Medical male circumcision has been identified as a highly effective biomedical method to reduce new HIV and sexually transmitted infections. It is a one-time intervention that provides men lifelong partial protection against HIV as well as other STIs. It should always be considered as part of a comprehensive HIV prevention package of services to be used with other methods of prevention, such as female and male condoms. Voluntary Medical Male Circumcision (or VMMC) also helps prevent HPV infection in the female partner, thereby lowering the chances of developing cancer of the cervix.
Globally, male circumcision is widely practised for a variety of reasons including religious, cultural, and medical. Currently, around two thirds of African men are circumcised, mainly for religious and cultural reasons. It has been observed that in countries where circumcision is commonly practiced, HIV rates are much lower compared to countries that do not circumcise.
Research studies have shown a lower risk of infection in circumcised men compared with uncircumcised men, as well as a lower prevalence of HIV infection in populations where male circumcision is common. In Uganda, Kenya, and South Africa, studies were done to compare new HIV infections in men who were circumcised and not circumcised. The results of these studies showed that male circumcision reduces the chances of men acquiring HIV—in one study by as much as 60%.
Based on these data, WHO and UNAIDS recommend that countries promote male circumcision as an additional method of HIV prevention. Countries or settings with generalized HIV epidemics and low prevalence of circumcision should urgently scale up circumcision services.
In North and West Africa, where men are mostly circumcised, HIV rates are lower compared to Southern Africa, where fewer men are circumcised and HIV rates are higher.
Zimbabwe has an estimated prevalence rate of 10% for male circumcision. It’s strategic goal for VMMC is “to contribute to the reduction of HIV incidence by scaling up VMMC to reach 80% of HIV-negative men between 13-29 years by 2017.”
A modelling exercise was done to show the potential impact of male circumcision on HIV incidence. The exercise showed that if 1.3 million men were circumcised, 212,000 HIV infections could be averted (so four circumcisions to avoid one person being infected with HIV). In this scenario, HIV prevalence would decrease to 4.4% by 2025, compared to an anticipated 7.3% if male circumcision is not scaled up.
-
What Is Male Circumcision? (5 min)
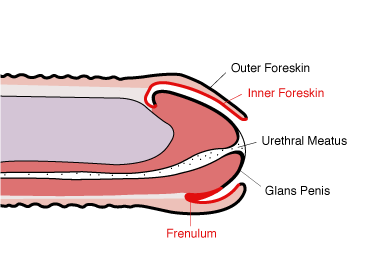
Male circumcision is the complete removal of the skin that covers the head of the penis (foreskin). The skin is removed through surgical or non-surgical methods. The procedure is done voluntarily and performed in health facilities by trained medical personnel.
 McCoombe and Short, AIDS 2006, 20:1491-1495
McCoombe and Short, AIDS 2006, 20:1491-1495The primary cells through which HIV enters the body are called Langerhans cells. These cells are present in high density in the epithelium of the inner foreskin and are nearer the epithelial surface due to lack of keratin.
Study of foreskin and cervical biopsies showed that the inner foreskin is more easily infected with HIV than external foreskin or cervical tissue. The inner mucosal surface of the foreskin lacks the thick layer of keratin that covers most exposed skin. This leaves numerous mucosal Langerhans cells and other immune cell targets easily accessible to HIV infection.
The highly vascularized foreskin mucosa, and in particular the frenulum, is prone to tearing and bleeding during intercourse. These micro-injuries allow easy access of HIV to the bloodstream. If an uncircumcised male has an ulcerative STI, this may facilitate entry of the virus, leading to increased risk of HIV through the disrupted mucosal surface of the ulcer.
-
Delivery of VMMC (5 min)
Delivery of VMMC in Zimbabwe employs three models of service delivery: static, outreach, and mobile. Tap on each model to learn more about it.
Static model
The static model involves permanent structures within existing district health care facilities. The resources are sometimes shared with the facility as well as support outreach and mobile sites. Static sites offer male circumcision all year, except for when the team does outreach events, and usually targets males within the vicinity of the sites.
Outreach model
The outreach model involves temporarily using existing structures at facilities not offering male circumcision and is only available during periods of high demand. The target population is males in remote areas without facilities offering male circumcision.
Mobile site model
Like the outreach model, the mobile site model targets males in remote areas. The mobile sites uses temporary structures like tents and semi-permanent structures for short periods of time or during high demand.
Eligibility criteria
Eligibility criteria for inclusion in the Zimbabwe MC programme includes:
- Uncircumcised men and boys above the age of 10 years
- No contraindications such as keloids, bleeds, hypospadias, or epispadias disease
- Consent to three medical visits
- And that sexually active men consent to avoiding sex for six weeks after the circumcision.
HIV tests are also recommended before undergoing the procedure. However, clients are still eligible for male circumcision should they decline a test.
-
Methods for Male Circumcision (5 min)
Male circumcision is done either through the surgical or non-surgical method through use of devices. The PrePex, device comes in different size from A (the smallest) and E (the largest). These device sizes are currently placed on males 14 years and older. Smaller sizes for younger males are under qualification by WHO.

The PrePex device for male circumcision involves compression of the foreskin between an elastic ring and a hard surface that is sufficient to occlude circulation and produce tissue ischemia and necrosis. After device placement the entire foreskin is left until the foreskin necrosis and can be excised.
Ensure that there is non-accumulation of urine under the foreskin (by directing the urine flow from urethra) before removal of the device as this can cause a stench smell.
The Prepex device procedure is faster and bloodless, and no injections for anaesthesia or stitches are needed. It also allows men to take less time off work and can be conducted by nurses in simple settings.
Disposal of foreskins
In accordance with Human Tissue Act of 1982, all foreskin and surgical waste are incinerated at the circumcision centre. Do not remove this waste from the centre. One of the minimum conditions for opening a circumcision centre is that it should have a functional incinerator where such waste is burnt at very high temperatures. Members of the public should be assured that foreskin and waste are disposed of safely.
Genital hygiene
Health providers and mobilisers should educate communities on importance of maintaining personal hygiene before, during, and after the procedure.
Tap on each arrow in the graphic to learn more.
After Procedure
- Education on the genital hygiene/wound care
- Providing clean or sterile dressings to use at home
- Client given flyers on wound care
During Procedure
Follow standard surgical protocols on skin preparation of the genital area
Before Circumcision
Client encouraged to bath thoroughly and wash under the foreskin
-
Benefits and Risks (5 min)
Benefits
If circumcision is being done for reasons other than the treatment of a specific medical problem, the health benefits are primarily preventive, and may only be realized long after the procedure.
- Reduction of chances of men acquiring HIV by 60%1
- Improves hygiene of the penis
- Reduces the risk of getting other STIs, such as herpes and syphilis
- Helps prevent cancer of the penis
- Prevents inflammation of the glans (balanitis) and the foreskin (posthitis)
- Reduces the risk of urinary tract infections in childhood
- Reduces complications that involve the foreskin such as inability to retract the foreskin (phimosis) and swelling of the retracted foreskin (paraphimosis)
Benefits for women include:
- A woman with a circumcised partner has lower chances of getting infected with the virus that causes cervical cancer.
- A woman with a circumcised partner also has a lower risk of chlamydia infection, which can cause infertility if it remains undetected.
- Reduces chances of HIV infection to the woman.
Male circumcision is not recommended for HIV-positive men, as there are no health benefits for them in terms of HIV prevention. However, if the man still wants to be circumcised, appropriate counselling will be provided. He should be made aware that wound healing may take longer than in HIV-negative men. There is higher complication rate of MC in HIV-positive men in advanced stages of HIV infection.
Risks
Circumcision may reduce the risk of acquiring some infections and related complications but does not guarantee complete protection. The degree of risk of the individual is likely to depend on his behaviour and where he lives.
As for any surgical procedure, there are risks associated with circumcision. The problems generally occur during or soon after the procedure. They include pain, bleeding, haematoma, infection at the site of the circumcision, increased sensitivity of the glans penis for the first few months after the procedure, irritation of the glans, meatitis, injury to the penis, and adverse reaction to the anaesthetic used during the circumcision. These complications are uncommon when circumcision is performed by well-trained, experienced health care personnel in adequately equipped facilities. Data from controlled trials show that under such conditions, few procedures result in complications. The complications are usually readily manageable and rapidly resolved.
Male circumcision does not offer complete protection against HIV. A circumcised person will still need to practice other HIV prevention behaviours, which include abstinence, reducing the number of sexual partners, being faithful to one sexual partner, using male or female condoms correctly and consistently, and knowing one’s HIV status.
-
Knowledge Check (5 min)
-
Follow-Up Care (10 min)
Follow- up care for male circumcision is very important to discuss with your clients. Follow-up visits are recommended to all voluntary medical male circumcision clients to ensure all adverse events are identified and managed appropriately.
Tap the tabs below to learn more.
Wound Care
Wound care is very important after circumcision to allow healing and prevent infection of the wound. Following surgical MC clients are advised to:
- Keep penis clean and dry at all times. Avoid disruption of the wound due to physical work, sports, or cycling.
- Keep penis in upright position at all times to reduce swelling and pain.
- Wear clean and well-fitting underwear to provide comfort and support.
- Mild swelling and pain is normal but visit the nearest clinic if swelling or pain worsens.
- Go to the VMMC clinic for removal of the bandage on day 2.
- Prepare saline water using 1 level teaspoon of course salt to 500 mL of drinking water (should taste like tears).
- Immerse circumcised organ in salty water after bandage removal at least once to three times a day for 15-20 minutes.
- Continue until the last stitch falls off. Stitches should not be removed as they will dissolve on their own.
- Do not engage in sexual activity or masturbate for at least six weeks, (the penis must heal completely before any sexual activity resumes). Complete recovery takes about six weeks.
- Do not apply any medication, ointment, cream, or antiseptic to the wound. Do not use traditional herbs on the wound. Keep the wound protected from any contamination with soil, dirt, or unclean water.
Counseling
It’s important to counsel MC clients on sexual practices immediately after the procedure, wound care, and erections. Let them know that early resumption of sex renders clients vulnerable to HIV acquisition if HIV negative. There is also a higher risk of transmitting HIV to partner if HIV positive.
Advise them to care for the wound as directed above, including immersing penis in salt water frequently (at least once a day) for surgical procedures only until the wound is healed. They should avoid application of herbal remedies, soil, dust, cow dung, and any medicinal application on wound.
Counsel clients that erections will be more frequent initially as a response to pain and the exposure of the glans. This should normalize as the wound heals. Reassure client that this has no relation with the need for sex. It usually happens in the morning and client should be advised to empty their bladder. If increased number of erections continues, advise client to stand on the floor bare footed as it can cool the blood supply to the lower limbs, which can relieve the problem.
Adverse Events
Quality assurance is key to prevent adverse event during circumcision and post operatively. Wound care should be emphasised pre-operatively and post operatively. Clients are encouraged to attend follow-up visits as instructed to monitor wound healing. Adverse events that require urgent attention are:
- Excessive bleeding
- Excessive pain
- Difficulty and pain when passing urine
- Pus or white liquid from the penis
- Excessive swelling of the penis, including haematoma
- Wound rupture
- Fever a week after circumcision
- Stiffness of the jaw
Referral
For HIV-positive clients, refer to HIV care and treatment services and always encourage mutual disclosure and partner testing. Provide follow-up care for ongoing risk reduction counselling, give information on correct and consistent use of condoms, demonstrate and provide condoms for sexually active clients, and promote early treatment and management of STIS.
For adolescents, encourage them to visit nearest youth centre/organisation for more information or services on Adolescent Sexual and Reproductive Health (ASRH). Discuss men’s supportive role in women and children’s health and emphasize behaviour changes, such as abstinence, being mutually faithful, and engaging in safer sex methods.
Male Circumcision and Adolescent Sexual and Reproductive Health (ASRH)
Male circumcision is an additional entry point for increasing male participation in sexual reproductive health (SRH) services, and in particular HIV prevention services, such as:
- Information and counselling on sexual intercourse, health problems related to the reproductive system, and safer sexual behaviours, such as:
- Reduction in the number of sexual partners
- Provision of male and female condoms and promotion of their correct and consistent use
- Being faithful to one sexual partner
- Delaying onset of sexual activities
- Diagnosis and management of STIs
- HIV testing and counselling (HTC) and referral for treatment, care and support
- Family planning services
For some adolescents and young adults, male circumcision intervention is the only available entry point to health care and services. It offers a window of opportunity to discuss ASRH, and for counselling on healthier lifestyles and approach to better health-seeking behaviour.
It is also important to add male circumcision as part of the topics discussed within the context of ASRH services. In this regard, there are clear and important linkages between male circumcision and ASRH and hence, where possible, it is of high importance to integrate these two services as much as possible.
-
Male Circumcision and Adolescent Sexual and Reproductive Health (ASRH) (5 min)
Male circumcision is an additional entry point for increasing male participation in sexual reproductive health (SRH) services, and in particular HIV prevention services, such as:
- Information and counselling on sexual intercourse, health problems related to the reproductive system, and safer sexual behaviours, such as:
- Reduction in the number of sexual partners
- Provision of male and female condoms and promotion of their correct and consistent use
- Being faithful to one sexual partner
- Delaying onset of sexual activities
- Diagnosis and management of STIs
- HIV testing and counselling (HTC) and referral for treatment, care and support
- Family planning services
For some adolescents and young adults, male circumcision intervention is the only available entry point to health care and services. It offers a window of opportunity to discuss ASRH, and for counselling on healthier lifestyles and approach to better health-seeking behaviour.
It is also important to add male circumcision as part of the topics discussed within the context of ASRH services. In this regard, there are clear and important linkages between male circumcision and ASRH and hence, where possible, it is of high importance to integrate these two services as much as possible.
- Information and counselling on sexual intercourse, health problems related to the reproductive system, and safer sexual behaviours, such as:
-
Knowledge Check (5 min)
-
Key Points (5 min)
- Male circumcision only offers partial protection (60%).
- Circumcised men can still get infected with HIV.
- Circumcised men, if HIV-positive, can infect their sexual partners.
- Need to prevent HIV and STI infection and seek early treatment.
- Discourage application of cow dung, soil, snuff, herbs on wound. Wash hands with soap thoroughly before and after handling the wound post circumcision.
- Promoting and providing safe male circumcision does not replace other interventions to prevent heterosexual transmission of HIV but provides an additional strategy.
- Male circumcision must be provided as part of a comprehensive national HIV prevention package and not offered in isolation.
- Male circumcision is an additional entry point for increasing male participation in HIV prevention services.
