Session 1: HIV Prevention
Occupational Exposure
In this session, we will discuss the importance of practicing preventive health behaviors, the universal standard precautions to prevent occupational exposure to bloodborne pathogens, including HIV and how to treat exposure with post-exposure prophylaxis (PEP).
Learning Objectives
By the end of this session, you will be able to:
- Describe the HIV preventive strategies.
- Describe prevention and control strategies of HIV and other infections in the workplace.
- Outline key elements of infection prevention and control (IPC).
- Describe PEP.
Learning Activities
-
Introduction to HIV Prevention (5 min)
Sponsored by UNFPA, UNAIDS, and the Zimbabwean Ministry of Health and Child Welfare, researchers explored the reasons for the decline in HIV prevalence and examined what lessons can be learned and replicated. The study pinpointed several key factors in Zimbabwe’s success, which include changes in sexual behaviour, personal experiences related to the high AIDS mortality in the country, and correct information about HIV transmission and prevention.

The most significant cause of the decline was seen to be the reduction in multiple sexual partnerships, with a 30% fall in men reporting extra-marital relationships. This can be partly attributed to the success of HIV prevention programmes, through mass media and based on interpersonal communication through the church, work place, friends, and family. Such programmes stressed the protective effect of having fewer partners and promoted condom use during casual sex. “The behaviour changes associated with the HIV decline appear to be largely the result of people increasingly talking about HIV and its link to risky sexual behaviour,” said Clemens Benedikt, HIV prevention manager in the UNFPA office in Zimbabwe and one of the authors of the report.
Zimbabwe provides a clear example of the profoundly positive results that behaviour change can bring about an effective AIDS response. Despite the growing availability of antiretroviral medicines, Zimbabwe's experience highlights the importance of prevention in an effective and sustained response to HIV. According to UNAIDS, globally there are still two new HIV infections for every one person starting treatment, and prevention efforts make up only around 20% of AIDS-related spending in low- and middle-income countries.
In this session, we will discuss key preventive strategies and ways you as a health care worker can educate your clients about the importance of combination prevention strategies to reduce new HIV infections. These include:
- Social behaviour change communication
- Medical male circumcision
- Test and treat for HIV and STIs
- STI Prevention and management
- Antiretroviral therapy (ART)
- Prevention of mother-to-child transmission
Public health education is important and should include messages about the nature of HIV and other STIs, the dangers of infection, complications, modes of transmission, methods of prevention, and treatment. As you work with clients it will be important to promote safer sexual behaviour and encourage abstinence.
Abstinence means not engaging in any sexual activity in which there is a direct or theoretical risk of exposure to blood, semen, or vaginal fluid.Refraining from sexual intercourse is the best way to prevent transmission of HIV and other sexually transmitted infections. You’ll also want to encourage your clients to delay their first sexual experience, avoid situations that may promote casual sexual liaisons and avoid multiple concurrent partnerships. It is also important to educate clients on the proper use of condoms. Using condoms correctly and consistently during sexual intercourse can greatly reduce the chances of acquiring or transmitting HIV and other sexually transmitted infections.
Other effective promotion techniques include:
- Early STI-care seeking
- Good STI care-seeking behavior
- Making STI services accessible and available
- Testing and counseling for HIV
- Increasing access to HIV testing and counseling
- Scaling up voluntary counseling and testing (VCT) and provider-initiated testing and counseling (PITC)
- Prevention of mother-to-child transmission of HIV
- Strengthening PMTCT activities
- Prioritising the provision of lifelong ART for pregnant and breastfeeding women
- Encouraging voluntary medical male circumcision (VMMC)
- Promoting antiretroviral treatment (ART) for all PLHIV, early access to ART, and ART in sero-discordant couples
-
Occupational Exposure/IPC (5 min)

The greatest risk for accidental exposure to an infectious agent is with the handling of sharp objects that have been used on infectious patients. Health care workers should always be aware that blood and secretions from patients are potentially infectious. Therefore, your health facility should ensure the continuous supply of educational materials, disposable syringes and needles, and proper sharps bins. All personnel should be taught how to safely handle and dispose of sharp objects, which includes not recapping needles, using proper “sharps bins” for disposing of sharps, and taking care when performing procedures.
Standard Precautions
These are routine infection control precautions that should apply to ALL patients, health care workers and visitors in all health-care settings.
Standard precautions involve the use of protective barriers, such as gloves, gowns, aprons, masks, or protective eyewear, which can reduce the risk of exposure of the health care worker’s skin or mucous membranes to potentially infectious materials. Standard precautions are designed to prevent transmission of HIV, hepatitis B virus (HBV), and other bloodborne pathogens when providing health care. Under standard precautions, the blood and certain body fluids of all clients are considered potentially infectious for HIV, HBV, and other bloodborne pathogens.
Standard precautions are infection-control measures that reduce the risks of blood‐borne pathogens including HIV in health care settings. These are routine infection control precautions that should apply to all patents, health care workers and visitors in all health-care settings.Standard precautions should be observed with every client, regardless of whether the service provider thinks the client might be infected with HIV, hepatitis, or any other blood‐borne pathogen. Maintaining standard precautions with every client is important because until laboratory tests are conducted, it is not possible to tell who is infected with pathogens, such as HIV and hepatitis viruses. Some infections have a “window period” following exposure, when laboratory test results are negative even though the person is infected, and infected individuals themselves may not even be aware of their status.

Prevention of occupational exposure in health facilities
Health facilities should implement standard precautions for the prevention of exposure to potentially infectious material. The programme should include the training of all employees in the handling and disposal of infectious material and all personnel should be made aware of the risks involved in improper handling of such material, and the steps necessary for preventing exposure should be clearly displayed in posters.
Blood and secretions from clients may be infectious. Simple contamination of unbroken skin is not a significant risk, but contamination of intact mucous surfaces of the mouth and eyes is. The health facility should ensure the continuous supply of personal protective equipment, educational materials, disposable syringes, needles and sharps containers. Health facilities should also ensure the availability and accessibility of medicines for post-exposure prophylaxis (PEP).
Next, we will discuss the key elements of infection prevention and control.
-
Hand Hygiene (5 min)
Hand hygiene is one of the single most important practices to reduce the transmission of infectious agents in healthcare settings and is an essential element of standard precautions. The term “hand hygiene” includes both hand washing and hand decontamination.
In the absence of visibly soiled hands, approved alcohol-based products for hand disinfection are preferred over antimicrobial or plain soap and water because of their superior microbicidal activity, reduced drying of the skin, and convenience. Appropriate accessible facilities for hand hygiene should be provided for all health workers, patients, and visitors.
Hand washing should be done:
- When arriving at your facility and before going home
- Before and after direct contact with each client
- Before performing procedures on clients
- Before and after putting on and taking off gloves
- After contact with inanimate objects in the immediate vicinity of the client
- After using the toilet
There are four types of hand hygiene.Tap on the tabs below to learn about each one.
Routine hand washing
Simply washing hands with plain soap and running water removes transient micro-organisms and soil, blood or other organic material from hands and is appropriate in most situations when hands should be washed, including after arriving at work.
Antiseptic and running water
Hand washing with antiseptic and running water removes transient micro-organisms and soil and kills or inhibits the growth of resident micro-organisms and reduces the risk of infections in high-risk situations, such as:
- When there is heavy microbial contamination.
- Before performing invasive procedures, (e.g., the placement and care of intravascular devices, in dwelling urinary catheters).
- Before contact with patients who have immune defects, damage to the integumentary system/skin (e.g., burns, wounds) and percutaneous implanted devices.
- Before and after direct contact with patients who have antimicrobial resistant organisms.
Alcohol-based hand rub
Alcohol is one kind of antiseptic hand rub, which kills or inhibits the growth of most transient and resident micro-organisms but does not remove micro-organisms or soil. It can be used when hand washing with soap and running water is not possible, as long as hands are not visibly soiled with dirt, blood, or other organic material.
Surgical hand rub
Scrubbing with antiseptic before beginning surgical procedures will help prevent the growth of micro-organisms for a period of time. It reduces the risk of infections to the patient if the gloves are damaged during the procedure.
-
Hand Hygiene (5 min)
Watch the short video to see the proper way to perform hand hygiene.
-
ABHR (5 min)
Watch the short video to see the proper way to perform alcohol-based hand rub.
-
Personal Protective Equipment (5 min)
Personal protective equipment (PPE) refers to a variety of barriers used alone or in combination to protect mucous membranes, airways, skin, and clothing from contact with infectious agents. The selection of PPE (whether gowns, gloves, aprons, masks, or respirators) is based on the nature of the interactions and/or the likely mode(s) of transmission in the provision of care.
It is important that PPE is used effectively, correctly, and at all times where contact with blood and body fluids of patients may occur. Continuous availability of personal protective equipment and adequate training for its proper use are essential.

Health workers should routinely assess the risk of exposure to body substances or contaminated areas before any anticipated health care activity and select PPE based on the assessment of risk. Staff must be aware that use of personal protective equipment does not replace the need to follow basic infection control measures such as hand hygiene. Also, incorrect use of personal protective equipment increases the risk of contracting healthcare-associated infections.
PPE should be taken off immediately after use. The risk of self-contamination is very high when removing PPE. When PPE is removed, there is potential for contamination from PPE to hands, mucous membranes, clothing, and skin. PPE should be removed slowly and carefully, then discarded in the appropriate waste bin.
The following principles apply when removing PPE:
- Ensure the outside of PPE does NOT touch skin or any part of the body.
- Take off the outermost PPE first.
- Perform hand hygiene after PPE is removed.
-
Injection Safety (5 min)

The goals of injection safety are to reduce unnecessary injections, improve protection against the acquisition of infections during necessary procedures, and ensure the safe management of sharps. Safe injection practices shall be given a priority in all health facilities to reduce the spread of bloodborne pathogens including HIV and hepatitis B and C. Sharps disposal should be efficiently managed using methods that are safe for staff, the community, and the environment.
A standardized guide on injection safety should be in place for all staff working in clinical, diagnostic, administration, education, and cleansing departments within the health sector both in public and private health care settings and related educational institutions. All pre-service health professionals should be instructed on safe injection practice with hands-on practice training in the clinical area.
Procurement and supply chain management should ensure the provision of medical supplies including safe syringes and sharps containers or boxes. On-the-job support, supervision, and behaviour change exercises to improve practice should be implemented. Recording and reporting systems for safe injection practices should be in place, including the use of a register to record needle-stick injuries as part of the health facility post exposure policy (PEP). Records on needle-stick injuries exposure to bloodborne pathogens should be regularly monitored by the facility infection control committee and used to direct training interventions where required.
Safe injection techniques include the following:
- Not recapping needles. Do not recap needles for disposal whenever possible. If recapping is required for the procedure being done, you must use tongs, a recapping device or one-hand scoop method to recap the needle.
- Cleaning or disposing of instruments safely.
- Using needles or scalpel blades on one client only.
- Always warning clients when they are about to get an injection.
- Handling instruments safely.
- Disposing of single use needles (hypodermic and suture) and sharps (scalpel blades, lancets, razors, and scissors) in puncture and leak-proof sharps boxes.
- Applying proper surgical practice: Using needle holders to avoid using fingers for needle placement.
- Properly processing instruments, devices, and equipment used during invasive procedures. After each use, decontaminate and clean with high-level disinfect or sterilize all devices and equipment.
-
Respiratory Hygiene and Cough Etiquette (5 min)

Respiratory hygiene and cough etiquette are source control measures that are now considered as part of standard precautions. Health care workers must be aware of the different routes of transmission of respiratory pathogens. For example, it’s important to know the respiratory route for tuberculosis and the respiratory and contact route for influenza viruses. Ensuring quality practice in reducing the transmission of these pathogens should include:
- Education of health workers, patients, and visitors
- Promotion of cough etiquette for coughing patients
- Improving supply of hand hygiene resources including disposable hand paper towel and PPE
- Triaging coughing patients
- Ensuring spatial separation of persons with acute febrile respiratory symptoms
-
Environmental and Linen Management (5 min)
Environmental Management and Cleaning
To minimize the transmission of microorganisms from equipment and the environment, adequate methods for cleaning, disinfection, and sterilization must be in place. Written policies and procedures that take into account the functions of each section and the degree of risk of exposure to healthcare-associated infections (HAIs) must be developed for each facility and updated on a regular basis. For airborne transmissions, ensure adequate circulation of indoor air through the opening of windows.
Linen Management
Used linen should be handled, transported, and processed in a manner which prevents skin and mucous membrane exposure and contamination of clothing and avoids transfer of pathogens to other patients and/or the environment. Written procedures must be in place to describe the process of separation at point of generation and sluicing of linen; colour coding of linen bags, as well as the laundering processes used by the facility. Those handling linen at all stages of processing must use appropriate PPE.
-
Waste Management (5 min)

Waste generated in health settings is a potential reservoir of pathogenic organisms and requires appropriate handling. The Ministry of Health and Child Care bears overall responsibility for the regulation of potentially infectious health care facility waste. Local government or government agencies that ensure public health and environmental regulatory compliance have overall responsibility for local facilities.
Each facility generating waste has a primary responsibility to manage its waste on daily basis. Each health facility is therefore responsible for developing a waste management plan and plan for the management of all types of waste generated by the facility; ensuring that all health care workers are trained in the requirements of the plan and the care safety procedures and appropriate records are maintained as described in the national IPC guidelines.
Safe handling and disposal of waste
Use systems for safe waste collection and disposal. Collect waste sorted by type: general waste, medical waste, and hazardous chemical waste.
Use the following guidelines when handling waste:
- Deposit waste in leak-proof containers.
- Wear heavy duty gloves.
- Carry solid contaminated waste to the disposal site in covered containers.
- Burn or bury contaminated solid waste.
- Carefully pour liquid waste down a drain or flushable toilet.
- Wash hands, gloves, and containers after disposal of infectious waste.
-
Reprocessing (5 min)
Appropriate cleaning, disinfection, and sterilisation of patient equipment are important in limiting and/or preventing the transmission of micro-organisms. Contaminated medical equipment and instruments can transmit infection to both patients and staff. The equipment and instruments must be effectively decontaminated after each use using a process of cleaning and then disinfecting or sterilising as appropriate. All reusable instruments that are used during a specific procedure on a patient should be sterilised or disinfected.
It is advisable to identify the different types of instruments in use within each health facility according to their use. This will help determine what steps are needed for IPC management, which can then be described in standard operating procedures. Quality assurance and quality control procedures should be in place to ensure that procedures are adhered to and the processes are functioning correctly.
-
Knowledge Check (5 min)
-
Reading: Post-Exposure Prophylaxis (PEP) (5 min)

Although occupational transmission of HIV to health care workers is extremely rare, each facility should have a system for responding when a health care worker is injured by a needle-stick, sharp object used on a client and/or exposed to an infectious disease. Specific post-exposure policies are needed for a number of infectious diseases, including human immunodeficiency virus (HIV), viral hepatitis, pandemic influenza, severe acute respiratory syndrome (SARS), and tuberculosis.
Post-exposure prophylaxis (PEP) is a way to prevent HIV infection after a recent possible exposure to the virus. PEP means taking antiretroviral medicines (ART) after being potentially exposed to HIV to prevent becoming infected. PEP should be used only in emergency situations and must be started within 72 hours after a recent possible exposure to HIV. You should report your exposure to your supervisor and seek medical attention immediately.
The following types of exposures should be considered for post-exposure prophylaxis (PEP):
- Needle-stick injury or injury with a sharp object used on a client
- Mucosal exposure of the mouth or eyes by splashing fluids
- Broken skin exposed to a small volume of blood or secretions, such as may occur with sexual abuse
- Human bite
- Sexual assault (rape)
- Unprotected sex by consent with an infected partner
The medications used in PEP depend on the exposure to HIV. The exposure can be classified as high risk or low risk for HIV infection. Tap on each tab to read more:
Low risk
- Solid, such as surgical needle, superficial exposure on intact skin
- Small volume (e.g., drops of blood) on mucous membranes or non-intact skin
- Source client asymptomatic or with VL less than 1 500 copies/mL
High risk
- Large-bore needle, deep injury
- Large-volume splash on mucous membranes or non-intact skin
- Source client symptomatic or with high VL levels
Procedure for Injury with a Sharp Object
In the event of an injury with a sharp object, such as a needle or scalpel that has been used on a patient, or in the event of a mucous surface being contaminated with blood or secretions from a patient the following steps should be followed:
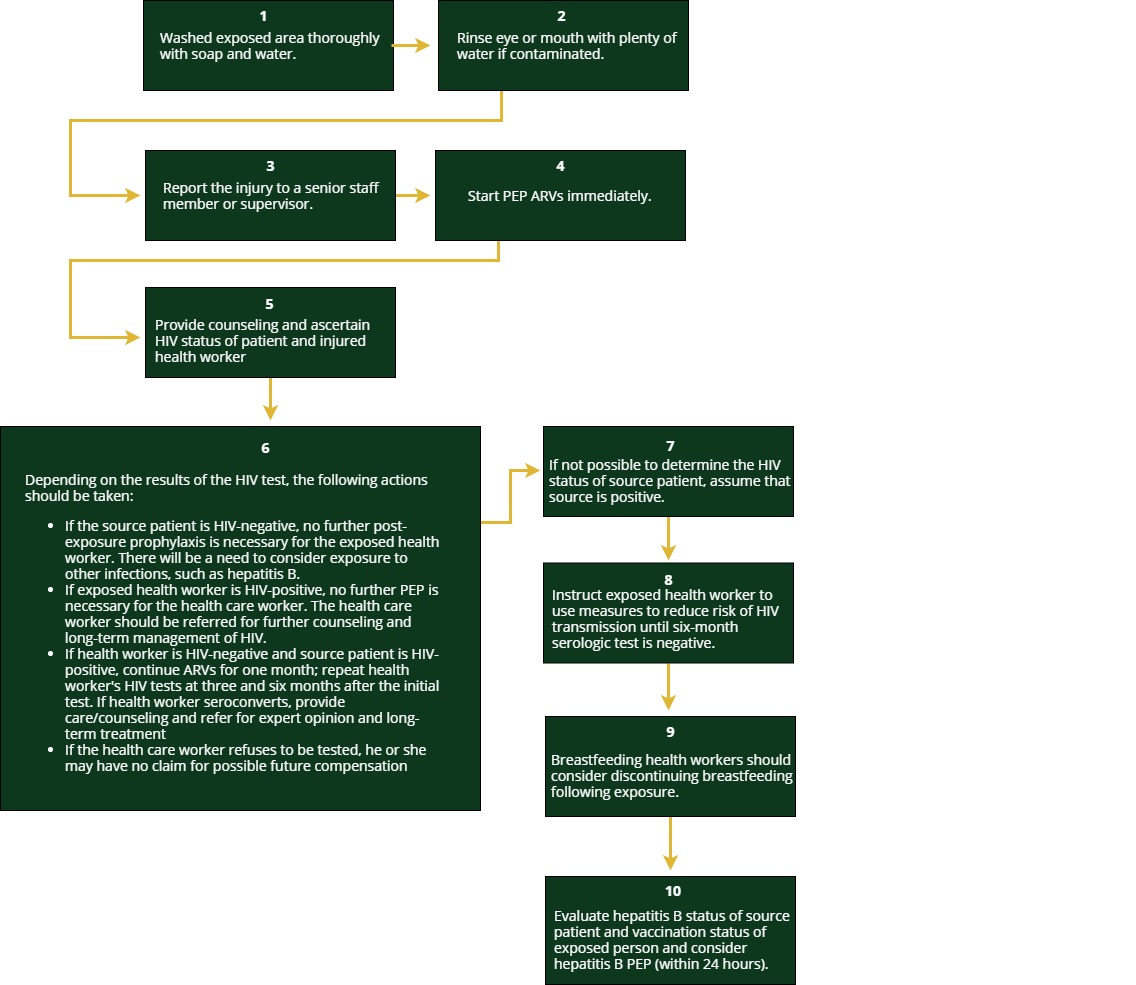
Antiretroviral Drugs to Be Used in Post-Exposure Prophylaxis
In people who have been accidentally exposed to HIV through needle-stick inoculation or through contamination of mucous membranes by secretions, it has been shown that administration of antiretroviral medicines (ARVs) within 72 hours of exposure reduces the likelihood of HIV infection being transmitted.
Immediately after exposure, all exposed health workers should take the following regimen for one month:
- Tenofovir 300 mg orally once daily plus
- Lamivudine 300 mg orally once daily plus
- Atazanavir (300 mg)/ ritonavir 100 mg orally once daily
This regimen is continued for 28 days. If the source patient is HIV-negative, no further PEP is necessary. Exposure to other infections such as hepatitis B will need to be considered.
Management Procedures
Baseline testing of exposed health care workers should be performed for HIV and encouraged to test for HBV exposure.Tap to review a flow chart of the specific PEP management procedures.
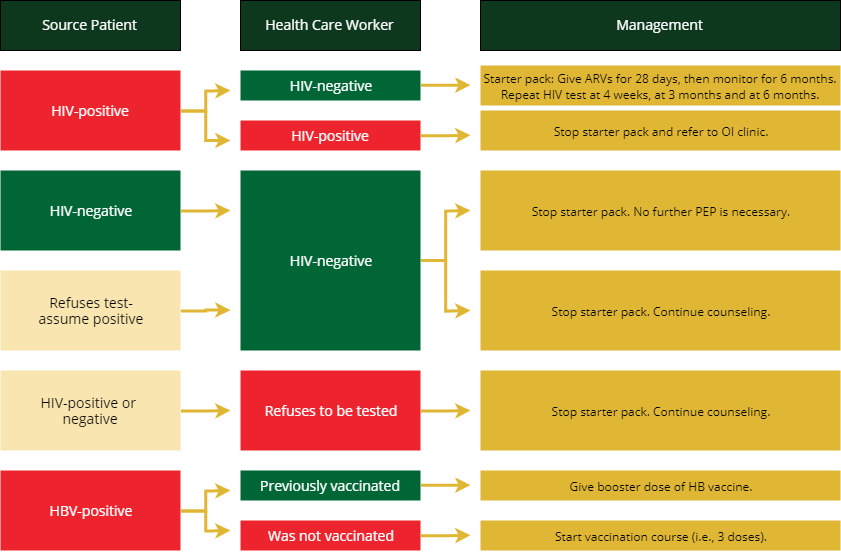 Source: National Infection Prevention and Control Guidelines in Zimbabwe May 2015
Source: National Infection Prevention and Control Guidelines in Zimbabwe May 2015 -
Knowledge Check (5 min)
A doctor from a local hospital is doing a caesarean section on a woman who is HIV-infected. The woman is not on antiretroviral therapy. The doctor accidentally pricks himself with the suture needle while suturing the uterus and he starts to bleed profusely. The doctor does not know his own HIV status.
-
Key Points (5 min)
- Standard Precautions are routine infection control precautions that should apply to all patients, HCW and visitors in all health-care settings.
- All blood and body fluids should be treated as infectious.
- Hand hygiene is the single most important measure to prevent transmission of infection and is the cornerstone of infection prevention.
- Before undertaking any activity or procedure, you should assess the risk of exposure to blood or body fluids. If there is a possible risk, you should wear the PPE that provides appropriate protection against the risks associated with the procedure or task being undertaken.
- Use sharps with caution: Do not recap needles and dispose in puncture proof receptacles immediately after use.
- PEP should be considered if you have had a recent possible exposure to HIV at work.
- PEP must be commenced as soon as possible or within 72 hours of exposure to HIV.
- PEP should be considered for non-occupational exposure to HIV such as sexual assault.
