Session 8: Diagnosis and Management of Common OIs
Clients infected by HIV have an increased risk of developing several infections because of their impaired immune systems. The important opportunistic infections are highlighted under the WHO clinical staging section. In this session, we will take a deeper look at opportunistic infections and HIV-related malignancies and how to apply the guidelines for managing these common chronic illnesses among people living with HIV/AIDS. Finally, we will discuss how to prescribe cotrimoxazole and fluconazole prophylaxis to infants, children, adolescents and adult clients according to the national guidelines.
Learning Objectives
By the end of this session, you will be able to:
- Describe the diagnosis and management of the Pneumocystis jiroveci (carinii) pneumonia (PCP) in adults, adolescents and children.
- Describe the diagnosis and management of pneumonia in adults.
- Describe the diagnosis and management of serious bacterial infections (including pneumonia) in children.
- Discuss nausea and vomiting in PLHIV.
- Describe the causes and types of diarrhoea in PLHIV.
- Explain treatment of diarrhoea in PLHIV.
- Describe the diagnosis of cryptococcal meningitis.
- Describe the management of cryptococcal meningitis.
- Describe the diagnosis and management of the following oral and dermatological conditions: candidiasis, oral hairy leukoplakia, aphthous ulcers, herpes simplex type 1 and 2, Herpes zoster, sebhorreic dermatitis, and fungal infections (apart from candidiasis).
- Describe the diagnosis and management of the following HIV-associated malignancies:
- Kaposi sarcoma
- Lymphomas
- Discuss how to prescribe cotrimoxazole prophylaxis to appropriate infant, child, adolescent, and adult clients.
Learning Activities
-
Pneumocystis Jiroveci (Carinii) Pneumonia (PCP) (5 min)

Pneumocystis jiroveci (carinii) pneumonia (PCP) is a fungal infection of the lungs caused by the fungus Pneumocystis jirovecii (formerly carinii). This fungus is common in the environment and rarely causes illness in healthy people. However, it can cause a lung infection in people with a weakened immune system due to HIV/AIDS.
PCP is a WHO clinical stage 4 condition. The risk of PCP is significantly reduced by giving cotrimoxazole prophylaxis to clients in WHO clinical stages 2-4 or with CD4 counts less than 350.
Tap on the tabs below to learn about the diagnosis and management in adults and children.
In Adults
Diagnosis
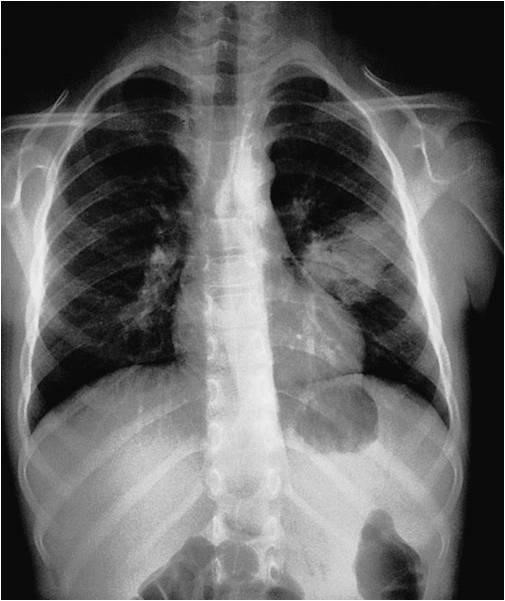
The diagnosis of PCP is essentially a clinical one, and the CXR may be normal (in early disease) or may show patchy infiltrates or ground glass opacification in both middle zones. Symptoms and signs include:
- Progressive shortness of breath (especially on exertion)
- Cough that is dry or productive of scanty clear or white sputum
- Fever
- Central chest pain

Treatment
Standard treatment involves cotrimoxazole (CMZ) 1920 mg three times a day for 21 days.
In severe cases (with tachypnoea [>30/min], cyanosis of the nail beds and tongue) hospital admission and oxygen therapy may be required. In addition to standard treatment, prednisolone should be given 40 mg twice a day for five days, then 40 mg daily for five days. After ten days, 20 mg should be taken once a day for five days.
Prophylaxis (primary or secondary)
Cotrimoxazole provides protection against bacterial infections and toxoplasmosis and keeps clients out of hospital. Conventionally, 960 mg once daily or three times a week has been used. Alternatively, 480 mg daily may be as efficacious. Other forms of prophylaxis include nebulised pentamidine (300 mg/month via jet nebuliser) or dapsone.
In Children
Diagnosis
The diagnosis of PCP is essentially a clinical one and may be associated with other HIV-related symptoms, including oral thrush, lymphadenopathy, and/or weight loss. The onset can be abrupt or insidious and may be afebrile or present with a low-grade fever.
The condition is characterized by marked respiratory distress, manifested by the following signs:
- chest in-drawing
- cyanosis
- the inability to drink
- marked tachypnoea
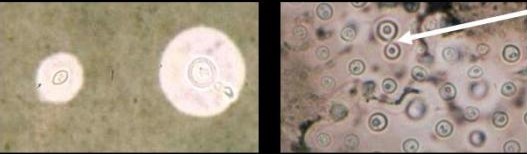
Auscultation of the chest may reveal a clear chest or diffuse fine crepitations. Pulse oximetry will show severe persistent hypoxia with oxygen saturation levels commonly below 90%. The CXR may be normal or show bilateral diffuse parenchymal infiltrates with a “ground glass” or reticulogranular appearance. Fungal elements of Pneumocystis Jiroveci organisms may be identified in stains of induced sputum or broncho-alveolar lavage.
Management
Therapy must be initiated promptly along with treatment for bacterial pneumonia. (Some centres use ceftrioxone for treatment of bacterial pneumonia).
- Give a high-dose CMZ 20 mg/kg of trimethoprim per day intravenously OR orally given in three to four doses for 21 days.
- Add prednisone at 2 mg/kg/day for 7-14 days if child is in severe respiratory distress.
- Additional supportive management is required such as:
- Oxygen therapy
- Maintenance and monitoring of hydration
- Pain relief (paracetamol to be used with caution if the infant is below three months of age)
- Treatment for bacterial pneumonia continued, and secondary prophylaxis provided after the acute episode
-
Pneumonia in Adults (5 min)
Bacterial lower respiratory tract infections are more frequent and severe in immunosuppressed clients with HIV. HIV-infected clients are 20 times more likely to acquire streptococcal infections. Recurrent bacterial pneumonias may be the first indication of HIV infection, and all clients with pneumonia should be offered an HIV test.
The causes of bacterial pneumonia in persons with HIV include:
- Streptococcus pneumonia
- Haemophilus influenza
- Klebsiella pneumonia
- Staphylococcus aureus
- Pseudomonas aeruginosa
Diagnosis
The diagnosis of bacterial pneumonia depends on the symptoms and signs (same as HIV-negative individuals) and includes the following:
- Cough
- Fever
- Myalgia
- Headache
- Loss of appetite
- Chest pain
- Shortness of breath
The presentation may be variable and includes classic lobar pneumonia, bronchopneumonia, or with unresponsive and atypical pneumonia. CXR may reveal lobar consolidation, patchy consolidation, diffuse lung infiltrates, or atypical changes including cavitating disease—cavities more common with Klebsiella or Staphylococcus. The causative agent may be identified by sputum examination.
Treatment
Always exclude TB and PCP. If the client’s condition does not warrant admission, the drug of choice is amoxycillin, given three times daily for 7 days. The client must be advised to return earlier to clinic if symptoms worsen. Admission and close monitoring is mandatory if any of these signs are present:
- Respiratory distress (RR>30)
- Cyanosis
- Pulse above 124/min
- Temperature above 40° or below 35°
- Altered mental state
- Elderly (above 65 years)
- Presence of chronic lung disease, chronic renal failure, chronic cardiac failure, or chronic liver disease
Admitted clients must receive IV antibiotics and oxygen therapy where necessary.
-
Serious Bacterial Infections (Including Pneumonia) in CShildren (5 min)

HIV-infected children frequently suffer from serious bacterial infections. These include:
- Empyema
- Pyomyositis
- Bone or joint infection
- Meningitis
The choice of antibiotic for the management of these infections depends on the organism and the type of infection. Standard treatment protocols should be followed when managing these infections. Children whose immune systems are not seriously compromised can be expected to respond to normal courses of antibiotic therapy, but those that are severely immunocompromised may require intravenous administration and prolonged duration of therapy.
-
Knowledge Check (5 min)
-
Common Gastro-Intestinal Tract (GIT) Diseases (10 min)
Many people living with HIV will experience some nausea when commencing ARVs. They should be reassured that this is a self-limiting side effect that usually resolves within 1 to 2 weeks. If it persists and is an obstacle to the client taking their ART, the client should report to the health care worker.
It is very important to discuss the topic of nausea and vomiting with your clients as these symptoms may cause the client to interrupt their medication. Anti-emetic medications may be necessary in order to assist the clients to adhere to ART.
The causes of the nausea or vomiting should be identified and may include any of the following:
- Side effects of medication (ART or OI medications)
- Disease in the liver, pancreas or small intestine, such as hepatitis
- Disease in the in the CNS, such as cryptococcal meningitis
- Alcoholism
If the client vomits within 30 minutes of taking the ARVs, he/she should be counselled to wait at least 30 minutes and repeat the medication after eating a small amount. All the ARVs except didanosine can be taken with food. If he/she vomits after 30 minutes have passed since taking the medication, there is no need to repeat it unless the medication is visible in the vomitus.
Diarrhoeal Disease
Diarrhoeal disease is the passing of more than three loose stools per day. The incidence of diarrhoea increases as the CD4 decreases.
Tap the tabs below to review the differences between small bowel and large bowel diarrhea.
Features of diarrhoea originating from small bowel (enteritis)
- Large volume watery stools
- More often associated with dehydration, electrolyte disturbances, malabsorption, low-grade fevers and nausea
- If abdominal pain is present it is usually in the peri-umbilical area
Features of diarrhoea originating in the large bowel (colitis)
- Frequent
- Small volume stools that may contain blood, mucus or pus
- May be accompanied by symptoms of proctitis and lower quadrant abdominal pain
Causes
Major enteric infections may be associated with bacteraemia, are usually of greater severity, invasiveness, chronicity and often recur. The symptoms are usually cramping abdominal pain, tenesmus, bloating, and nausea. Diarrhoea caused by C. difficile infection is associated with recent antibiotic usage and may be difficult to treat. It tends to recur more often in HIV-infected people. Treatment is metronidazole or oral vancomycin.
The major enteric and bacterial pathogens that cause diarrhoea in PLHIV are listed below.
Enteric Pathogens Bacterial Pathogens - Isospora
- C. difficile
- Cryptosporidia
- Cytomegalovirus
- Microsporidia
- Adheren bacteria
- MAC
- Campylobacter
- Clostridium difficile
- Shigella
- Adherent E. coli
- Salmonella
- MAC
Types of Diarrhoea in PLHIV
Tap the tabs below to review the types of diarrhoea.
Acute Diarrhoea
3 or more loose stools per day occurring for 3 to 10 days
Causes
- Enteric pathogens as listed above;
- Medications: Protease Inhibitors (Nelfinavir, any Ritonavir-containing regimen) and DDI
- Idiopathic (in 25-40% of cases)
The diagnosis is made on stool analysis:
- Micro
- Culture and sensitivity
- AFB
- C. difficile toxin
- blood culture for salmonella species and mycobacterium avium complex (MAC)
Treatment
- Guided by stool results
- Empirical therapy using Cotrimoxazole,
- Ciprofloxacin with or without
- Metronidazole is often used
Chronic Diarrhoea
Lasting for more than 30 days and usually indicates advanced HIV infection.
Diagnosis
- Cryptosporidia (10-30%)
- Microsporidia (15-30%)
- CMV colitis (15-40%)
- MAC (10-20%)
- Isospora
- Giardia
- Entamoeba (1-3%)
- Cyclospora (‹1%)
- other - KS, lymphoma, TB, idiopathic (after endoscopy—20-30%)
Treatment
- Rehydration
- Diet
- Anti- diarrhoeal agents
- Stool MCS
- Treatment of the specific cause
-
Knowledge Check (5 min)
-
Cryptococcal Meningitis (10 min)
Cryptococcal meningitis (CM) is the most common cause of community-acquired HIV-associated meningitis in sub-Saharan Africa. It is associated with high rates of morbidity and mortality and is uniformly fatal if left untreated. Clients initiating ART with undiagnosed cryptococcal disease are at higher risk of early mortality than clients who are pre-emptively diagnosed and treated for cryptococcal disease. Therefore, all clients initiating ART should be clinically screened for evidence of symptomatic cryptococcal disease.
Diagnosis

Typical symptoms and signs of meningitis, such as headache or meningism, are often absent. Presenting symptoms and signs include:
- Fever
- Headache
- Nausea
- Vomiting
- Cognitive dysfunction (irritability, behavioural changes, somnolence, or even psychosis)
- Focal signs and seizures may be present
- Altered mental status
Screening Tests
All those who screen positive should be referred for further diagnostic workup for meningitis.
Screening of asymptomatic ART naïve individuals with CD4 count ‹100 cells/mm3 is recommended and should be done with a cryptococcal neoformans antigen test (CrAg) using latex agglutination (LA) tests or lateral flow assays (LFA) on serum, plasma, or CSF.
A lumbar puncture should be offered to individuals who screen positive for cryptococcal antigen, as a positive cryptococcal antigen may precede the onset of clinical cryptococcal meningitis by many weeks.
Diagnostic Tests
The most significant marker of poor prognosis is persistently raised intracranial pressure. A high CSF pressure, above 20 cm water, is often a clue to the diagnosis. A positive culture for Cryptococcus neoformans gives a definitive diagnosis, but this may take up to two weeks. A positive India ink smear on microscopy is often helpful but may be too insensitive to exclude the diagnosis. The CSF cryptococcal antigen (CRAG) test has a sensitivity of 95%. The presence of cryptococcal antigen in the serum is a good marker of HIV associated CM.
Treatment
Treatment must be with amphotericin B-based regimens. Ideally, amphotericin B must be combined with flucytosine. However, flucytosine is typically not available in resource limited settings, including Zimbabwe.
Combination therapy with amphotericin B and fluconazole is strongly recommended. In the absence of amphotericin B, high-dose fluconazole can be used as alternative therapy. Therapy is characterized by the following phased approach:
Cryptococcal Meningitis Prophylaxis
Fluconazole is used in the prevention of cryptococcal disease, either as a primary prophylaxis in preemptive therapy, or as secondary prophylaxis after an individual has been diagnosed with cryptococcal infection and received appropriate treatment. It should be given to all PLHIV who have been diagnosed with CM until they have reached a state of immune reconstitution.
Recommended Therapy
Timing of ART for individuals with asymptomatic cryptococcal antigenemia is unknown. It is recommended to initiate ART 2 to 4 weeks after initiation of antifungal therapy in individuals who screen positive for serum CrAg without any evidence of disseminated cryptococcal meningitis.
Tap the tabs below to learn more about the preferred and alternative therapy for cryptococcal meningitis.
Preferred
Treatment Phase Regimen Duration of therapy Induction Phase Amphotericin B 0.7-1 mg/kg/day IV + Fluconazole 800 mg orally once daily 2 weeks Consolidation Phase fluconazole 800 mg orally once daily 8 weeks Maintenance or Secondary Prophylaxis fluconazole 200 mg orally once daily Until CD4 count >200 for 6 months Alternate
Treatment Phase Regimen Duration of therapy Induction Phase fluconazole 1200 mg orally daily 2 weeks Consolidation Phase fluconazole 800 mg orally daily 8 weeks Maintenance or Secondary Prophylaxis fluconazole 200 mg orally once daily Until CD4 count >200 for 6 months Treatment Decisions for Asymptomatic Cryptococcal Disease
Result Treatment Decision Serum CrAg Negative No lumbar puncture necessary.
No fluconazole required.
Initiate ART.
Serum CrAg Positive If available recommend lumbar puncture.
- If CSF CrAg positive, manage for cryptococcal meningitis
- If CSF CrAg negative, treat with fluconazole, starting with 800 mg orally once daily for two weeks, followed by fluconazole 400 mg orally daily for eight weeks, followed by maintenance therapy with fluconazole 200 mg orally daily until CD4 > 200 cells/mm3 for six months
-
Knowledge Check (5 min)
Indicate whether the following statements regarding CM are true or false.
-
Case Study: Takunda (5 min)

Takunda is a 43-year-old man who started ART three weeks ago at your hospital. His baseline CD4 is 42 and no other investigations were done. He started on Tenolam-E and cotrimoxazole and presents with gradually worsening headache on and off for one month. He is relieved by paracetamol at first, but now the stronger pain-killers are not effective.
Results of a lumbar puncture showed numerous Cryptococcus neoformans on India ink stain.
-
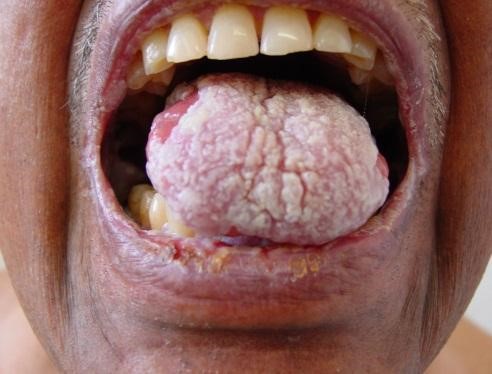
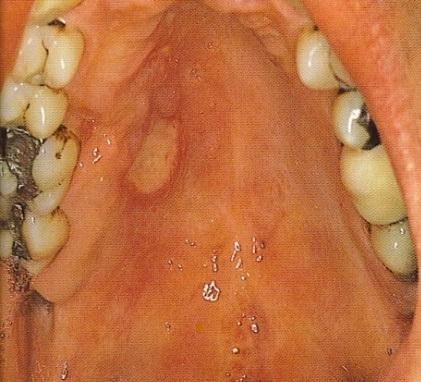
Common Oral and Dermatological Conditions (15 min)
Oral and cutaneous lesions are commonly found in children, adolescents, and adults with HIV infection. Frequently, the diagnosis of HIV infection is made from examination of the oral cavity and the skin. Lesions can be caused by infectious agents, neoplastic disease, or inflammatory conditions.
To view the most common oral manifestations found in adults, tap the arrows below.
-
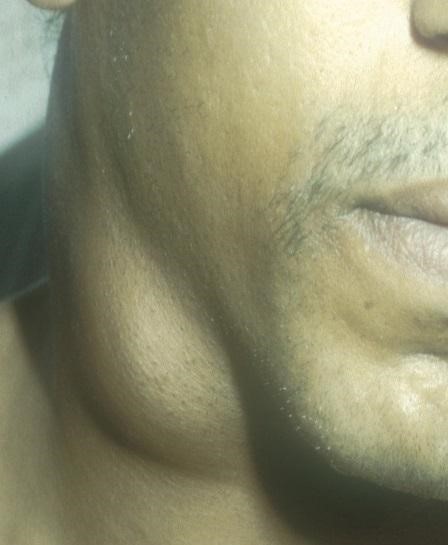
HIV-Associated Malignancies (10 min)
People infected with HIV have a substantially higher risk of some types of cancer compared with uninfected people of the same age. The general term for these cancers is “HIV-associated cancers.” Three of these cancers are known as “acquired immunodeficiency syndrome (AIDs)-defining cancers” or “AIDS-defining malignancies”: Kaposi sarcoma, aggressive B-cell non-Hodgkin lymphoma and cervical cancer.
Kaposi’s sarcoma (KS) is a systemic disease that can present with cutaneous lesions with or without internal involvement. KS can involve the oral cavity, lymph nodes, and viscera. Classic KS tends to be indolent, presenting with erythematous or violaceous patches on the lower extremities.
Tap the arrows below to view all images.
-
Cotrimoxazole Prophylaxis (10 min)
As you have learned from this session, people living with HIV are prone to develop OIs, such as Pneumocystis Jiroveci pneumonia (PCP), toxoplasmosis, and lower respiratory tract bacterial infections and bacterial skin infections. Cotrimoxazole prophylaxis (CPT) can potentially prevent the following OIs:
- Streptococcus pneumoniae pneumonia
- Non-typhoid salmonellosis
- Pneumocystis Jirovecii pneumonia (PCP)
- Cerebral toxoplasmosis
- Nocardiosis
- Isosporiasis
Who Should Receive Cotrimoxazole Prophylaxis?
CPT should be initiated to the following:
- All clients with WHO clinical stages 2, 3 and 4 disease.
- All clients with CD4 counts of less than 350.
- Pregnant women with CD4 counts of less than 350.
- All children born to HIV-positive mothers at six weeks of age, until they are tested and confirmed to be negative.
How Should Cotrimoxazole Prophylaxis Be Prescribed?
Cotrimoxazole should be given once daily orally. Health care workers should keep the following recommendations in mind when offering CPT:
- CPT should be started at least two weeks before the start of ART. This allows time to identify those who might be allergic to cotrimoxazole.
- CPT should be continued indefinitely.
- For clients who are allergic to cotrimoxazole, consider desensitization.
Note: Pregnant and lactating women can be started on ART before CPT.
CPT in Infants and CShildren
All children born to HIV-infected mothers should receive CPT starting at 6 weeks after birth, or at first encounter thereafter with the health care system. They should continue until the HIV infection has been excluded, and the infant is no longer at risk of acquiring HIV through breast milk.
In the HIV-infected child:
- CPT should be continued indefinitely.
- Dapsone can be provided for children who cannot tolerate cotrimoxazole.
- Severe adverse reactions to cotrimoxazole in children are uncommon.
- Children must be given once daily cotrimoxazole according to their weight.
- Adherence should be discussed at initiation and monitored at each visit.
Cotrimoxazole is contraindicated for infants and children with glucose-6-phosphate/dehydrogenase deficiency, and those with a history of severe adverse reaction to cotrimoxazole or other sulphur drugs.
The following reactions are uncommon and may include:
- Severe skin reaction, such as Stevens-Johnson syndrome
- Severe anaemia
- Pancytopaenia
- Renal and/or hepatic insufficiency
- Severe haematological toxicity
Dosing of Cotrimoxazole for Infants, Children and Adults
Age Dose Suspension (240 mg/5ml) Adult tablets (480 mg) Paediatric tablets (120 mg) 0 to 6 months 2.5 ml ¼ tablet 1 tablet 6 months through 3 years 5 ml ½ tablet 2 tablet Over 3 years 10 ml 1 tablet 3 tablet Source: Guidelines for Antiretroviral Therapy for the Prevention and Treatment of HIV in Zimbabwe 2015
Criteria for Cotrimoxazole Initiation and Discontinuation in Infants and Children
Age Criteria for Initiation Criteria for Discontinuation HIV exposed infants age group All from 6 weeks of age Until cessation of breastfeeding
Until cessation of breastfeeding
‹1 year In all Should be continued indefinitely 1-5 years WHO clinical stages 2, 3, and 4 regardless of CD4% OR
Any WHO stage and CD4 ‹25% or in all
Should be continued indefinitely ≥ 5 years including adults Any WHO stage and CD4 count ‹ 350 cells/mm3 OR
WHO stage 3 or 4 regardless of CD4 level
Should be continued indefinitely Source: Zimbabwe ART Guidelines 2016
When to Discontinue Cotrimoxazole (Zimbabwe OI/ART Guidelines)
In settings with low prevalence of both malaria and bacterial infections, CTX may be discontinued for children 5 years and older who are clinically stable or virally suppressed on ART for at least 6 months and with a CD4 count more than 350 cell count. For adults, pregnant and breast-feeding women, discontinue when clinically stable on ART, with evidence of immune recovery and viral suppression.
In malaria endemic settings or areas with high prevalence of severe bacterial infections, once CTX has been initiated, it must be continued. Do not stop.
Isoniazid and Cotrimoxazole Prophylaxis and ART Guidelines in Relation to WHO Clinical Stage and CD4 Count
National Policy Guidelines WHO Clinical Stage 1 (Asymptomatic) WHO Clinical Stage 2 (Mild) WHO Clinical Stage 3 (Advanced) WHO Clinical Stage 4 (Severe) INH Prophylaxis After excluding active TB After excluding active TB After excluding active TB After excluding active TB Cotrimoxazole Prophylaxis If CD4 count is ‹ or = 350 Cotrimoxazole prophylaxis Cotrimoxazole prophylaxis Other prophylaxis on treatment plan Cotrimoxazole prophylaxis Other prophylaxis on treatment plan ART therapy Only if CD4‹500 Only if CD4‹500 Medically eligible Medically eligible Evaluate the client for ART If HIV infected, prepare the client for ART initiation and adherence. Pregnant and breastfeeding women and children require rapid adherence preparation. -
Knowledge Check (15 min)
Take a look at the following photos and identify which stage the person is and why.
-
Key Points (5 min)
- Nausea and vomiting in PLHIV may be caused by medication or OIs.
- HCWs should be able to competently counsel clients on ART who may experience nausea and vomiting.
- Diarrhoeal disease is common in PLHIV and it is important for HCWs to diagnose and manage it appropriately.
- The diagnosis of PCP in children, adolescents, and adults is essentially a clinical one.
- CMZ prophylaxis will prevent PCP as well as a number of bacterial infections.
- Always exclude TB and PCP in children, adolescents or adults presenting with signs and symptoms of pneumonia.
- Nausea and vomiting in PLHIV may be caused by medication or OIs.
- HCWs should be able to competently counsel clients on ART who may experience nausea and vomiting.
- Diarrhoeal disease is common in PLHIV and it is important for HCWs to diagnose and manage it appropriately.
- Cryptococcal meningitis is the most common cause of mortality in PLHIV.
- It is important that a HCW is confident is making the diagnosis of CM and commences treatment or refers the client urgently.
- Fluconazole prophylaxis should be given to all PLHIV who have been diagnosed with CM, until they have reached a state of immune reconstitution.
- Oral and skin lesions occur frequently in PLHIV.
- Oral lesions should be managed appropriately, as they may cause PLHIV to reduce their food intake and have difficulty taking ARVs.
- HCWs should be able to differentiate between the different skin lesions and prescribe appropriate management.
- PLHIV have an increased risk of developing malignancies, such as Kaposi Sarcoma and Lymphomas.
- Malignancies in HIV-infected individuals are usually an indication of severe immunosuppression, and hence, eligibility for ART.
- Cotrimoxazole prophylaxis should be started in adults in WHO stage 2, 3 and 4, and in all clients with CD4 below 350, and continued until the client achieves immune reconstitution.
- All children born to HIV-infected mothers should receive CPT starting at 6 weeks after birth, or at first encounter thereafter with the health care system and should continue until they are confirmed HIV uninfected after cessation of breastfeeding.
- All clients initiating ART should be actively screened for evidence of OIs, especially in those with a CD4 count of below 100.