Session 9: Tuberculosis and HIV Co-Management
Introduction, Screening, and Diagnosis
This session will focus on tuberculosis (TB). You will be introduced to the global landscape of this epidemic, including specific details about how it is impacting Zimbabwe. Next, you will be given an overview of the disease including how it’s contracted and transmitted; the different strains of the disease; the progression it has within the body; and risk factors for developing active TB. The session will then look at screening for TB and will outline algorithms you can use for evaluating clients.
Learning Objectives
By the end of this session, you will be able to:
- Describe the epidemiology of TB and TB/HIV globally and in Zimbabwe.
- Describe the basic facts about TB.
- Describe the risk factors for acquiring TB.
- Describe the basic principles of the End TB Strategy.
- Identify signs and symptoms of TB.
- Identify presumptive TB cases using the TB screening tool.
- Describe the bacteriological and clinical diagnosis of TB.
Learning Activities
-
Understanding TB (10 min)
Tuberculosis (TB) is the world’s most deadly infectious disease, which kills more people than even HIV. Zimbabwe is one of the 30 high-burden countries that contribute to more than 80% of the global burden of TB, TB-HIV, and multi-drug resistant TB (MDR-TB). In this session, we will discuss TB care and management at the primary health care level in Zimbabwe.
Global Epidemiology of TB
In 2015, an estimated 10.4 million people suffered from TB globally. Men accounted for 5.9 million (56%), women made up 3.5 million (34%), and children accounted for 1.0 million (10%). People living with HIV accounted for 1.2 million (11%) of all new TB cases. There were an estimated 1.4 million TB deaths in 2015, and an additional 0.4 million deaths among PLHIV. Although the global incidence continues to fall by 1.5% annually, this needs to accelerate to a 4 – 5% annual decline by 2020. Even though it is curable, only 83% of all TB clients in 2014 and 52% of MDR-TB clients in 2013 were successfully treated.
TB in Zimbabwe has been fueled by a high HIV prevalence. It 2015, it was estimated that about 14.6% adults, ages 15-64 years, were infected with TB. For every ten of these clients diagnosed and started on TB treatment, seven of them were co-infected with HIV. In 2015, 72% of the total estimated TB cases in the community were diagnosed and started on treatment.
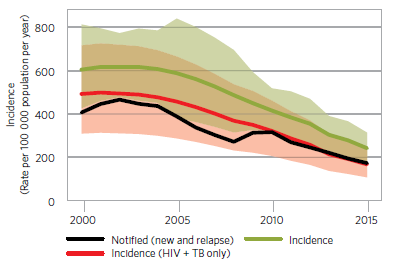
As you can see in the chart below, improved access to ART has significantly contributed to a reduction in the morbidity and mortality from TB in Zimbabwe. TB incidence in 2015 was 242 per 100,000 population compared to an estimate of 605 per 100,000 in 2000. Mortality due to TB alone has declined from 18 per 100,000 population in 2000 to 11 per 100,000 population in 2015.
What is TB?
TB is an airborne infectious and notifiable disease caused by a bacterium called Mycobacterium tuberculosis (M. tuberculosis). It can infect any system or organ within the human body. TB is carried in airborne particles, called droplet nuclei, and transmitted from person to person through the air when a person with active pulmonary TB coughs, sneezes, or speaks. Depending on the environment, these tiny particles can remain suspended in the air for several hours.
Transmission occurs when a person inhales droplet nuclei containing M. tuberculosis, and the droplet nuclei traverse the mouth or nasal passages, upper respiratory tract, and bronchi to reach the alveoli of the lungs.
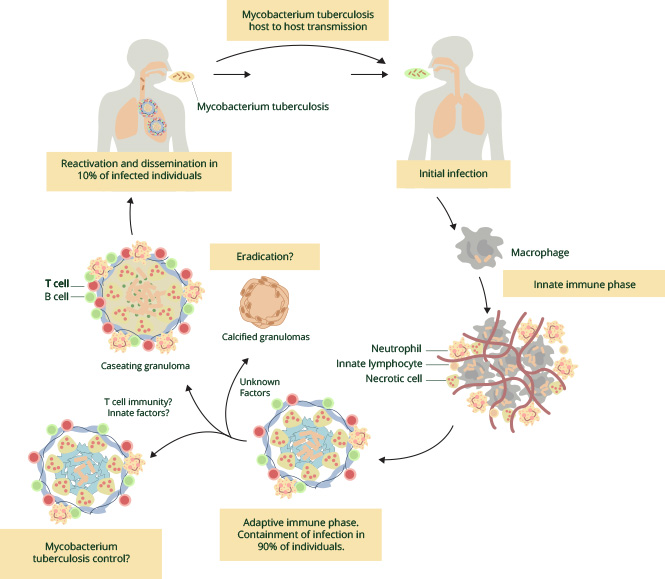
Once inhaled, the TB bacilli go to the lungs. White blood cells take up the TB bacilli, trying to initially kill it, and ultimately contain the infection. This results in the formation of Ghon focus (inflammatory primary lesion) in the lung tissue, also called the Primary Complex. Most people are able to contain the infection at this stage and never develop active TB disease. However, in some people, reactivations and dissemination of the infection can occur resulting in clients presenting with signs and symptoms of TB. This mostly occurs in people with a weak immune system that cannot contain the bacilli. The image below shows the pathogenesis of TB.
The probability that a person who is exposed to M. tuberculosis will become infected depends primarily on:
- The concentration of infectious droplets
- The number of bacilli generated by the TB client
- The amount of UV light and ventilation in the area--bacteria can more easily survive in areas with poor amounts of these
- Duration of exposure—there is a higher risk when more time is spent with an infectious person such as living in the same household
- Level of immunity
Once infected, a person can go for several years before showing any signs and symptoms of active TB disease. Such persons are said to have latent TB infection.
-
Factors Affecting Risk (5 min)
The infectiousness of a person with TB disease is directly related to the number of bacilli they expel into the air. In addition, there are various factors that determine the probability of transmission and acquisition of infection. These include factors of both the host and the recipient, many of which are poorly understood; factors related to the pathogen; and environmental factors. Tap on each factor below to view what is currently known about transmission of M. tuberculosis.
Infectiousness of the air droplets
As mentioned in opening paragraph of this section, the infectiousness of a person with TB disease is directly related to the number of bacilli they expel into the air. Clients with bacteriologically confirmed TB are more infectious than those with clinically diagnosed TB, but both can transmit it.
Susceptibility of the exposed individual
The immune status of the exposed individual is closely associated with their risk of becoming infected with TB. People with a weak immune system, like those with HIV, diabetes, or malnutrition, are at a greater risk.
Environment
The environment where transmission is taking place can be a factor for infection. When we talk about the environment, we are talking about the surroundings that an individual lives in. In these surroundings the concentration of infectious droplet nuclei, space, ventilation, air circulation, lighting, air pressure, and specimen handling all come into play and impact the probability of becoming infected. People in congregate settings like prisons and overcrowded places like urban slums where there is also poor ventilation are at increased risk.
Exposure
Duration, proximity, and frequency of exposure to an infectious individual are all important factors. TB contacts, such as family and people living in the same household as with someone with TB, and healthcare workers (HCWs) are at increased risk because of the increased amount of exposure that they are likely to have.
Persons most at risk of progression from TB infection to TB disease
The majority of people without HIV infection who are infected with M. tuberculosis do not develop tuberculosis disease. About one-third of HIV clients are co-infected with latent TB; of these clients, 5-10% per year will develop active TB disease. This percentage is grossly higher than the 5-10% lifetime risk of developing active TB disease in HIV-negative individuals. Because HIV is so closely linked with TB, TB clients should routinely be offered testing and counselling for HIV.
The Zimbabwe National TB Control Programme (NTP) has identified the following groups of people as high-risk groups for active TB:
- Persons living with HIV Infection (PLHIV).
- Extremes of age: Children, especially those less than 5 years and elderly above 65 years.
- Current and ex-miners (both formal and informal).
- Persons living in correctional facilities, including inmates and officers working in these facilities, as well as their families.
- Healthcare workers.
- Persons living with diabetes mellitus.
- Persons receiving immunosuppressive therapies.
- Persons living in remote rural areas with poor access to health services.
- Persons living in other congregate settings such as refugee camps and compounds.
- Friends, family, and coworkers of those living with TB (TB contacts.)
-
Types of TB (5 min)
Latent TB vs. Active TB
Not all infected people with TB infection develop active TB disease. TB disease can develop soon after infection, many years after infection, or maybe never. A person infected with M. tuberculosis without signs and symptoms of TB has latent tuberculosis infection (LTBI), or latent TB. The table below illustrates the differences between the two:
Latent TB infection Active TB disease Person carries TB bacilli inside body Organ disease Immune system is able to control the infection Immune system is unable to control the infection No active multiplication of TB bacilli TB bacilli multiply actively No signs and symptoms Symptomatic Not infectious Infectious Types of TB
There are two forms of TB, pulmonary TB and extrapulmonary TB (EPTB). Pulmonary TB affects the lungs, while EPTB affects other organs.
Common sites for EPTB include the following:
- Cervical lymph nodes (scrofula)
- Heart (TB pericarditis)
- Spine (Potts disease)
- Pleura
- Brain (TB meningitis)
- Kidney (renal TB)
Another key difference between pulmonary TB and EPTB is that pulmonary TB is infectious, while EPTB is usually not.
Clients who are bacteriologically confirmed (smear, Xpert, culture positive) pulmonary TB are the most infectious cases in the community. Therefore, it is very important to treat them in order to effectively control the spread of disease. Some clients with pulmonary TB are clinically diagnosed (smear, Xpert, culture negative) and are much less likely to infect others. Clinical diagnosis of TB requires other methods such as X-ray, and an expert clinician.
Early detection of positive pulmonary TB cases is very important and should be a priority for every health worker.
-
End TB Strategy (10 min)
Tuberculosis prevention, care, and control are based on the following nine guiding principles:
- Early and complete identification of incident TB cases with prompt initiation of effective treatment so as to reduce TB morbidity, including clinical illness that may result from long-term sequel of TB, prevent death, and stop transmission of the causative agent.
- Treatment of active TB disease with multiple medicines to prevent M. tuberculosis from developing resistance to any one single medicine.
- 3Provision of appropriate support to persons being evaluated for TB or on treatment for TB to ensure full adherence to treatment. This support should help avoid processes or procedures that have the potential to increase diagnostic or treatment costs to the client or their family.
- Provision of an enabling environment with adequate resources (human, financial, commodities, work environments) to ensure effective and efficient delivery of TB services.
- Proactively and routinely screening and testing for groups of clients known to be at risk of active TB for the disease and promptly linking those found to have TB to care and treatment.
- Provision of tuberculosis preventive therapy (TBPT) to individuals who are infected with M. tuberculosis, but who at the time of evaluation do not have clinical, radiologic, and/or bacteriologic evidence of active TB disease.
- Engagement with multiple partners and stakeholders in the TB response including private health care providers, non-governmental organizations, community-based organizations, and communities themselves in the TB response.
- Vigorous pursuit of efforts to eliminate poverty in the population that is the major driver of TB.
- Provision of an environment for creativity and innovation to thrive with rapid adaptation of new ideas, approaches, and practices.
In 2014, the World Health assembly passed a comprehensive strategy for tuberculosis prevention, care, and control that encompasses the principles listed above. This strategy presents targets and milestones for globally eradicating TB. Fittingly, it’s called the END TB Strategy.
The main targets for 2035 are to:
- Reduce tuberculosis deaths by 95% (compared with 2015).
- Reduce new cases of tuberculosis by 90%.
- Ensure that no family is burdened with catastrophic expenses due to TB.
The pillars and components of the strategy are three-fold. Tap on each pillar to read more:
Pillar One
Integrated, patient-centred care and prevention
- Early diagnosis of tuberculosis including universal drug-susceptibility testing, and systematic screening of contacts and high-risk groups.
- Treatment of all people with tuberculosis including drug-resistant tuberculosis, and patient support.
- Collaborative tuberculosis/HIV activities, and management of co-morbidities.
- Preventive treatment of persons at high risk, and vaccination against tuberculosis.
Pillar Two
Bold policies and supportive systems
- Political commitment with adequate resources for tuberculosis care and prevention.
- Engagement of communities, civil society organizations, and public and private care providers.
- Universal health coverage policy and regulatory frameworks for case notification, vital registration, quality and rational use of medicines, and infection control
- Social protection, poverty alleviation and actions on other determinants of tuberculosis
Pillar Three
Intensified research and innovation
- Discovery, development and rapid uptake of new tools, interventions and strategies
- Research to optimize implementation and impact, and promote innovations
For more details about the END TB Strategy, see the END TB Strategy FAQ Sheet available in the resources section of the training.
-
Knowledge Check (10 min)
-
Screening for TB (5 min)
Joseph is recently diagnosed with HIV. He comes to your clinic complaining of a cough that he has had for four weeks. Upon further investigation, he has a fever, but reports a lack of appetite. He also says that he lost some weight after having diarrhoea that resolved after two weeks. His current BMI is 19 kg/m2.
Joseph exhibited some of the key symptoms that are suggestive of TB—he had a cough, decreased appetite, and weight loss. The following is the complete list of signs and symptoms to screen for when working with a client who may have TB:
- Cough of 1 week or more; any duration (for PLHIV)
- Production of sputum
- Night sweats
- Fever
- Weight loss
- Shortness of breath
- Chest pain
- Loss of appetite
- A general feeling of being unwell
-
Bacteriological and Clinical (10 min)
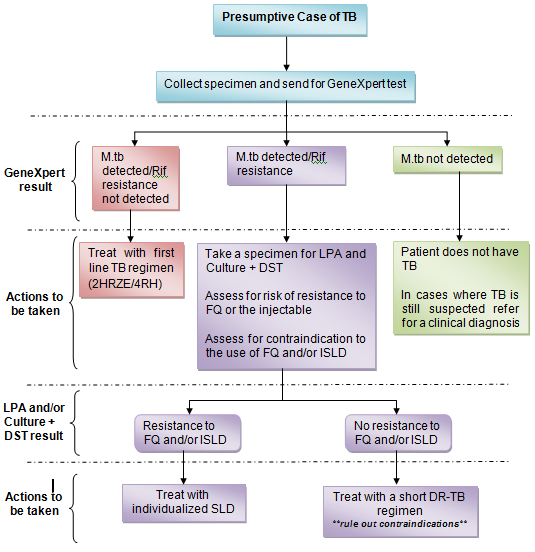
As mentioned in the previous section, the TB algorithm recommends conducting a GeneXpert TB test on clients who have a positive symptom screen, and/or a low BMI (≤ 17 kg/m2), and/or an abnormal chest x-ray.
Algorithm for diagnosis of bacteriologically confirmed TB
Once the GeneXpert (Xpert MTB/Rif Assay) test is completed, use the following algorithm to determine the next course of action:
Diagnosis of extrapulmonary TB
Even if clients do not exhibit respiratory symptoms such as a cough, if they have a fever, night sweats, and/or weight loss, you will want to evaluate them for tuberculosis as these symptoms could be indicative of extrapulmonary TB (EPTB).
You may find it quite difficult to diagnose EPTB as the symptoms will vary depending on the organ being affected. However, many clients with EPTB will experience constitutional symptoms of fever, night sweating, and loss of weight. The presence of these symptoms, especially if they have lasted several weeks, should alert you of the possibility of EPTB. Delays in diagnosing EPTB, particularly among PLHIV, can result in poor treatment outcomes. If you are in a lower level primary health institution, refer all clients you presume to have EPTB to a district or mission hospital where a medical officer can make the diagnosis and start them on treatment.
Tap on the following forms of EPTB to read more about their clinical presentation and the recommended investigations to conduct for each:
TB adenitis
Typical clinical presentation: Asymmetrical, painless non-tender lymph node enlargement usually for > 1month, +/- discharging sinus, especially in the neck.
Investigations: Fine needle aspiration (FNA) for GeneXpert and cytological examination. Node biopsy can also be sent for Gene Xpert, TB culture and histological examination.
Pleural TB
Typical clinical presentation: Chest pain, shortness of breath, reduced breath sounds and stony dullness on percussion and reduced breath sounds.
Investigations: CXR to confirm pleural effusion, thoracocentesis (pleural fluid aspiration) and pleural fluid analysis (biochemistry and cell analysis), pleural biopsy for Gene Xpert, TB culture and histological examination.
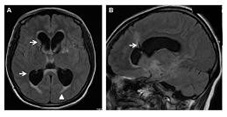
TB meningitis
Typical clinical presentation: Headache, irritability/ abnormal behaviour, vomiting (without diarrhoea), lethargic/reduced level of consciousness, convulsions, neck stiffness, bulging fontanelle in young children, cranial nerve palsies.
Investigations: Lumbar puncture obtain CSF for Xpert MTB/Rif/ assay, microscopy, culture, and sensitivity for other causes of meningitis.
Miliary TB/ disseminated TB
Typical clinical presentation: Non-specific, lethargic, persistent fever, wasting.
Investigations: Chest radiography and lumbar puncture to obtain CSF for GeneXpert /blood for TB culture, liver, and/or splenic aspirates and other tests.
Abdominal TB/ peritoneal TB
Typical clinical presentation: Abdominal swelling with ascites or abdominal masses.
Investigations: Abdominal ultrasound and ascitic tap for Xpert MTB/RIF assay/ ultrasound guided abdominal mass or organ sampling for cytological and bacteriologic testing including GeneXpert.
Osteo-articular including spinal TB
Typical clinical presentation: Swelling of the end of long bones with limitation of movement/anterior collapse of vertebra on x-ray, para-spinal abscesses, cold psoas abscess /unilateral effusion of usually knee or hip joint.
Investigations: Radiography of joint or bone or spine, if there is a joint effusion tap or synovial biopsy for GeneXpert.
Pericardial TB
Cardiac failure, distant heart sounds. Apex beat difficult to localise, large and globular heart on the CXR.
Investigations: Echocardiography/Ultrasound and pericardial tap, send pericardial fluid for GeneXpert.
Clinial diagnosis of TB
Not all clients with active TB are able to produce sputum that will have M. tuberculosis detected using a GeneXpert or other confirmatory lab tests. Most PLHIV, for example, have a low bacillary load in their sputum and will therefore have negative GeneXpert results despite having TB.
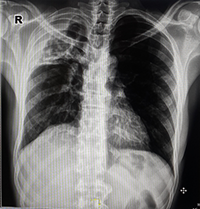
If you have a client who has a chronic cough and other constitutional symptoms of TB and who doesn’t respond to the appropriate antibiotic treatments, he or she may have TB even if the GeneXpert tests come back negative. In these situations, refer the client to a medical officer at the district or mission hospital where a clinical diagnosis of TB can be made. The medical officer will use a combination of clinical signs and symptoms, other supporting evidence from a CXR and laboratory tests (LF-LAM, pleural fluid aspirates, csf, ascitic fluid tap), and his or her clinical expertise to make the diagnosis of clinical TB. By referring a client early to a medical officer, you can help facilitate an early diagnosis and better treatment outcomes. This is a typical CXR for pulmonary TB.
-
Knowledge Check (5 min)
-
Key Points (5 min)
- TB is the world’s most deadly infectious disease that kills more people than even HIV.
- In 2015, people living with HIV accounted for 1.2 million (11%) of all new TB cases worldwide.
- TB is an airborne infectious and notifiable disease caused by a bacterium called Mycobacterium tuberculosis. It is carried in airborne particles, called droplet nuclei and transmitted from person to person through the air when a person with active pulmonary TB either coughs, sneezes, or speaks.
- There are two forms of TB, pulmonary TB and extrapulmonary TB (EPTB). Pulmonary TB affects the lungs and is infectious, and EPTB affects other organs and is not infectious.
- Not all infected people with TB infection develop active TB disease. A person infected with M. tuberculosis without signs and symptoms of TB has latent tuberculosis infection (LTBI), or latent TB.
- Because HIV is so closely linked with TB, TB clients should routinely be offered testing and counselling for HIV.
- The World Health Organization has created a comprehensive strategy for the TB prevention, care, and control called the End TB Strategy.
- All clients presenting at a health facility should be screened for active TB.
- Symptom screening is based on a history of cough, fever, weight loss and night sweats.
- Where available a CXR should be used to screen for TB among presumptive cases.
- Where available a CXR should be used to screen for TB among presumptive cases.
- A spot sputum should be collected in all presumptive TB clients and sent for GeneXpert.