Session 10: ART Initiation
Starting Adults on ART
In this session, we will discuss the benefits of Antiretroviral therapy, how to assess client readiness for ART in various populations, the appropriate ART regimen and dosage, and effective adherence support interventions and strategies for supporting adherence to ART.
Learning Objectives
By the end of this session, you will be able to:
- Explain how to assess client readiness for ART.
- Describe the preferred first line ART regimen in Zimbabwe.
- Describe the important side effects of ARVs.
Learning Activities
-
Introduction to Initiating ART (5 min)

Meet Nancy. She is a 29-year-old woman who started treatment for PTB 2 months ago (coughing, lost weight, and sputum was +AAFBs). The nurse told her she needed to start ART because she has TB. She tested HIV-positive last year and diagnosed PTB.
She is a teacher by profession but not able to work due to the illness. Her husband and 2 children have not been tested. She has not had CD4 count yet; currently on TB tx. On examination she weighed 58 kg and seems well.
Throughout this session, you will learn how to assess client readiness for ART in various populations, understand the appropriate ART regimen and dosage, and complete case studies to demonstrate your understanding.

Prior to starting ART, health care workers should:
- Have a documented HIV test result.
- Verify HIV test result.
- Be sure client fits the criteria to be started on ART at a first-level facility.
- Make sure all opportunistic infections have been treated or stabilized.
- The client is ready for ARV therapy.
- Supportive clinical team prepared for chronic care.
- Have a reliable drug supply.
When initiating ART, it is important to educate patients about the benefits of ART, address barriers to adherence, and recommend strategies to optimize adherence. On a case-by-case basis, ART may be deferred because of clinical and/or psychosocial factors; however, therapy should be initiated as soon as possible.
Remember, starting ART is generally not an emergency, so patients should be adequately prepared for it.
To assess clients for readiness to ART:
- Review the ARV regimen, dosage, and scheduling.
- Discuss the likely potential adverse effects.
- Determine required monitoring.
- Address medical and psychosocial issues (e.g., alcohol, psychiatric disorders).
- Counsel clients about adopting appropriate lifestyle measures, such as safer sex practices (including use of condoms).
-
Treatment Decisions for Initiating ART (5 min)
ART is recommended for all individuals with HIV, regardless of CD4 cell count or WHO clinical stage, to reduce the morbidity and mortality associated with HIV infection and to prevent HIV transmission.
As a priority, you should initiate ART in all individuals with severe/advanced HIV disease (WHO clinical stage 3 or 4), or CD4 count less than or equal to 350 cells/mm3.
Clients with CD4<100
Clients with CD4 cell count below 100 should be fast-tracked for treatment initiation. Clients should:
- Be screened for symptomatic TB.
- Be screened for Cryptococcal disease using serum Crag test.
- Receive cotrimoxazole and INH prophylaxis like all other clients.
- Be closely monitored for 3 months, as this is their highest risk period for contracting bacterial infections and TB or cryptococcal immune reconstitution inflammatory syndrome (IRIS).
As a health care worker, you should educate clients and their families to report immediately to a health facility if they are unwell whilst their CD4 is <100.
Reasons to Defer ART
The decision to initiate ART should always include consideration of a patient’s comorbid conditions and his or her willingness and readiness to initiate therapy. Thus, on a case-by-case basis, ART may be deferred because of clinical and/or psychosocial factors; however, therapy should be initiated as soon as possible.
Reasons for deferring ART for a client include:
- Has cryptococcal meningitis (defer for at least 2 to 4 weeks)
- Needs further counselling (e.g., for alcohol problems)
- Has TB (defer starting ART for at least 2 weeks)
- Has no fixed abode
- Has untreated mental health issues (e.g., severe depression, schizophrenia)
- Is terminally ill and unable to swallow oral medications
Such clients should be offered continued monitoring and close follow-up as well as counselling so that ART can be started at an appropriate time. Very ill clients should be referred to the next level for doctor’s assessment and discretion.
-
Recommended Treatment Regimens for Adults and Adolescents (5 min)
Huge reductions have been seen in rates of death and suffering when use is made of a potent ARV regimen, particularly in early stages of the disease. The national ART programme is now using simplified and user friendly fixed-dose combinations (FDC) for ARVs. The following information is taken from the Consolidated National Guidelines for Antiretroviral Therapy for the Prevention and Treatment of HIV in Zimbabwe 2016.
First-Line ART Regimens for Adults and Adolescents
First-line ART should consist of two nucleoside reverse-transcriptase inhibitors (NRTIs) plus a non-nucleoside reverse-transcriptase inhibitor (NNRTI).
For initiation and maintenance, a triple combination of tenofovir (300 mg) + lamivudine (300 mg) + efavirenz (600 mg/400 mg) is recommended as the preferred option to initiate ART and will be taken once a day.
If TDF + 3TC + EFV is contraindicated or not available, one of the following options is recommended:
- TDF + 3TC + NVP
- AZT + 3TC + EFV/NVP
- TDF + FTC + EFV/NVP
Target ARV Regimen Alternative Regimen Adolescents (10-19 years) ≥ 25 kg, Adults including pregnant and breastfeeding women, TB/HIV, HBV/HIV TDF + 3TC + EFV TDF + 3TC + NVP
AZT + 3TC + EFV
AZT + 3TC + NVPSource Guidelines for Antiretroviral Therapy for the Prevention and Treatment of HIV in Zimbabwe, 2016 guidelines, page 28.Clinical Considerations when using TDF
Tenofovir (TDF) may be associated with acute kidney injury or chronic kidney disease as well as reduced bone mineral density in pregnant women, adolescents and children. Below are clinical considerations when using TDF:
- Laboratory monitoring is not mandatory to initiate treatment with TDF.
- Routine blood pressure monitoring may be used to assess for hypertension.
- Urine dipsticks may be used to detect glycosuria or severe TDF nephrotoxicity in individuals without diabetes using TDF-containing regimens.
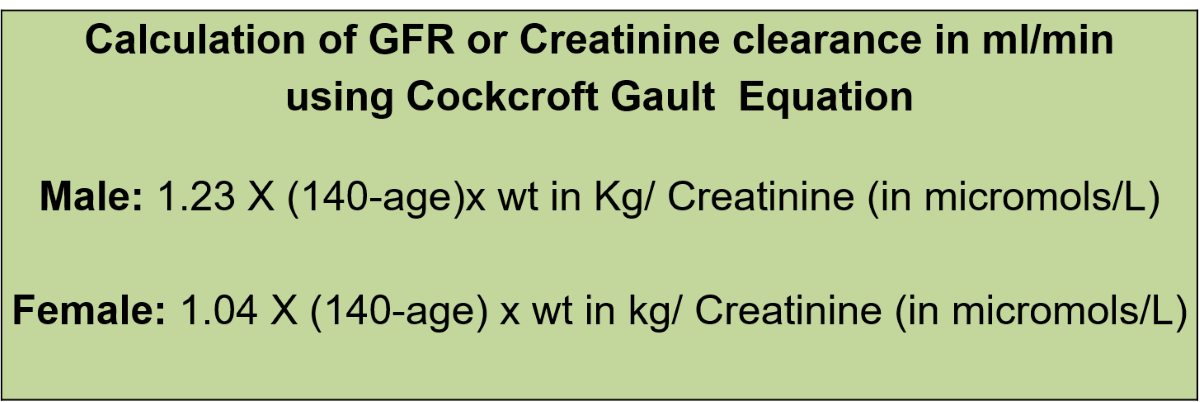
- If the creatinine test is routinely available, use the estimated glomerular filtration rate at baseline before initiating TDF regimens.
- Do not initiate TDF when the estimated glomerular filtration rate is below 50 mL/min, or in clients with uncontrolled diabetes, uncontrolled hypertension and renal failure.
-
Adverse Medical Events (5 min)
Some patients experience treatment-limiting toxicities associated with ART. In these cases, ART must be modified. ART-associated adverse events can range from acute and potentially life-threatening to chronic and insidious.
Serious life-threatening events require the immediate discontinuation of all ARV drugs and re-initiation of an alternative regimen without overlapping toxicity. Toxicities that are not life-threatening can usually be managed by substituting another ARV agent for the presumed causative agent without interrupting ART. Other, chronic, non–life-threatening adverse events can be addressed either by switching the potentially causative agent for another agent or by managing the adverse event with additional pharmacological or nonpharmacological interventions. Management strategies must be individualized for each patient.
The fundamental principle of regimen switching is to maintain viral suppression. A change of a single medicine in a multi-medicine regimen is permitted—that is, the offending medicine may be replaced, preferably with an alternative medicine of the same class.
If the client has suspected adverse medicine events, therapy should be altered as follows:
- An alternative to lamivudine (3TC) is emtricitabine (FTC); these medicines are considered pharmacologically equivalent. In the event that you come across a client on tenofovir/emtricitabine/efavirenz, you may substitute emtricitabine with lamivudine.
- Given zidovudine adverse events, such as anaemia or neutropenia, zidovudine will be replaced by tenofovir.
- If a client reacts to nevirapine, he or she should be switched to efavirenz 400 mg or 600 mg orally once daily at night.
- In the event of lactic acidosis, the current ARVs should be discontinued, and ART restarted after checking for normalisation of the lactate levels.
- In case of severe psychiatric reaction on EFV give NVP provided there are no contraindications to NVP.
- In case creatinine clearance is known and <50 mL/min give AZT or abacavir.
- For clients presenting with renal impairment; consult/refer for specialist opinion.
Reference
See Appendix III of the Guidelines for Antiretroviral Therapy for the Prevention and Treatment of HIV in Zimbabwe) for substitutions in the event of medicine toxicity/adverse events and unavailability.Later in this session, you will learn more about the toxicities that can occur with ART medications and how to effectively monitor your clients.
Tips from the Experts on the Safety and Efficacy of ARVs
- Regimens based on two NRTIs plus one NNRTI are efficacious, are less expensive, have generic formulations, and are available as FDCs.
- The preferred first line regimen of tenofovir, lamivudine and efavirenz has relatively few adverse effects and is taken once daily.
- PIs should generally be preserved for second line or third line therapy and for infants.
- Zidovudine (as an alternative to tenofovir) can cause anaemia but is less likely to cause peripheral neuropathy.
- Efavirenz has less adverse effects compared to nevirapine.
- Nevirapine can cause a rash and hepatotoxicity, and thus should be used with caution when initiating ART at higher levels of CD4 counts (e.g., in women with CD4 counts greater than 250, and in men with CD4 counts greater than 400).
- Stavudine has been phased out.
-
Side Effects of ARVs (5 min)
All ARVs have class-specific side effects and individual medicines may cause specific side effects. In addition, significant medicine interactions and toxicities may occur when using some ARVs in combination with each other, and with other medicines, such as TB medicines.
Take a look at the table below to view the important side effects of ARVs and action to be taken.
Medicine Side Effects Action to be Taken Nucleotide/Nucleoside reverse transcriptase inhibitors Tenofovir (TDF) - Gastrointestinal (GI) symptoms
- Rash
- Renal complications
- Decreases in bone mineral density
Monitor creatinine.
Substitute with zidovudine or abacavir.Zidovudine (AZT, ZDV) - Anaemia
- Neutropenia
- Headache
- Myopathy
- Lactic acidosis
- Lipoatrophy or lipodystrophy/fat redistribution
Monitor full blood count; if severe anaemia, change to tenofovir or abacavir. Lamivudine (3TC) Usually nil Abacavir (ABC) Severe hypersensitivity Reactions Withdraw medicine immediately; give alternative, such as tenofovir or zidovudine.
Do not restart medicine, as this can be fatal.Stavudine (d4T) - Peripheral neuropathy
- Abdominal pain
- Fatigue
- Lactic acidosis
- Pancreatitis
- Lipodystrophy/fat redistribution
Monitor and withdraw medicine if symptoms are severe or unacceptable to client. Non-nucleoside reverse transcriptase inhibitors Nevirapine (NVP) - Fever
- Fatigue
- Nausea
- Mild or severe skin rashes (e.g., Stevens- Johnson syndrome [rare])
- Liver toxicity
- Abnormal liver function tests (LFTs)
If LFTs are suggestive of hepatitis or if jaundice is present, discontinue.
If rash is severe, discontinue and replace with Efavirenz.Efavirenz (EFV) Central nervous system symptoms (usually during the first three weeks and then resolve): - Confusion
- Headache
- Sleep disturbance
- Abnormal dreams
Monitor; withdraw medicine if symptoms persist. Gynaecomastia Substitute with NVP Protease Inhibitors Atazanavir (ATV) - Jaundice
- Nausea
- Diarrhea
- Headache
- Hyperbilirubinaemia
Monitor; withdraw medicine if symptoms are severe. Lopinavir/ritonavir (LPV/r) - Lipodystrophy/fat redistribution
- GI intolerance
- Diarrhoea
- Hyperglycaemia
- Hyperlipidaemia
Give loperamide for the diarrhoea. Monitor: withdraw medicine if symptoms are severe. Ritonavir (RTV) - Lipodystrophy/fat redistribution
- Pancreatitis
- Hepatitis
- Skin sensitivity
- Circumoral paraesthesia
- Nausea
- Vomiting
- Diarrhoea
Monitor; withdraw medicine if symptoms are severe. Integrase Inhibitor Raltegravir - Mood changes
- Depression
- Myopathy
- Skin reactions e.g., Stevens- Johnson syndrome, hypersensitivity
- Hepatotoxicity and hypersensitivity reactions
Discontinue if severe skin reaction occurs. Dolutegravir (DTG) Monitor, withdraw medicine if symptoms are severe Source Guidelines for Antiretroviral Therapy for the Prevention and Treatment of HIV in Zimbabwe, 2016, Table 14, pages 53-54. -
Knowledge Check (5 min)
-
Key Points (5 min)
- Prior to initiating ART, HCWs should assess clients for readiness.
- The preferred first line regimen of tenofovir, lamivudine and efavirenz has relatively few adverse effects, and is taken once daily.
- All ARVs have class-specific side effects, and individual medicines may cause specific side effects. All clients taking ART should be monitored for side effects. Refer to appropriate guidelines to for treatment of these side effects.