Session 11: Monitoring Clients on ART
Comorbidities
In this section you’ll be introduced to common comorbidities associated with HIV, such as hypertension and diabetes mellitus, and you learn how to manage them in your clients. You will also be introduced to common mental health issues for PLHIV and the value of providing psychosocial support for this population.
Learning Objectives
By the end of this session you will be able to:
- Describe common comorbidities that PLHIV may develop.
- Discuss treatment options for comorbidities.
- Assess mental health in PLHIV.
- Identify strategies to meet the psychosocial support needs of PLHIV.
-
Reading: Comorbidities (10 min)
Gerald

Gerald is a 55-year-old man who owns his own business. He was diagnosed with HIV in his early 30s and has been on ART since then. When he first tested positive, he felt very sad and hopeless. He had a very good childhood friend who had died from this disease only a year after being diagnosed. Gerald felt like he would have the same fate. This made it very difficult for him to concentrate on his new business or spending time with friends and family. In addition, he was very worried that his family would find out about his status. He didn’t want them to think badly of him. At the time, his doctor said that what Gerald was feeling was normal and it was called depression. He put him on special medication and connected him with a support group where he could talk to other people living with HIV. In time, Gerald began to feel better and more like himself again.
Recently, Gerald noticed that he needed to urinate all the time. His wife also complained that he was getting too thin. She didn’t want the neighbors to think she didn’t feed him well. After a series of tests, his doctor told him that he had developed diabetes and that he would need to take additional medication and to change his diet. If he did this, his doctor said that Gerald would continue to live for many more years.
Comorbidities
The development of highly active antiretroviral therapy for HIV infection in the 1990s is one of modern medicine’s most dramatic success stories. Once, being diagnosed with HIV was a death sentence, and stories of clients like Gerald who have lived for 20 years with HIV would not have been possible.
Now, with ART, HIV infection is largely a manageable chronic condition. Today, Gerald and many others on an ART regimen can reasonably expect to live longer. This remarkable success has brought with it a new set of challenges for clients and health professionals.
Even when the disease is well controlled, people with HIV can develop aging-related conditions, such as cardiovascular disease, certain cancers, kidney and liver disease, osteoporosis, and cognitive impairment decades ahead of their HIV-negative counterparts.
Elderly clients who are HIV-positive are also susceptible to developing chronic and metabolic complications and adverse effects associated with their treatments. As the number of PLHIV who are reaching older ages increases, their health needs become a more pressing public health issue.
Management of HIV and AIDS is gradually expanding to include chronic and metabolic complications of the disease and the adverse effects associated with its treatment. It is therefore important that screening and management of common comorbidities are offered as part of comprehensive HIV treatment and care.
-
Reading: Physical Diseases (10 min)
As mentioned in the case study above, Gerald was recently diagnosed with diabetes mellitus. This disease along with hypertension are two physical diseases that PLHIV are at risk of developing. Tap on each of these diseases to learn more:
Hypertension
PLHIV are at risk of developing hypertension. Hypertension is defined as a diastolic blood pressure of 90mm Hg or higher, or a systolic pressure of 140mm Hg or higher. Furthermore, hypertension is a leading risk factor for coronary heart disease, congestive heart failure, stroke, ruptured aortic aneurysm, renal disease, and retinopathy. When you meet with PLHIV, conduct routine blood pressure measurements to screen for hypertension. Also, educate your clients about the risks for developing elevated blood pressure.
Risk factors for hypertension include:
- Increasing age
- High dietary salt intake
- Lack of exercise
- Being overweight/obesity
- Smoking
- High alcohol intake
- ART medicines, such as the PIs
Several medicines are available for the management of hypertension. Visit the resources section of this training to read guidelines for management from the Essential Medicines List and Standard Treatment Guideline for Zimbabwe (EDLIZ).
Diabetes Mellitus
As we saw with Gerald, diabetes and metabolic complaints frequently develop in PLHIV clients. Diabetes mellitus is a metabolic disorder characterized by chronic hyperglycaemia with disturbances of carbohydrate, fat, and protein metabolism resulting from defects in insulin secretion, insulin action, or both. Certain metabolic factors related to HIV, and to HIV therapy, may increase the incidence of diabetes in PLHIV. As treatment of HIV develops and access to HIV therapy improves, the incidence diabetes in PLHIV may increase.
Major symptoms of diabetes are:
- Polyuria
- Polydipsia
- Polyphagia
- Unexplained loss of weight
- Recurrent infections, such as candidiasis
Clients who have symptoms and signs suggestive of diabetes must be offered blood sugar testing. If blood sugar is elevated, management of diabetes mellitus should be offered according to national guidelines available in the EDLIZ.
-
Reading: Mental Health in PLHIV (15 min)
Like Gerald, it’s common for PLHIV to struggle with mental health issues such as depression, anxiety, and substance abuse.
Mental health is the state of well-being in which every individual realises his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.
As you know, positive mental health is important for everyone. An individual’s mental health status affects how he or she thinks, feels, and acts. It also helps determine how an individual handles stress, relates to others, takes care of him or herself, and makes choices. A good mental health status enables an individual to function better at work, at school, and in relationships. In addition, good mental health means that an individual can provide better care for his or her children or other family members.
Overall, mental health plays a significant role in an individual’s physical health. WHO emphasizes this point by defining health as, “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
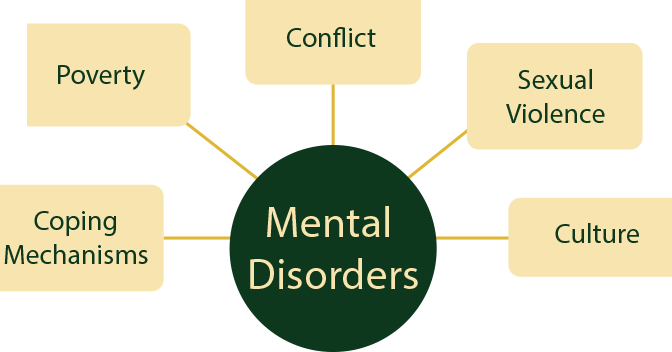
The prevalence of mental disorders varies widely by setting, and may be influenced by difficult life circumstances, such as poverty, conflict, sexual violence, culture, and coping mechanisms. Studies show an increase in the prevalence in mental health disease in PLHIV.
Substance Abuse Problems
When you work with PLHIV, it’s highly likely that you will have clients who have both mental health and substance abuse problems. Alcohol and drug abuse can negatively affect treatment adherence and also increase the risk of liver diseases. Co-infection with HBV and/or HCV increases the risk of liver damage. Since poor mental health and substance abuse both negatively impact HIV outcomes, it’s important to integrate both mental health and substance abuse services into the HIV care that clients receive. Providing integrated care becomes extra challenging in resource-limited settings that are remote or under-resourced and where many health care workers may lack training in how to diagnose and manage mental health problems.
Managing Mental Health Problems
At the most basic level, you should ask clients about mood, feelings of helplessness, and depression at each clinic or home visit. Depression can be managed by physicians or clinical officers, but it’s important to keep in mind that there is potential for interactions between many drugs used in psychiatric treatment and antiretroviral drugs. Basic counselling can assist individuals, especially when suffering follows diagnosis or relates to stigma or bereavement. There are also many psychiatric treatment options that are available that can be provided by trained professionals. If mental health issues are suspected, the Shona Symptom Questionnaire (Appendix 3 OSDM) can be used by healthcare providers for screening and monitoring response to interventions. This questionnaire is available in the resources section of this training.
Clients who are diagnosed with mental health conditions will need appropriate evidence-based treatment. PLHIV suffering from mental health disorders may be treated with medicines, psychological interventions, counselling, and/or social interventions. As a healthcare worker, you should refer PLHIV for appropriate assistance, whether it’s a community-based support group with other PLHIV, counselling services, or psychiatric services. Drug therapies for mental health problems may work better if used along with special kinds of psychological therapies. Social interventions that target psychosocial risks factors associated with greater psychiatric morbidity may also lead to improvements in PLHIV with mental health disease.
-
Reading: Psychosocial Support (5 min)
One of the ways Gerald was treated for depression was with a support group. This kind of psychosocial support is one of the ways to address and prevent mental health issues. Psychosocial support is defined as an ongoing process which aims to meet the physical, emotional, social, mental and spiritual needs of clients and their families. When possible, refer PLHIV to a support group. These groups can offer a safe environment where participants can share ideas and experience as well receive ongoing support related to adherence and other issues. Sometimes support members are the only other people who know an individual’s status.
Support for Children and Adolescents
For children and adolescents, an HIV diagnosis can provide stress and anxiety for many different reasons. They may face difficulty accepting and coping with their status. They may also have fear about the uncertainty about their future or of disclosing their status to others. They may feel a desire and need for normal physical and emotional relationships. On top of these difficult emotions, they may not have loving, supportive, or accepting relationships in their lives. Connecting HIV-positive children and adolescents with psychosocial support groups helps them realize that they are not alone. It also provides a safe and confidential environment for them to openly discuss their experience and emotions.
-
Quiz: Knowledge Check (10 min)
-
Reading: Key Points (5 min)
- Screening for and the management of hypertension, diabetes mellitus, and mental health disorders in PLHIV needs to be part of comprehensive HIV management, treatment, and care.
- Poor mental health is common among PLHIV and it is important to recognise and manage appropriately.
- When possible children, adolescents, and adults should be referred to local psychosocial support services.
In conclusion, the following key points are important to keep in mind when discussing comorbidities in PLHIV:
