Session 11: Monitoring Clients on ART
Monitoring Overview
In session 11 you will learn about monitoring HIV-positive adults, children, and adolescents. In this particular section, you will learn about the value of monitoring and how to monitor for adherence to treatment, side effects, and treatment effectiveness.
Learning Objectives
By the end of this session you will be able to:
- Describe the process of monitoring adults before starting ART.
- Discuss monitoring once ART has been initiated in adults.
- Explain the procedures for monitoring children and adolescents.
- Discuss the criteria for referrals for adults, adolescents and children.
-
Reading: Introduction (5 min)
Tafadzwa
 Tafadzwa is a 38-year-old truck driver. Recently, he tested positive for HIV and was told that he would need to begin taking medications. Before starting him on an ART regimen, the healthcare worker gave him an exam, measured his blood pressure, and took bloodwork. Once on medications, he was asked to keep track of how many times he missed taking one of his pills in a notebook and bring this notebook and his medications to his next visit in two weeks. Tafadzwa was very careful and only missed taking two of his pills in between his visits. During the next visit, the healthcare worker gave him another exam and asked if he was experiencing any new symptoms. Tafadzwa said that his appetite was not what it usually was and that foods sometimes had a metallic taste, but otherwise he felt fine. Following the exam, Tafadzwa was told that he would need to return back in two weeks for another visit. He was also encouraged to let the health worker know if he experienced any additional symptoms or illnesses before this time.
Tafadzwa is a 38-year-old truck driver. Recently, he tested positive for HIV and was told that he would need to begin taking medications. Before starting him on an ART regimen, the healthcare worker gave him an exam, measured his blood pressure, and took bloodwork. Once on medications, he was asked to keep track of how many times he missed taking one of his pills in a notebook and bring this notebook and his medications to his next visit in two weeks. Tafadzwa was very careful and only missed taking two of his pills in between his visits. During the next visit, the healthcare worker gave him another exam and asked if he was experiencing any new symptoms. Tafadzwa said that his appetite was not what it usually was and that foods sometimes had a metallic taste, but otherwise he felt fine. Following the exam, Tafadzwa was told that he would need to return back in two weeks for another visit. He was also encouraged to let the health worker know if he experienced any additional symptoms or illnesses before this time.Value of Monitoring
Monitoring HIV clients, like Tafadzwa, is vital and enables us to know whether treatment is successful or not. Overall, monitoring ensures that we can improve clients’ health, keep them healthy, decrease their risk of developing resistance to medication, and decrease their risk of HIV transmission to sexual partners or from mother to child.
When we perform a test to monitor a client on ART, it’s not an end but rather the beginning of monitoring the client. We need to act on the results appropriately through correctly interpreting results and by helping the client understand what the results mean so that he or she will adhere to the treatment plan. Normal results should be communicated to patients and good adherence reinforced.
-
Reading: Before Starting ART (5 min)
Before Starting ART
Once clients begin their medications, you will need to closely monitor them to assess adherence to the treatment regimen, side effects of the medications, and the efficacy of the treatment.
However, monitoring starts even before clients begin their treatment. When you first meet with a HIV-positive client, you will want to monitor them in the following ways:
- Take a detailed history
- Perform a physical examination including blood pressure measurement
- Perform basic laboratory tests
- Conduct a confirmatory HIV test before ART initiation
- Screen for TB
- Give the client an ART card for documenting his or her treatment and visits (available from the AIDS and TB Directorate)
- Document the client’s WHO clinical stage in his or her file or card
In most instances, you will also want to perform the following baseline tests:
- Full blood count (if zidovudine will be used)
- Baseline CD4 cell count
- Alanine transaminase test
- Serum creatinine test (if tenofovir will be used)
- Urinalysis
- Pregnancy test
- Mantoux test in children
- GeneXpert or CXR (to exclude TB)
- Blood pressure
- Syphilis serology test (if possible)
- Hepatitis B and C tests (if possible)
-
Reading: Monitoring Adherence to Treatment (7 min)
Monitoring Adherence to Treatment
In order for treatment to be effective, clients need to adhere closely to their treatment regimen--a 95% adherence is recommended. You can help with adherence by providing counselling, strengthening client’s treatment literacy skills, and conducting routine adherence assessments. Tap on each category to learn more:
Counselling
At each visit provide counselling and encourage clients to seek help between visits as needed.
Treatment literacy
Clients on ART need to understand their treatment including how their medications work and what side effects are possible. They also need to know what steps they can take to continue to live a healthy and positive life. Treatment literacy aims to educate clients about their treatment so that they can be successful on their treatment regimen. When working with your clients, you can help them with health literacy by providing them with information on side effects and what to expect from the treatment as well as answering any medication related question that they might have.
Adherence assessment
At each visit, assess adherence to determine if the client is taking medications according to the agreed upon schedule. Pill counting is a useful tool for this; therefore, instruct clients to bring all of their medications and containers to each visit. Refer back to the adherence assessment session to refresh your memory about how to do this.
Adherence Measurement Tools
To date, there is no standardized tool to measure adherence. There are, however, two approaches typically used. Either adherence is measured by gathering information from the client or it is measured by independently monitoring drug intake. Both of these approaches come with their own set of advantages and disadvantages. Tap on the tools below to learn more:
Client self-report
During a client self-report, you will ask the client to report on his or her own adherence through a series of questions. The recall time that you use can vary. For example, you can ask the client to recall the number of times that he or she missed a dose over the past four days, over one week, or over a month.
Advantages: This is a relatively simple and efficient method of assessing adherence in clinical practice. It is more reliable when asking about a shorter recall period (e.g., four days).
Disadvantages: Clients may overestimate adherence for recall periods longer than four days.
Pill counts
Using pill counts allows you to independently monitor drug intake in a way that is not dependent on a client’s report. When taking a pill count, you will count the number of pills that the client has leftover in his or her pill bottles. Use this number to calculate adherence using the following formula:
Adherence percentage = ((# doses should have been taken - # missed doses) ∕ # doses should have taken) × 100 ∕ 1
Advantages: Simple, cheap, and objective in assessing adherence.
Disadvantages: This method relies on the clients to bring all their medications during visits, but studies have noted that client’s sometimes put pills in another container, leave some at home, or share with family or friends who are also HIV positive. As a result, relying on this method may lead to an over-estimation of adherence.
Population Council et al., 2004; Wagner et al., 2001Pharmacy refill tracking
Another independent monitoring method is to gather pharmacy refill data to gauge adherence. In this method, it’s assumed that clients who collect their medications regularly are adhering to the treatment.
Population Council et al., 2004Advantages: This method has the advantage of being a simple and an objective measure of adherence.
Disadvantages: This method is based on the assumption that the amount of pills remaining shows how many pills the client took. While clients may be collecting their medications from the pharmacy, there is no guarantee that they are actually taking them. Instead, they could be sharing their medications with friends and family, or discarding the pills. Also, this method will also not provide adequate information about when medications are taken and at what dosage. In addition, in order for this method to be reliable, an effective record keeping system needs to be set up in the pharmacy. This is difficult in more resource limited parts of the region where computers, let alone power, are largely non-existent in health care facilities. Finally, this method requires that clients use the same pharmacy for all refills, which is not always the case.
Biological markers
In this approach you will monitor the level of the viral load in the bloodstream in order to gauge adherence. Since the goal of HAART is to suppress the multiplication of the HIV/AIDS virus, low levels of viral load is an indication of adherence to the regimen.
Advantages: This method is objective and a state-of-the-art way of measuring adherence.
Disadvantages: There is mounting evidence that shows that viral loads could still remain high even when the client is adhering perfectly. This could be due to a number of reasons, among them treatment failure, ART drug resistance, and poor absorption of the drug.
Wagner et al., 2001; Population Council et al., 2004 -
Reading: Monitoring for Side Effects (5 min)
Monitoring for Side Effects
While on ART, clients may develop new symptoms. For this reason, make sure to examine clients carefully during each visit as newly occurring symptoms may indicate the presence of an intercurrent illness, adverse medicine events, or immune reconstitution inflammatory syndrome. If an intercurrent illness is detected, treat it appropriately. If in doubt, refer the client to your clinical mentor or higher-level OI/ART clinic.
The 2017 OSDM offers an ART follow-up schedule that is included in the resources section of this training. According to this schedule, after the initial treatment, clients should return for follow-up visits every two weeks for the first month and then monthly for the next three months. During these visits, watch for common side effects such as:
- Anaemia
- Renal impairment
- Central nervous system side effects
- Skin rashes or Steven Johnson Syndrome
- Lipodystrophy or fat redistribution
- Liver toxicities
If an adverse medicine reaction is observed document it and report to the Medicines Control Authority (MCAZ) which is the national pharmacovigilance center. The reporting forms are available at MCAZ and are included in the resources section of this training.
-
Reading: Monitoring Effectiveness of Treatment (5 min)
One of the most important goals of monitoring is to gauge whether or not the treatment regimen is effective for the client. You can do this through regular clinical examinations, along with laboratory tests. The three ways to monitor the effectiveness of ART are to evaluate:
- Clinical improvement
- Immunologic function (CD4 count)
- HIV viral load (VL)
These methods are used for adult clients as well as children and adolescents. WHO recommends VL testing as the gold standard for monitoring response to ARV medicines as it’s more sensitive and can detect adherence problems and treatment failure much earlier than CD4 count testing. Given reduced access to VL testing in Zimbabwe; however, CD4 testing should be conducted regularly at six-month intervals.Tap each heading to read more about the three methods:
Clinical monitoring
You should monitor for clinical improvement every time you meet with a client. During the meeting, ask whether the client feels better. Check to see if he or she is gaining weight. Also see if there are symptoms and signs of the original presenting illness. If relevant, check to see if infections that were present before ARVs were started such as oral thrush, hairy leukoplakia, genital herpes, skin rash, diarrhoea, and molluscum contagiosum have improved.
Clinical Failure
Adults or adolescents: An adult or adolescent client has clinical failure when a new or recurrent clinical event indicating severe immunodeficiency (WHO stage 4 clinical condition) is present after 6 months of effective treatment
Children: A child has clinical failure when a new or recurrent clinical event indicating advanced or severe immunodeficiency (WHO stage 3 and 4 clinical conditions with exception of TB) is present after 6 months of effective treatment
Immunological monitoring
In Zimbabwe, as VL testing is being scaled up, CD4 testing will continue to be used for some time. It should be conducted every six months, especially after the first two years of commencing ART.
With successful ART, the CD4 lymphocyte count increases. The rate of increase depends on the initial CD4 count. CD4 count testing should be performed every six months, particularly after the first two years of initiation of ART. If immunological failure is suspected, which is defined as persistently declining CD4 counts, as measured on two occasions at least three to six months apart, consider switching the client to a second-line therapy after consultation with your supervisor or clinical mentor or refer him/her to a higher level facility.
It is important to conduct a thorough adherence assessment prior to switching ART. If there is substance use or mental health conditions that are affecting adherence, these must be addressed so ensure adherence to the second-line therapy.
Immunological failure
Adults or adolescents: An adult or adolescent client has immunological failure when their CD4 counts falls to the baseline (or below) or persistent CD4 levels below 100 cells/mm3
Children: A child has immunological failure when their CD4 count decreases to pre-therapy CD4 count/percentage. In addition, a child younger than 5 years with a persistent CD4 level below 200 cells/ mm3 or CD4% < 10% has immunological failure. A child older than 5 years with a persistent CD4 levels below 100 cells/mm3 when a new or recurrent clinical event indicating advanced or severe immunodeficiency (WHO stage 3 and 4 clinical conditions with exception of TB) is present after 6 months of effective treatment also has immunological failure
Virological (HIV viral load) monitoring
WHO recommends VL testing as the gold standard for monitoring response to ARV medicines; this should be done routinely once a year.
With good adherence, the VL usually decreases to undetectable levels (below limit of detection), within six months of ART. For this reason, measuring VL is useful for identifying treatment failure early. In such situations, review the client’s adherence, treatment regimen and other medications including herbs and traditional medicines and consider changing the regimen.
Virological failure
A client, regardless of age, has virological failure when their viral load is greater than 1,000 copies/mL for two consecutive measurements after three months of enhanced adherence counselling.
-
Reading: Frequency of Clinic Visits (10 min)
Let’s return to Tafadzwa. To ensure that monitoring takes place at appropriate points in his care, he will need to be seen on a regular basis. Let’s go through the schedule of clinic visits that Tafadzwa will follow for the first year of treatment.
Initially, he will need to be seen every two weeks for the first month. If he’s doing well with his treatment, he will only need to visit the clinic once during the second, third and fourth months. At this point, Tafadzwa should be able to reduce his visits to every two months. If after six months from ART initiation, Tafadzwa is still doing well with his ART regimen, his visits can be reduced even further. This schedule of care follows the Routine VL Monitoring Algorithm shown below:
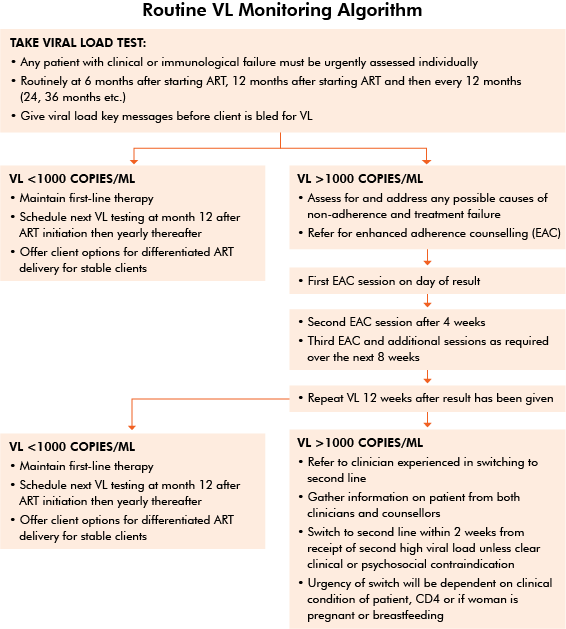
When clients like Tafadzwa are clinically stable and on chronic medication, they do not need to be seen by the clinician at every visit. For more information, refer to the OSDM in the resource section of this training.
Clinically Stable
A patient on ART is considered to be clinical stable in one of two ways depending on if VL monitoring is available.Tap on each heading to read more:
When VL monitoring is available
A client is considered stable when:
- There are no intercurrent illnesses
- The client has a VL < 1,000 copies/ml
- The client has been on ART for at least 6 months
When VL monitoring is NOT available
A client is considered stable when:
- There are no current OIs
- The client's CD4 ≥ 200 copies/mm3
- The client has been on ART for at least 6 months
-
Reading: Types of Clinic Visits (5 min)
There are three main types of clinic visits. First, there is a clinical visit. This is a scheduled appointment where the clinician makes a thorough assessment and reviews monitoring blood tests. A stable client on ART should be seen for a clinical assessment every 6 months.
The second type of visit is an unscheduled visit. This is any visit by a client who is in-between refill or clinical visits. Unscheduled visits may occur whenever a client develops a problem.
The third kind of visit is a refill visit. This is a scheduled appointment where the client has a pre-filled prescription and collects his or her medicine without seeing the nurse or doctor. According to the 2017 OSDM, there are several models available for refill visits. These different options address specific challenges and should be selected accordingly. Tap on the following to learn more:
Fast-track
Facility-based individual refill from pharmacy – target duration 30 minutes. This option should be available at all sites where drugs are dispensed from a separate room to where the clinical consultation is performed.
The client collects their refill directly from the dispensing point. They do not queue to see the clinician. The client can collect the medication any time during clinic opening hours on his or her refill day. This model has most value in sites where dispensing is performed in a separate room by a different health care worker to the clinical consultation.
Club refill
Facility-based health care worker-led group refill – target duration 30-60 minutes. Experience to date suggests that this model is more popular in sites with large cohorts and in urban areas. As a group model, it provides the additional benefit of peer support.
For clinics with larger cohorts, clients booked for refills on a given day can be organised into groups of 10-20. The group is then booked at the same time for each refill. On arrival, a health care worker (nurse, primary counsellor or expert client) facilitates discussion, identifies any group member who has a new clinical problem requiring review, and then distributes the medication. Medication can be pre-packed and labelled prior to the group meeting.
Outreach
Community-based individual ART delivery through mobile outreach. This option should be considered for clients from hard-to-reach areas or where existing outreach activities are already occurring to a fixed location. Logistics to support regular visits to the location must be ensured.
Refills may be collected by the individual client and may be distributed by the nurse or, if pre-packed, by a primary counsellor, community health worker, or expert client. If feasible differentiated ART delivery for different subpopulations and for clients with high viral loads may be delivered through outreach.
Community ART refill groups (CARGs)
Community-based client-led group refill. This refill option has been shown to be more popular in rural areas and where distance is a major challenge to the client. As a group model, there is the additional benefit of peer support. Some clients may benefit from the peer support gained by this model even where distance is not a challenge.
Community ART refill groups are self-formed groups of clients on ART. They are usually from the same geographical area and are willing to disclose their HIV status to each other. The system ensures that all members attend the clinic for their clinical visits and monitoring blood tests together as a group. For refill appointments, the group members nominate one member to collect the drugs from the facility and distribute the refill to all group members.
Family member refill
When a number of family members are on ART, it may be possible for one member to collect for the others. If a child is involved, it is essential that the child follows the paediatric follow-up schedule included in order to ensure that drug doses are adjusted correctly according to weight. Details regarding this follow-up schedule can be found on pages 46-47 in the 2017 OSDM which is located in the resources section of this training.
Additionally, for more information on the different refill visit models described above and to learn more about factors to consider when deciding the most appropriate model to recommend for a client, see section 2.5 of the 2017 OSDM.Criteria for Referrals
During a visit, there are times when you will need to refer a client to a higher level of care. The following are indications that a client on ART should be referred:
- Hb<8g/dl
- Coinfections with drug-resistant TB, cryptococcal infection
- Comorbidities, such as diabetes mellitus, kidney disease/insufficiency, liver disease/insufficiency
- Severe adverse drug events
- Treatment failure as indicated by development of new OIs or malignancies; recurrence of infections that are not responding to treatment; decline/lack of growth rate; regression of developmental milestones, etc.
- Severely ill child
- Severely malnourished child
-
Quiz: Knowledge Check (10 min)
-
Reading: Monitoring Children and Adolescents on ART (10 min)
Mary and Susan
Mary and Susan are sisters. Mary is 15 years old and Susan is 8. They lost their parents about a year ago. Their mother died of AIDS and their father, who was a heavy drinker, died of liver problems. Mary suspects that her father was also infected with HIV. Currently, the sisters are living with an aunt who has been acting as their chief caretaker. Both sisters were diagnosed HIV-positive two years ago. They have been on ART and receiving clinical care since their diagnosis.
Monitoring Children and Adolescents
Just as with adult clients, children and adolescent clients like Mary and Susan need to be closely monitored using clinical, immunological, and virologic methods to assess adherence to the treatment, tolerance of the medication, any side effects of the medications, and the efficacy of the treatment. Unlike adult clients, Mary and Susan will also be assessed using growth charts to ensure that they are growing and developing appropriately for their ages. Tap on each type of monitoring to read more:
Clinical monitoring
When Mary and Susan had their initial ART visits, the healthcare worker took care to meet with their aunt and provide her with comprehensive education regarding HIV infection, ART, follow-up appointments and expectations. The worker also reviewed with the aunt her understanding of HIV including the disease process and adherence strategies. The worker also made sure that the aunt was giving accurate dosing and administration of ART and other medications to the girls. After talking with the aunt for quite some time, the worker gave both girls a full clinical assessment.
During the two-week follow-up visit and subsequent monthly visits, the healthcare worker treating Mary and Susan completed a thorough assessment that included:
- Recording any changes in their condition since the last visit using the symptom checklist
- A targeted physical examination
- Monitoring for side effects and toxicities
- A growth and developmental assessment that checks for weight, height, head circumference (in children below the age of two years), developmental milestones, and signs of immune reconstitution
- Assessing medicaton adherence
- Asking for a demonstration of dose and administration
- Recalculating the dose based on weight if needed and dispense further medications
- Monitoring cognitive development
- Monitoring for psychosocial issues or challenges
The worker asked questions that would help with psychological monitoring. She asked the girls questions about their:
- Progress at school
- Relationships with family members, friends, and schoolmates
- Attitude towards daily medication and adherence
- Knowledge of why they are taking medications and coming to the clinic for regular visits
Because Mary is an adolescent, when the worker met with her, they discussed issues pertaining to sexual awareness and associated behavioural issues.
Laboratory monitoring
The WHO 2015 guidelines recommend virological monitoring as the method of choice for assessing treatment success or failure. Both clinical and immunological monitoring will continue to be used, and routine viral loads will be done.
The inability to perform laboratory monitoring, including CD4 or viral load, should not prevent children from receiving ART.
When children and adolescents like Mary and Susan come for their visits, the following laboratory investigations are recommended, but are not mandatory:
- Baseline Hb and WBC, if available, are recommended at initiation of ART.
- Baseline creatinine should be done if TDF is used as part of the regimen.
- Children on AZT should have Hb at 8 weeks after starting ART (or more frequently if symptomatic).
- Routine toxicity laboratory monitoring not recommended and should be based on the development of symptoms.
- Conduct a urine dipstick for protein and glucose (if available).
- Viral load is desirable, but not essential, prior to starting ART. Targeted viral load should be done to confirm clinical or immunological failure before switching a treatment regimen.
-
Reading: Role of Testing (5 min)
As you have just learned, there are many tests and measurements that are important to conduct when working with PLHIV. Clients, especially younger clients like Mary and Susan, may grow impatient and not understand why they need to keep coming in to the clinic for testing. You can explain to them and their caretakers that each test serves an important role in the monitoring process.
Through monitoring, you’re ensuring that the treatment regimen is successful and that your clients are able to thrive. The following table lists tests and measurements that are conducted when monitoring PLHIV clients and explains the purpose of each. Keep this information in mind when talking with your clients.
Test/Measurement Purpose Confirm HIV status during the initial visit Ensures that the original test was accurate Conduct a clinical assessment at each visit Identifies if there are new side effects, symptoms or opportunistic infections Measure Hb/FBC (if available) at the initial visit and then during the 1, 2, 3, 6 and 12 months Rules out anaemia due to Zidovudine Measure CD4 count (if available) at the initial visit and then every 6 months Monitors response to ART Conduct a urine dipstick for protein and glucose (if available) at the initial visit Initially excludes glycosuria and then assesses renal function Take glomerular filtration rate +/-serum creatinine (if available) at each visit Monitors renal function Conduct WHO clinical staging at each visit Monitors response to ART Test viral load at 6 months and at 12 months after ART initiation, and then annually thereafter Monitors viral suppression, response to ART, adherence assessment and detect treatment failure Ask for drug related adverse events at each visit Detect drug toxicities For children and adolescents, measure weight, height, MUAC and head circumference (for infants) at each visit Monitors growth and nutrition of child For children and adolescents, assess cognitive development at each visit Monitors overall child development -
Quiz: Knowledge Check (10 min)
-
Reading: Key Points (5 min)
- Monitoring clients on ART is necessary in order to assess adherence to treatment, tolerance, side effects, and efficacy of ART.
- Successful ART treatment can be monitored by assessing clinical improvement, immunological, and virological function.
- Virological monitoring is the “gold standard” and most sensitive way to determine ART treatment success.
- HCWs should be able to identify clients who require referring to the next level of care and promptly do so.
