Session 11: Monitoring Clients on ART
Toxicities, Side Effects, and Complications
In this section you will learn about toxicities associated with ART medications and how to manage them in your clients. You will also learn about Immune Reconstitution Inflammatory Syndrome and how to treat it.
Learning Objectives
By the end of this session you will be able to:
- Describe the principles in the management of ART medicines toxicities.
- Define and describe IRIS.
- Explain the treatment of IRIS.
-
Reading: ART Toxicities (15 min)

Up until this point we have looked at case studies where the clients are responding successfully to their ART regimen. This is not always the case. Let’s look at Rumbi. She is a 28-year-old bank teller who was diagnosed with HIV when she became pregnant with her daughter five years ago. Her initial ART regimen was nevirapine/3TC/stavudine. After a few months on her medications, she began to experience a feeling in her feet like her shoes were too tight and like there was a warm iron on the bottom of her feet. At night, the bed covers touching her feet were painful. She did not tell her provider initially because she thought the feeling was going to decrease, but also thought that it was something that she would just have to live with. When the pain started interfering with her ability to walk even short distances especially at her work and caring for her baby, she told the worker that she wanted to stop taking her medications because they made her feel bad.
After a thorough assessment of her pain and physical examination that revealed peripheral neuropathy secondary to stavudine. Her provider changed her stavudine to zidovudine and also prescribed amitriptyline at night which not only helped the pain in Rumbi’s feet but also helped her sleep better. She returned to the clinic for follow-up every few weeks but was upset that the pain continued for a long time. Several times over the first few months after changing the medication, Rumbi told her provider that she did not think she needed the HIV medications at all and that she was much better before she ever started them. She would stay in the clinic after her appointment crying and asking, “Why this is happening to me?” Rumbi’s provider asked the HTC counselor to schedule time to talk to her and provide additional support. Her provider also increased the amitriptyline dose and eventually Rumbi started to feel some relief. She was able to walk better and further and also stand on her feet longer to prepare dinner and do her housework.
After a thorough assessment of her pain and physical examination that revealed peripheral neuropathy secondary to stavudine. Her provider changed her stavudine to zidovudine and also prescribed amitriptyline at night which not only helped the pain in Rumbi’s feet but also helped her sleep better. She returned to the clinic for follow-up every few weeks but was upset that the pain continued for a long time. Several times over the first few months after changing the medication, Rumbi told her provider that she did not think she needed the HIV medications at all and that she was much better before she ever started them. She would stay in the clinic after her appointment crying and asking, “Why this is happening to me?” Rumbi’s provider asked the HTC counselor to schedule time to talk to her and provide additional support. Her provider also increased the amitriptyline dose and eventually Rumbi started to feel some relief. She was able to walk better and further and also stand on her feet longer to prepare dinner and do her housework.
Toxicities
As we learned in previous sections, monitoring clients on ART is necessary in order to assess adherence to treatment, tolerance, side effects, and the efficacy of ART. Let’s focus on monitoring for sides effects, which are also referred to as drug toxicities. According to the World Health Organization, a toxicity is an unintended effect of a drug occurring at normal doses related to the pharmacological properties of the drug.
ART toxicities can vary widely and can cause mild reactions such as rashes, insomnia, and/or diarrhoea. They can also cause more extreme reactions such as anaemia, renal failure, and Steven Johnson Syndrome. Some can even be life threatening if not managed appropriately. Moreover, toxicities can lead to poor medication adherence. For this reason, it’s important to monitor for toxicities at every clinic visit and respond promptly when they are detected. Remember to report all side effects to MCAZ.
The more common ART toxicities are:
- Anaemia (AZT-related)
- Rash, hepatotoxicity and hypersensitivity reactions (NNRTIs, especially NVP)
- Peripheral neuropathy (D4T, AZT, DDI)
- Lactic acidosis (D4T, DDI)
- Lipodystrophy/fat redistribution (D4T, PIs)
- Metabolic syndrome including insulin resistance, hyperglycaemia, hypertriglyceridaemia, hypercholesterolemia and low HDL levels (PIs)
- Jaundice (atazanavir)
- Gynecomastia (efavirenz)
-
Reading: Managing Toxicities (10 min)
You will manage toxicities differently depending on the severity of the reaction. Tap on the following severity levels to read more:
Mild reactions
While mild reactions are bothersome, they do not require changes in therapy. When a client is experiencing a mild reaction, start by evaluating him or her completely, checking to see if the symptoms are due to the ART medications or if there are other factors at work. It’s important to keep in mind that not all problems are caused by ART medications. First, look at all of the medications that the client is taking and check to see if the reaction may in fact be caused by a non-ART medication. Next, examine the overall health of the client. Often, what may seem like a reaction to ART medications may actually be caused by a concurrent infection or illness.
Side effects may be the reason why patients stop taking their medications. As we read with Rumbi, as soon as she started having trouble walking, especially at work and caring for her baby, her first thought was to stop taking the medications that were making her feel sick. She did not share her problem with her provider and waited until the symptoms became severe. When working with clients in the same situation, be sure to emphasize the importance of maintaining adherence and reassure them that many side effects are short-term and can be treated, but if they become too bothersome, that there are alternatives. Also, emphasize to all clients that they should talk to you when they first experience their symptoms and not wait until the symptoms become severe as Rumbi did. Waiting can complicate treatment and leaves a great opportunity for poor adherence.
Moderate reactions
For moderate reactions consider continuing the client on ART for as long as feasible. If the client does not improve on symptomatic therapy, consider single drug substitutions. For a few moderate toxicities such as peripheral neuropathy or lipodystrophy, you can consider single drug substitutions earlier. Always exclude treatment failure before doing a single drug substitution.
Severe reactions
Substitute the offending drug without stopping ART.
Life threatening reactions
For life threatening reactions, immediately discontinue all ART medicines. Manage the medical event with symptomatic and supportive therapy. When the client is stabilized, reintroduce ART medicines using a modified regimen (i.e., with an ART substitution for the offending drug). If the offending medicine is an NNRTI (NVP or EFV), stop the NNRTI and continue the other two medicines for a week and then stop. NNRTIs have a long half-life hence stopping all 3 medicines at once will lead to NNRTI monotherapy. If patient is being managed at a primary healthcare facility, discontinue ART, stabilize, and then refer patient to be seen by a doctor in a hospital.
Medication Substitutions
When working with PLHIV clients, there are several critical questions that you’ll want to ask yourself regarding their ART regimen. You’ll want to think about when to start them on a regimen and what medications to start them on. If there are side effects, you’ll also want to think about when substitutions are needed and what substitutions are best. Consult with HIV expert, supervisor, health officer/mentor when considering substitution, switching to second- or third-line due to treatment failure or decisions to stop ART completely. A second-line regimen should be started only after consultation with an appropriate specialist in HIV and AIDS care/treatment or your mentor.
Most critical questions to ask yourself regarding their ART regimen are:
- When to start? What to start?
- When to substitute? What to substitute?
- When to switch? What to switch?
- How to stop?
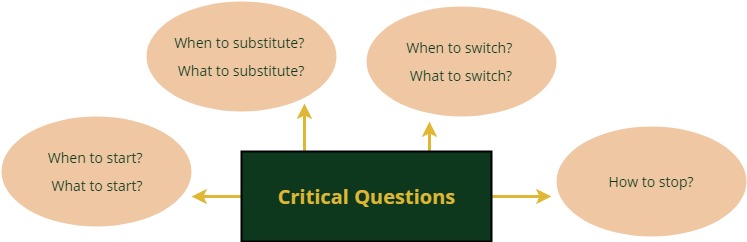
When considering a medication substitution, it’s safe to change one drug for another due to toxicity reasons, provided that the client is otherwise well and has been compliant with ARV. Switching all three drugs is reserved for treatment failure. It’s important to keep in mind that changing one drug in a failing regimen can lead to early resistance of the new drug.
The most common reasons for substitution include:
- Hypersensitivity--skin rash, hepatitis
- Hematologic--anaemia
- Mitochondrial toxicities caused by NRTIs
- Bone complications such as osteonecrosis and osteoporosis
- Severe persistent CNS toxicities e.g., dizziness (efavirenz)
- Gynecomastia (efavirenz)
- Drug induced liver injury
It is important to consult with a clinical mentor or supervisor before substituting ARVs as this may affect future treatment options.
Toxicities in Children and Adolescents
Children and adolescents may develop the same toxicities as adults, but they appear to be less common in younger children. This may be related to the immaturity of their immune systems—resulting in lower incidences of immune-mediated toxicities—and also due to the immaturity of the hepatic metabolic pathways.
-
Reading: Drug Toxicity Categories (10 min)
Rumbi, the client we learned about at the start of this section, was experiencing peripheral neuropathy. If you recall, her symptoms continued for several months and it took a while for her to feel healthy again. For these reasons, her toxicity is categorized as a chronic toxicity. In addition to chronic toxicity, there are also life threatening and acute/short-term toxicities. Tap on each type to learn more:
Acute or short-term toxicity
Acute or short-term toxicities are likely to occur in the first few months. With these toxicities it’s important to help clients with adherence and encourage them not to stop taking their medications. The following are common acute/short-term toxicities:
Gastrointestinal (GI) intolerance
GI problems are the most common side effect reported by clients taking ARVs. Fortunately, due to the newer agents, these complaints have decreased significantly. Initially after starting ART, clients may complain of nausea or a change in their stool. Counselling that includes the possibility of GI side effects and discussing ways to avoid or decrease the problem is important patient education to ensure adherence. Zimbabwe first-line ARVs can be taken with or without food but if the client is experiencing nausea, they may benefit from taking the medication with or immediately after their meal. Second-line ARVs that include a PI should be taken with food to avoid GI side effects. Clients should be encouraged to call or return to the clinic if the GI side effects increase or are preventing them from taking their ARVs.
Anaemia
The risk of developing severe anaemia is about 5% in clients. AZT and concomitant cotrimoxazole often increases this risk. Anemia is worsened by comorbidities such as malnutrition and malaria.
Prior to starting clients on AZT, test them for anaemia and make sure that either their Hb is greater than 7 g/dl or that they show no signs of clinical anaemia (if Hb testing is unavailable). If a client becomes anaemic while on AZT, stop this medication if their Hb drops to below 7 g/dl or they show signs of clinical anaemia (if Hb testing is unavailable). Tenofovir (TDF) can be used as an alternative ARV.
Central Nervous System (CNS) effects
It’s common that you will have clients who experience CNS effects early in their ART treatment with efavirenz (EFV). These effects usually subside after 1-2 weeks. About 26% to 58% of clients on EFV develop these types of toxicities. Symptoms include headaches, dizziness, vivid dreams, sleep/mood alteration, depression, and psychosis (rare). Usually a medication substitution is not needed for CNS effects, but when it is, you can use nevirapine (refer to guidelines for CD4 restrictions) or lopinavir/ritonavir.
Renal failure caused by tenofovir
It’s rare for tenofovir to cause renal toxicity in otherwise normal kidneys, but it’s common for this medication to aggravate renal impairment. Therefore, before starting a client on tenofovir, a baseline creatinine level should be taken ideally using the estimated glomerular filtration rate. Do not initiate TDF and seek expert advice when the estimated glomerular filtration rate is less than 50 mL/min or in long-term diabetes, uncontrolled hypertension, and renal failure. According to the 2016 Zimbabwe guidelines, urine dipsticks may be used to detect glycosuria or severe TDF nephrotoxicity in clients without diabetes using TDF-containing regimens. Creatinine levels should be repeated if there any indications of renal impairment.
Chronic toxicity
Most chronic toxicity are due to the mitochondrial toxicity of NRTIs. The following are the most common forms of chronic toxicity:
- Peripheral neuropathy
- Lipoatrophy
- Lactic acidosis
- Pancreatitis
- Hepatic steatosis
- Myopathy
- Nephropathy
Peripheral Neuropathy
There are three distinct forms of peripheral neuropathy (PN) associated with HIV.
The first is HIV-associated peripheral (or distal) sensory polyneuropathy. This form of PN occurs in more than 30% of clients and usually occurs when the CD4 count is less than 200. Clients with peripheral sensory polyneuropathy usually experience peripheral paraesthesia, which is typically feelings of “pins and needles”, itching, burning or cold sensations or reduced sensation beginning in the toes and moving proximally.
The second form of PN is NRTI-associated peripheral neuropathy. It’s most common when clients are on stavudine and didanosine and is much less common when patients are on zidovudine. It’s rarer for clients on lamivudine, tenofovir, and abacavir to experience NRTI-associated peripheral neuropathy.
The final form of PN is INH-induced peripheral neuropathy, which can occur in clients on TB medications. This form of PN is prevented or reversed with vitamin B6 (pyridoxine).
There are several management strategies that you can use for clients with PN. If the client has PN during the initial stages of starting ART, it may be due to the virus itself and/or prior or current alcohol use or diabetes. Once the virus is better controlled, the symptoms of PN may decrease. If the PN is due to diabetes, it will be important to ensure that the client is following his/her diabetic medication and nutrition regimen. Alcohol use should be lessened or discouraged. If, however, PN develops while the client is on ART, you can use symptomatic therapy for minor cases. Anticonvulsants such as lamotrigine and gabapentin are found to be effective in managing PN, but can be cost prohibitive. If cost is an issue, you can try more affordable medications such as amitryptilline and carbamazepine. You may also find that your clients need an analgesia such as paracetamol or co-codamol to help with pain.
It’s important to warn your clients that symptoms can take months to resolve. By letting them know what to expect, you will help to reduce the chances that they will become discouraged and stop taking their medications.
Lipodystrophy
Another chronic toxicity that clients can develop is lipodystrophy. Lipodystrophy refers to the changes in body fat that affect some people with HIV. A client may experience loss of fat tissue in their face, limbs, and/or buttocks (lipoatrophy). They may also experience an accumulation of fat in their abdomen, breasts, or neck (lipohypertrophy). Lipodystrophy is less common with the newer antiretroviral medications. The following images show what lipodystrophy looks like when it presents on the face, arm, and mid-section.
Source: https://aidsinfo.nih.gov/understanding-hiv-aids/fact-sheets/22/61/hiv-and-lipodystrophyCurrently, there is no treatment for lipodystrophy, however, progression can be halted by substituting tenofovir or abacavir (NOT zidovudine). Clients may eventually recover lost fat over time, but this is not always the case.
Metabolic Disturbances
NRTIs and PIs can all be associated with:
- Dyslipidemia, which is elevation of plasma cholesterol, triglycerides (TGs) or both, or a low high-density lipoprotein level that contributes to the development of atherosclerosis
- Diabetes mellitus
- Osteopenia which is reduced bone mass of lesser severity than osteoporosis
Atazanavir (boosted or unboosted), darunavir, and saquinavir appear to have a limited effect on insulin sensitivity and glucose metabolism.
Life threatening toxicity
Life threatening toxicities include:
- Drug hypersensitivity—Stevens-Johnson Syndrome
- Hepatitis
- Pancreatitis
- Lactic acidosis
-
Reading: Drug Hypersensitivities (10 min)
Drug hypersensitivities are a specific kind of side effect involving an immune-mediated system reaction. They are much more common with PLHIV than with HIV-negative individuals. For PLHIV, hypersensitivities usually occur early in therapy, most often during the first 4 weeks.
Early signs and symptoms include:
- Mucosal involvement
- High liver enzymes
- High fever
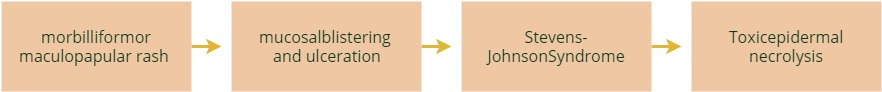
Clients with drug hypersensitivities often have dermatological (cutaneous) reactions that range from a minor skin rashes to more severe skin disorders such as Stevens-Johnson Syndrome and toxic epidermal necrolysis. The following image shows the range of reactions
Other symptoms include:
- Myalgia, arthralgia
- Fatigue
- Hypotension
- Nephritis, pneumonitis, hepatitis
The most common ARVs that result in drug hypersensitivity are both NNRTIs, nevirapine, efavirenz, abacavir, and cotrimoxazole. Tap on following headings to learn more:
NNRTI hypersensitivity
As mentioned above, nevirapine and efavirenz are most often the cause of hypersensitivity in PLHIV. The risk of developing this hypersensitivity is increased by certain factors. For example, clients who are on prednisone have an increased risk of developing NNRTI hypersensitivity. In addition, men with a CD4 of greater than 400 cells/µL and women with a CD4 greater than 250 cells/µL are at a greater risk. While age and race have not been found to be risk factors, women are more at risk than men.
For clients on nevirapine, risk is reduced by following the recommended dose escalation which is Nevirapine one tablet daily for the first two weeks. If no reaction, increase to the standard dose of one tablet twice daily. Also, if a client has a reaction to nevirapine, it does not necessarily mean that he or she will react to efavirenz as the risk of cross-hypersensitivity is low.
The following chart shows the likelihood of developing reactions on nevirapine and efavirenz:
EVF NVP Total incidence of rash (all grades/causes) 28% 35% Incidence of severe rash (grade 3-4 rash) 0.7% 6.6% Incidence of Steven Johnson's syndrome 0.1% 0.3% Treatment discontinuation due to rash 1.7% 7.0% Clients with NNRTI hypersensitivity will need close monitoring and supportive therapies such as antipruritics, antipyretics, and antibiotics in secondary skin infection. It’s not recommended to use steroids for clients with Steven Johnson’s syndrome. This is because specialists have found steroids to be harmful in advanced forms of the syndrome and unhelpful in early stages. When symptoms are resolved, restart the treatment with an alternative drug--either efavirenz or lopinavir/ritonavir. It is recommended that clients who develop hypersensitivity reactions be discussed with supervisor or clinical mentor.
Abacavir hypersensitivity reaction
Abacavir hypersensitivity is genetically rare in Africans. When it does occur, it usually begins within 4-6 weeks of starting therapy with a median onset is 11 days. Symptoms usually resolve quickly with cessation of therapy. If a client has had a previous hypersensitivity reaction, do not reuse abacavir as this can lead to more serious reactions, occurring within hours, such as hypotension and even death. Document abacavir hypersensitivity clearly in the clinic record so all providers are aware of this reaction.
Even though abacavir is not used as frequently and a hypersensitivity reaction to this medication is rare in Africans, it’s important to keep abacavir hypersensitivity in mind as it can be fatal.
Hepatitis
Nevirapine and sometimes efavirenz can cause hepatotoxicity. It usually occurs during the first 6 months and may be worsened by:
- Alcoholism
- Viral infections: hepatitis viruses (HBV, HCV)
- Heart disease (congestive heart failure)
- Concomitant medications (including TB medications, herbal therapy)
If a client’s liver enzymes (AST/ALT) levels increase to over 5 times the upper limit of normal or if clinical hepatitis (anorexia, nausea with jaundice) occurs, stop nevirapine immediately. When issues are resolved, restart with an alternative drug—either efavirenz or lopinavir/ritonavir.
Pancreatitis
If a client is experiencing abdominal pain, anorexia, nausea, vomiting, it may be due to pancreatitis. Didanosine and some TB medications can cause this reaction. The risk for developing pancreatitis may be worsened when the client:
- Abuses alcohol
- Has CD4 greater than 200 (risk doubled)
- Is a female (risk doubled)
- Has had pancreatitis previously (risk doubled)
- Is taking cotrimoxazole
Consult with your supervisor or mentor about treatment for pancreatitis, stopping ARVs until the condition is resolved and which ARVs to resume when the client is stable. Hospitalization may be needed for stabilization and treatment of serious pancreatitis
Lactic acidosis
Lactic acidosis is a rare but potentially fatal condition usually occurs in clients between 6 and 24 months of starting ART and peaks around 12 months. Typical history includes:
- Worsening peripheral neuropathy (often rapid)
- Weight loss (often dramatic)
- Loss appetite, nausea, abdominal pain
- Vomiting, myalgias
- Acidosis (dehydration, kussmal’s respiration)
For clients lactic acidosis, start by measuring serum lactate (if possible). Next, stop all medications and do not resume medications for at least one month or longer and only when all symptoms have resolved. Give clients intravenous fluids for supportive therapy. When restarting ART, avoid AZT, ddI and d4T. Patients must be managed in hospital and when discharged they must be followed up closely.
In patients who develop lactic acidosis it is important to stop ARVs for a period of time. NVP and 3TC are safe to restart, but the third drug should be tenofovir or abacavir. Lactic acidosis should be considered in any client with unexplained weight loss or vomiting or if there is a sudden worsening of peripheral neuropathy.
-
Reading: Immune Reconstitution Inflammatory Syndrome (10 min)
Immune reconstitution inflammatory syndrome (IRIS) occurs when the improving immune function unmasks a previous undiagnosed or new opportunistic infection (OI). In this situation, there was an infection present in the client’s body, but it was not clinically evident or treated adequately before ARVs were initiated. If a client begins to deteriorate clinically after starting ART, suspect IRIS. In most cases, the following symptoms will occur within 2 to 12 weeks of commencing ART:
- Fever
- Sweats
- Cough
- Loss of weight
- Neurocognitive changes such as severe headache, confusion
- Skin rash and lymphadenopathy
In Zimbabwe, common IRIS are TB, cryptococcal meningitis, and recurrent herpes simplex virus. It’s important not to confuse IRIS with treatment failure or drug toxicity. Additionally, IRIS is not a reason to stop ART, or to change the drug regimen, but the emerging OI must be treated.
IRIS in Children
Little has been reported about IRIS in children and adolescents, though research into this area is ongoing. When diagnosing children with IRIS, it’s important to consider their medication history and to conduct a clinical assessment. Also, consider the time between the onset of ART and the occurrence of signs and symptoms as a way to differentiate between IRIS and the development of new OIs.
In Zimbabwe, the most common pathogens causing IRIS in children and adolescents are similar to those in the adult population:
- Cryptococcus
- TB
- Herpes zoster
- Kaposi’s sarcoma
- Non-Hodgkins lymphoma
-
Quiz: Knowledge Check (10 min)
-
Reading: Key Points (5 min)
In conclusion, the following key points are important to keep in mind when dealing with ART toxicities as well as IRIS:
- It is important to counsel clients and caregivers about the possible side effects of ARVs. HCWs should monitor for side effects and toxicities of ART at each clinic visit.
- Clients who are starting ART should be counselled about the possibility of developing an IRIS.
- The common forms of IRIS in Zimbabwe are TB and cryptococcal meningitis.



