Session 12: ART in Pregnant and Breastfeeding Women
Antenatal Care, Labour, and Delivery
In this section we will learn about the components of a routine ANC visit. We will then discuss how to manage labour and delivery with an HIV-positive client, talk about how to manage the client post-partum, and we will learn about the diagnosis and treatment of HIV in infants.
Learning Objectives
By the end of this section, you will be able to:
- Describe the components of a routine ANC visit.
- Explain how to manage labour and delivery in the context of HIV infection.
- Describe post-partum management of HIV-infected women.
- Explain the diagnosis and treatment of HIV in infants.
Learning Activities
-
Antenatal Care Checklist (5 min)
Ideally all pregnant women should have four routine antenatal visits, and the first antenatal visit should be as soon as she realises she is pregnant. HIV-infected pregnant women require more frequent visits for adherence and side effect monitoring and scheduled laboratory monitoring including Hb check-up.
A checklist for routine ANC visit is provided below:
- Check for risk factors.
- Assess the pregnancy status. Develop a delivery plan. During the first visit prepare a birth and emergency plan with the woman. All HIVinfected pregnant women should be advised to give birth in a facility where there are skilled attendants who can provide safer delivery practices and PMTCT services. Women should be advised to go to the health facility as soon as labour starts or their waters break, whichever comes first.
- Check for preeclampsia at every antenatal visit.
- Check for anaemia at every antenatal visit.
- Assess maternal nutrition status by monitoring the weight and MUAC at every visit and manage appropriately.
- Check for STIs and treat.
- Assess the HIV status and provide the necessary chronic care for the woman and her family integrated with antenatal care.
- Respond to observed signs or volunteered problems, such as:
- Absence of foetal movement
- Ruptured membranes and no labour
- Fever or pain on urination
- Vaginal discharge or bleeding
- Signs suggesting HIV infection
- Cough or difficulty in breathing
- Ask if she is taking antiTB medicine, ART, cotrimoxazole, or any other medicines, if so, whether she is experiencing side effects.
- Promptly and correctly treat for malaria, since susceptibility to malaria increases during pregnancy in HIVinfected women.
- Screen for TB at each visit and treat if positive. Suspect TB if the woman has had a cough for any duration, persistent fever, unexplained weight loss, night sweats, or enlarged lymph nodes. It is important to note that a woman with untreated TB may transmit TB to her unborn baby during pregnancy and after delivery.
- Give appropriate preventive measures: cotrimoxazole, IPT, and IPpT.
- Advise on the next follow-up visit
- Test all pregnant women at booking and re-test previously HIV-negative women during third trimester, and/or at delivery, six weeks post-delivery and every six months thereafter until cessation of breastfeeding.
-
Managing Labour and Delivery (10 min)
In the absence of any intervention to reduce the risks of MTCT of HIV, a significant number of infants born to HIV-infected women become infected during labour and childbirth. Those of you who are managing labour and childbirth, therefore, have an important opportunity and responsibility to prevent mother-to-child transmission of HIV.
There are standard precautions to ensure safe delivery.
- Do not routinely artificially rupture membranes.
- Undertake an episiotomy only if absolutely necessary.
- Avoid unnecessary vaginal examinations.
- Use of sterile equipment is mandatory.
- Ensure that a skilled health care provider conducts the delivery.
- Continuously monitor foetal and maternal condition using the partograph.
- Use standard precautions for infection prevention and control.
Supportive care throughout labour is very important for your client’s well-being and for contributing to a good outcome of labour. Supportive care means providing a supportive, encouraging, and reassuring atmosphere that may help to accelerate the progress of labour.
HIV Testing Scenarios of Women Presenting in Labour
Start by checking the client’s record to see if she has been tested for HIV and if the test result is recorded on her card. Or ask the woman if she has been tested for HIV, when was she tested, the result of the test, and if partner was tested and the result of the partner.
Tap each of the tabs below to learn more about the three testing scenarios of client in labour.
She tells you she has tested HIV-positive
If she has tested HIV-positive, ask if she is on ART. If she is on ART, which medicines is she taking? When did she start taking them?
If she is not on treatment, inform her that you will commence her on ART for life immediately, and the baby will be commenced on NVP and AZT for twelve weeks. (High risk infant)
She tells you she has tested HIV-negative
If she has tested HIV-negative, check when the test was done and discuss risks of HIV exposure since the last HIV test. Offer HIV testing and counselling if the last HIV test was negative before 32 weeks gestation. If a woman’s test was negative after 32 weeks or in the third trimester, she will be retested at 6 weeks post-delivery.
She tells you she has not been tested
If she has not been tested, offer HIV testing and counselling.
ART regimen
The ART regimen used in the antenatal period does not change in labour. An HIV-positive pregnant woman presenting in labour will fall into one of the two categories shown in the table below.
Woman’s antenatal ART regimen Woman’s ART regimen during labour ART
Already on ART that was started during antenatal care or before pregnancy
Continue ART No ARV intervention
Had NOT received ART during pregnancy
Start lifelong ART for the woman during labour Women who were on ART during pregnancy, should continue their regimen post-delivery. HIV-positive women who were not on ART during their pregnancy will continue the ART regimen they started during labour (TDF + 3TC + EFV) and will continue lifelong treatment once a day nocte.
ARV prophylaxis for the infant
We covered prophylaxis earlier in this session. Let’s just complete a couple of review questions before moving on:
-
Postpartum Management (10 min)
Postpartum is the period up to six weeks after birth.
Before you discharge women/couples from the maternity ward, make sure that you provide them with family planning counselling or ensure that they receive the appropriate information during their postpartum follow-up visits. You should give them information regarding the risks and benefits of each type of family planning method so they can make an informed choice and plan any future pregnancies. If the woman has not disclosed her status, you should provide counselling on the importance of disclosure. If further information on safe infant feeding practices is required, it should be given and, where possible, the male partner should be involved in the counselling and information sessions.
Both men and women should be aware that sexual relations may be resumed as soon as it is comfortable for the woman and she is ready. Encourage couples to use condoms when having sex.
Let them know that the early weeks of breastfeeding are times when women are at particular risk of becoming infected with HIV. Postpartum women are more susceptible to HIV due to biological reasons. Also let them know that the risk of MTCT is higher when a newly HIV-infected woman breastfeeds, due to a high viral load in new infections.
After discharge from the facility, you should encourage your post-delivery client to return with her infant for routine post-delivery follow-up visits at three days, seven days, and six weeks. If the client gave birth at home, you should encourage her to go to the health facility as soon as possible after delivery.
You should offer HIV testing and counselling to women who do not know their status or those who tested negative. Test all pregnant women at booking and re-test previously HIV-negative women during third trimester, and/or at delivery, six weeks post-delivery and every six months thereafter until cessation of breastfeeding.
It is important to refer all babies born to HIV-infected women for HIV testing (DNA PCR/EID) at birth (within 72hours) and six weeks of age. Where resources are constrained prioritise high risk HEI for birth testing.
Integrating HIV Care into Outpatient Post-delivery Services
HIV care and family planning services should be integrated into routine post-delivery care within maternal, neonatal and child health (MNCH) settings. This has many advantages. Integration makes it possible for most post-delivery women to receive comprehensive routine maternal and HIV care on the same visit and at the same point of care. This can contribute to preventing delays in receiving essential care, shortening waiting times at each follow-up visit, and providing better coordinated care. A woman’s own health (and her own treatment) is an important consideration to ensure the baby’s health. Most HIV-related care and treatment for HIV-infected post-delivery women will be the same as for any non-pregnant HIV-infected adults.
Post-partum Recommendations
Tap on each of the following scenarios to find out the steps involved in care and treatment.
Mother is found to be HIV-positive after the delivery at the hospital
All post-delivery HIV-infected women are universally eligible for ART and should be initiated on ART. The clinical staging and prophylaxis against OIs are the same for post-delivery HIV-infected women as for other HIV-infected adults. Recommend ARV prophylaxis for the high risk new born (NVP+AZT)
Mother is HIV-positive, not on ART, and newborn is brought to facility after home delivery within 72 hours
Recommend ARV prophylaxis for the high risk new born and counsel the woman on exclusive breastfeeding and ART adherence. Quickly prepare her for ART initiation and commence her on ART. It’s important to assess her clinical stage and, where available, get a CD4 count. However, accessing a CD4 count should not delay ART initiation in all HIV-positive lactating women.
Prophylaxis against OIs are the same for post-delivery and breastfeeding women as for all other HIV-positive adults.
If baby is delivered at home and the mother is known to be HIV positive, administer ARV prophylaxis to newborn, even if the mother did not receive ARVs during pregnancy or labour. Start the baby on NVP +/- AZT depending on risk status of baby even if mother presents 72 hours or later after giving birth. If the mother’s HIV status is unknown, offer HTC. If she consents to be tested and her test is positive, assess and provide appropriate care.
There is a lot for you to remember around HIV in the labour and delivery setting. You will need to use all your skills to make sure that the interventions for reduction of MTCT of HIV during labour and childbirth are used to their fullest degree.
-
Diagnosis of HIV in Infants and Children (10 min)
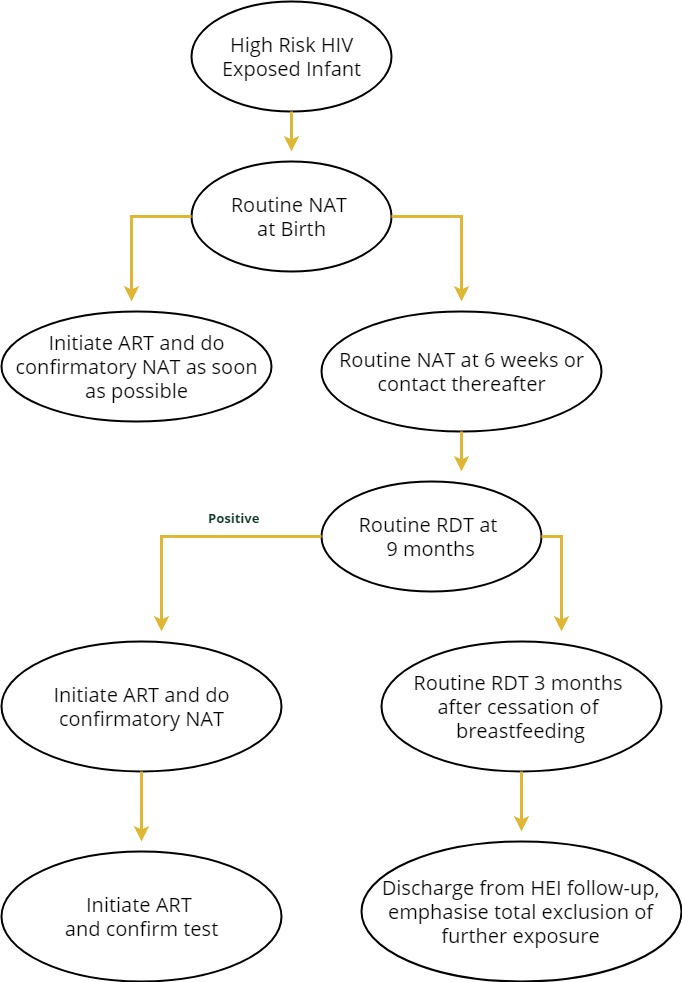
The Zimbabwe 2016 National Consolidated Guidelines recommend conduction of a nucleic acid test (NAT) to be done at birth (within 48 hours) for the high risk HEI. The NAT can be done through the usual DBS sample collection which is sent to the laboratory or as a point of care (POC) test at the facility or a nearby facility which will be acting as a hub using new technology such as the AlereQ POC NAT which are already in the country. The POC NAT can yield Infant`s HIV DNA results in just over an hour. Decentralisation of Early Infant diagnosis from only three laboratories namely NMRL, Mutare Provincial and Mpilo has already been started. This means that the turnaround time (TAT) for results even for samples that will be sent as DBS for testing will be less and results available timely. Infants testing positive with a NAT should be commenced on appropriate ART regimen for their age as soon as possible. A confirmatory nucleic acid test is mandatory but should not delay ART initiation. NAT at birth or Birth PCR will be rolled out to all HIV exposed infants as resources are availed.
Infants who test negative at birth and those in the low risk category will undergo a routine NAT at 6 weeks or earliest point of contact thereafter. Infants who test positive need to be initiated onto the appropriate ART regimen promptly while the mandatory confirmatory NAT test should be done it should not delay ART initiation.
Infants with negative results from tests done at birth and/or 6 weeks should get a routine RDT test at nine months. If the test is reactive, a NAT should be done. ART should be initiated as soon as possible after confirming HIV infection using NAT.
A final routine RDT test should be done three months after cessation of breastfeeding. If the child is above 18 months then the adult HIV testing algorithm should be followed if the test is positive. However, if the child is less than 18 months the positive RDT should be confirmed using NAT. ART should be initiated as soon as possible.
The algorithm for high-risk HIV exposed infants is below.
Active PITC for Infants and Children
Refer to accelerated action plan to scale up peadiatric ART ascertainment of HIV exposure status. For all infants with an unknown or uncertain HIV exposure at health facilities, ascertain their HIV exposure. For children below four months, use RDTs (mothers infected in their third trimester are unlikely to transfer maternal antibodies to the baby, and women who acquire HIV post-delivery do not transfer maternal antibodies through breast milk). For children 4 – 18 months, ascertain HIV exposure by testing the mother. For HEI testing at nine months, use RDTs and confirm positives with PCR.
Presumptive HIV diagnosis
Presumptive HIV diagnosis can be made where NAT testing is unavailable for infants less than 18 months, but an HIV test should be conducted as soon as possible. The criteria for making a presumptive diagnosis are a positive HIV antibody test and either
- Diagnosis of a stage 4 or any AIDS-indicator condition
OR
- Symptomatic for two of the following conditions:
- Oral thrush
- Severe pneumonia
- Severe sepsis
Case reporting form
As we move towards elimination of Mother to child Transmission of HIV and syphilis, it is important to identify all infants who test HIV positive to establish what went wrong and understand possible determinants of the HIV-positive outcome. This understanding will assist in crafting interventions to reach the goal where new infections are below 50 per 100 000 live births and the mother-to-child-transmission rate is below 5% (for breastfeeding nations like Zimbabwe). The case reporting form should be completed for all infants and children with positive results.
-
Martha’s Labour and Delivery (15 min)
Martha presents to the labour ward with her husband. She delivered her first baby, who is now two, at home, but came today since she’s not feeling well and worried about the baby. Her husband tells you that he does not like that his wife came. He doesn’t trust the clinic. All of his health problems have always been taken care of by the village traditional healer, and his son was delivered by the midwife without any problems. He felt his wife should have stayed at home with the midwife.
Martha tells you that she has had contractions since early morning that are getting stronger. It’s now late afternoon.
You admit Martha to the labour ward. Your assessment reveals the following:
Vital signs
B/P: 90/68
Pulse: 82 and regular
RR: 18 increasing during contractions
Temperature: 37.8 C
Weight: 50 kg
Height: 150 cm
Foetal heart rate: 148 beats per minute
Physical exam
Skin: dry, turgor decreased
HEENT: enlarged anterior cervical lymph nodes bilaterally
Mouth: dry, moderate amount of white plaques on the undersurface of the tongue and buccal mucosa
Chest: clear to auscultation
Abdomen: no horizontal ridge
One term size foetus palpated, movement during examination
Contractions: five minutes apart lasting one minute
Cervix: 5 cm dilated, thin, membranes intact
Urine: dark yellow, concentrated. No protein
Past medical history
- Fracture of her arm three years ago as a result of a fall.
- Medical history includes malaria when she was younger; no history of STIs or TB.
- Reports to you that she has had a white coating on her tongue and mouth that the traditional healer gave her a special drink which helped but it comes back.
- No previous HIV test done.
You ask Martha when she last had something to drink and she tells you that she had some water before coming but hasn’t been thirsty.
She also tells you that the white coat on her tongue comes and goes. She has taken a special tea in the past that seems to work for a short time, but then it comes back even worse. You ask her husband to bring her water and encourage Martha to drink. You begin your pre-test counseling.
Martha’s husband interrupts and wants to know why you need to do an HIV test when they’re both clean. He becomes agitated, especially when she’s having a contraction. He says that you just need to help her deliver his baby. His wife doesn’t need any tests or anything else in the clinic. Martha tells him that she wants the test done and asks him to please “let the nurse do her job.”
Martha’s HIV test is positive. She’s unusually quiet when the results are given, showing no emotion. You ask her if she understands the result and she nods yes. Martha asks her husband to take a test but he refuses. He says he will get it after the baby is born. He tells his wife he needs fresh air and walks out of the room.
Martha gave birth to a healthy 2.8 kg boy. She and her husband were concerned about the oral medicine they saw you give the baby and the shot he got in his leg.
While Martha recovers from labour, you provide routine post-partum care. You encourage her husband to get tested for HIV before they leave.
We will return to Martha later in the session when we cover Infant Feeding.
-
Key Points (5 min)
- Zimbabwe recommends breastfeeding as the infant feeding method of choice for all mothers regardless of HIV status.
- HIV-exposed infants need regular follow-up.
- Maternal and child health cards should be updated during each and every clinic encounter.
