Session 13: Support Services
In this session, we will discuss the importance of community support services for people living with HIV and how to organize and facilitate support groups.
Learning Objectives
By the end of this session you will be able to:
- Explain the benefit of psychosocial support.
- List the benefits of organizing support groups.
- Be able to plan and facilitate support groups.
-
Reading: Step Four (5 min)
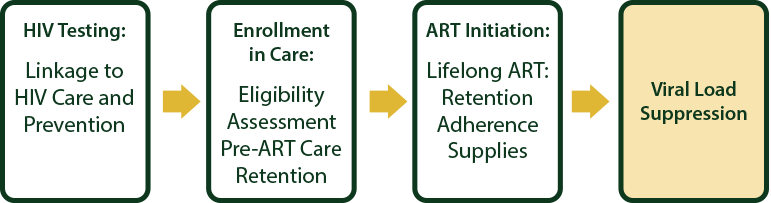
As you have learned in the previous sessions, this training follows the roadmap that is based on the WHO “treatment cascade.” It is a simple public health approach to counseling, diagnosis, and treatment. In the previous sessions, you have learned that HIV testing is an entry point for access to prevention treatment care and support services and enrolment into care and ART initiation. The fourth and final step is to ensure that appropriate long-term monitoring strategies are put in place—that patients are retained in care and that there is long-term control of HIV infection as evidenced by viral load suppression.
In this first session for the final step, we’ll cover support services.
-
Reading: Introduction (5 min)

Shingi is a 14-year-old girl who was is brought to the OI clinic by her aunt who has been her caregiver since her mother died when she was 12. She is in high school and has been doing well until the end of last term, when her teachers told her aunt that she has been uncooperative and difficult. They also told her aunt that her grades are dropping.
Her father died when she was 4 years old and she does not remember much about him. She was very close to her mother who looked after her when she was sick. Her mother and her both tested positive for HIV and TB. She was disclosed to when she was 12. Her mother was started on ARVs, but developed meningitis and died after three months of taking ARVs. Shingi has not yet started taking ARVs.
As a health care worker, you should be able to assess the different needs of individuals like Shingi and their caregivers at any given time or point of contact to ensure that their needs are addressed. However, many health facilities do not have the ability to provide all the needs and services to individuals, couples, and families infected and affected by HIV. Therefore, it is important that health care workers develop a way to establish a referral network of their clients to the community where CBOs and NGOs operate offering a variety of services that complement what is offered by the health facility.
You can do this by:
- Assessing and identifying gaps in services both at your site and in the referral network.
- Creating an integrated referral network.
- Meeting with staff at possible referral CBOs and NGOs operating in your health facility’s catchment area.
- Facilitating the coordination of service providers.
- Analysing how accessible and acceptable these resources and services are to clients.
Then create protocols and procedures for processing referrals. This includes when to make a referral, how to follow up on a referral, and how to problem-solve obstacles such as transportation, confidentiality, and childcare. You will also want to create and regularly maintain a referral resource directory that includes the name of the CBO/NGO, location and directions to the organization, physical address, and phone.
Next, we will discuss the issues of palliative care, bereavement, and psychosocial support.
-
Reading: Palliative Care (5 min)
Palliative care is an approach that improves the quality of life of client and their families facing the problems associated with a life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, including physical, psychosocial, and spiritual. It is a philosophy of care which includes a wide range of interventions in the area of clinical, emotional, social, and spiritual care.
The following models can be adapted to suit the setting in which palliative care is to be implemented:
- Home based care
- Outpatient care
- Outreach services for example roadside clinic
- Health facility based palliative care teams
- Palliative care specialised unit
- Day care
- Hospice inpatient care
- Workplace programmes
Palliative care is applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life, such as chemotherapy, radiation therapy for cancer clients, and antiretroviral therapy for people living with HIV; it includes those investigations needed to better understand and manage distressing clinical complications.
Remember that relief of pain is a fundamental human right. Palliative care provides relief from pain and offers a support system that enables clients to access and adhere to optimal clinical care. It addresses social and legal problems and in particular aims to reduce the impact of poverty on clients and their family members. This holistic approach can bring peace to those like Shingi who are experiencing distressing symptoms to help live as actively as possible as well as help the family to cope during their illnesses and in their bereavement.
-
Reading: Bereavement (5 min)
Death within a family system has a profound impact on the remaining subsystems. This is because of attachments or bonds that exist between family members or subsystems. Breaking these ties may result in anger, anxiety, depression, and emotional detachment.
Bereavement is a physical loss or deprivation of a person or object to whom one is attached.
(Source: Island Hospice Manual, Zimbabwe)There are many ways that one can experience bereavement or loss:
- Death of someone close
- Death of a pet
- Disability
- Retirement
- Migration
- Loss of a job/employment
- Separation or divorce
Grief and Mourning
Grief is the normal internal feeling one experiences in reaction to a loss, while bereavement is the state of experiencing that loss. It is a process and a self-healing way of recovering from loss. It acts as a healing process and can be associated with physical symptoms. At times it can be an intense, painful process that clients should be helped to work through.
As opposed to grief, mourning is the outward expression of that loss. Mourning usually involves culturally determined rituals that help the bereaved individuals make sense of the end of their loved one’s life and give structures to what can feel like a very confusing time. Essentially it means the individual’s effort to accept that a loss has occurred. Therefore, while the internal pain of grief is a more universal phenomenon, how people mourn is influenced by their personal, familial, cultural, religious, and societal beliefs and customs.
Mourning customs also affect how comfortable bereaved individuals may feel about seeking support from others as well as the appropriate ways for their friends and family to express sympathy during this time. For example, in Shingi’s case, it is likely she is still mourning the loss of her mother and she may differ in how much or how little she may talk about her loss with friends and family.
As a healthcare worker, it is important to determine whether or not participating in a bereavement support group or psychotherapy is acceptable. Bereavement counseling supports and encourages the bereaved to restructure their world and deal with their pain.
-
Case Study: Shingi (5 min)
Let’s revisit Shingi’s case. She is complaining of headaches, is unable to concentrate in school, and says she has no friends and is unhappy at school and at home. It is obvious that her aunt cares for her and is concerned about the change in Shingi and asks you if this is due to the HIV. She also says she heard that Shingi should start on ARVs according to the new ARV guidelines released by the ministry of health.
Shingi tells you that she misses her mother and she wants to go to her grave to see where she was buried. She did not attend the funeral service and burial as her grandmother said she was not old enough to understand what was happening when her mother died. Shingi says she would like to die and go to be with her mother, even though she knows that her aunt does care for her.
-
Reading: Psychosocial Support and HIV (5 min)
Psychosocial support (PSS) was defined earlier as an ongoing process which aims to meet the physical, emotional, social, mental, and spiritual needs of children and their families. Psychosocial support in HIV encompasses care of the mental, emotional, and social needs of people who test HIV positive, their families and the community. After a positive HIV test, clients may feel helpless, stigma from their community, and emotional. This is a crucial time to offer a psychosocial intervention.
Importance of Support Groups
Support groups are important for ongoing adherence support and counselling for PLHIV. Members can come together to engage in income-generating/livelihood programmes. Examples of support groups include adolescent, young mothers, and men’s support groups. Psychosocial support for adults should be provided by the health care worker. Unfortunately the reality of overcrowded services and overworked staff does not often allow for this to take place. Therefore, you as a health care worker play an important role in setting up support groups. Where possible, you should refer the individual to a local support group. These groups are often run in the community by non-governmental organisations or self-help groups.
Support groups should provide:
- A group facilitator. He or she will help generate a programme that includes a variety of structured activities and discussions of personal problems.
- A safe and caring environment. This environment will provide a spacein which people with HIV and AIDS can support and encourage each other, share ideas and experiences, and empower themselves. If members are at various stages of HIV infection, those at more advanced stages are able to empathise with, and support, those at earlier stages.
- Confidentiality. The members of the support group are sometimes the only people, apart from the counsellor, who know an individual’s status.
Psychosocial Support for Children and Adolescents
As covered earlier in the training, when children are diagnosed to be HIV-positive and informed of their status, they face a lot of psychological issues and emotions, which include fear, sadness, grief, and anger. Health care workers should be able to assess the different needs of the child and caregiver at any given time or point of contact, and to ensure that these needs are addressed.
Follow-up counselling, care, and support aims to reduce the impact of stressors by:
- Equipping the children and caregivers with accurate, honest information.
- Assisting the children and caregivers to develop coping strategies to reduce the impact of the challenges that they face.
- Ensuring that children receive the most appropriate care and support in order to meet their complex, evolving physical, social, emotional, mental, and spiritual needs.
- Protecting the best interests of the child at all times.
-
Reading: Creating Support Groups (5 min)
When creating support groups, follow these steps:
- Identify the interested people/clients.
- Approach them one-by-one as individuals (single people) and as couples (those married), and clearly outline the advantages of them joining.
- Find out from them whether they would be interested in joining a support group. Do not force them! Given them a chance to make their own decision.
- If they are interested, make a list of names and classify them by type of support group they would want to join (singles sessions, couples sessions, or mixed groups).
- Come up with a list of activities to embark on as a support group.
During your first group meeting you will want to:
- Introduce all group members and discuss support group objectives.
- Assist the group in setting expectations, duties, and responsibilities of each group participant.
- Facilitate the group to elect a group co-coordinator if needed.
- Guide the group in developing ground rules, which include discussions about confidentiality and disclosure to other members outside the group.
- Ensure that the group is viable, sustainable, and produces results that benefit members.
- Have the group set goals they want to achieve and decide how they intend to achieve these goals.
- Assist the group in securing an appropriate venue for their meetings. The members determine the venue as they wish (e.g., church, health centre, community hall).
- Encourage the group to meet regularly. Members decide on how often they want to meet. Once a month should be sufficient for groups.
- Come up with a list of topics the group would like to address.
- Provide education on reproductive health, family planning, HIV and AIDS issues (such as safer sex, disclosure, stress, nutrition).
- Link them to service providers or resources.
- Ensure a system where emergency meetings can be called to urgently address important issues.
- Monitor the activities through an agreed reporting format that the group decides upon.
-
Case Study: Tawanda (5 min)

Tawanda is a 15-year-old boy living with his mother and younger sister who has been transferred to your OI clinic as they have recently relocated from a neighbouring town. Tawanda was commenced on ARVs at the age of 8 years after he was admitted in hospital for meningitis. He is not aware of his HIV status and his mother does not want him to know until she thinks he is ready. She is worried that he will become depressed and stop taking his treatment, and that he will be angry with her. She tells him that the medications are for allergies which he suffers from.
When you see Tawanda for the first time, he seems intelligent and asks a lot of questions about the clinic and his medications.
Tawanda comes to the OI clinic for his routine visit three months later and tells you that he has discovered on the internet, that the medication he is taking is ARVs. He is angry and wants to know why he has not been told the truth. He is very angry with his mother for lying to him and wants to know why the nurses also did not tell him the truth about his HIV status. Mum is in tears.
-
Quiz: Knowledge Check (10 min)
-
Reading: Key Points (5 min)
- Bereavement counselling supports and encourages the bereaved to restructure their world and deal with their pain.
- Children and adolescents experience grief and bereavement through a wide range of reactions.
- Palliative care addresses physical, psychological, spiritual, and social needs of the client and their family.
- There are ethical rules and principles to providing quality palliative care.
- Palliative care is an interdisciplinary effort.
- Offering psychosocial support to clients can assist in coping skills as well as connect the client to their community.
- Forming support groups is a great way to offer psychosocial support.
- Support groups should be formed and maintained by group participants while counsellors should remain in a supportive role to the group’s needs.
