Session 5: Nutrition for PLHIV
In this session, you will learn about the importance of good nutrition for persons living with HIV (PLHIV). The session begins by looking at food and nutrition programmes. It covers the importance of providing nutritional counselling, care, and support to PLHIV as soon as they are diagnosed. It also addresses the unique nutritional needs of someone who is HIV-positive and how to best educate PLHIV about nutrition, energy needs, and food preparation.
Learning Objectives
By the end of this session you will be able to:
- Explain the importance of good nutrition in the context of HIV infection.
- Describe how HIV can affect the nutritional status of a person.
- Explain the nutritional requirements of PLHIV.
- Monitor nutritional status of children, adolescents, and adults.
-
Reading: Introduction (10 min)

Faith is 20 years old and attending university for a degree in computer science. She began seeing a provider at a clinic near the university for treatment of depression after feeling sad last semester when she did not do well on her mid-year examination. She was advised by her provider to start a mild antidepressant which has helped, but she still experiences periods of sadness as well as anxiety when projects are due or examinations are coming up. On her last clinic appointment, Faith was complaining of more fatigue than usual, poor appetite with a 2 kg weight loss, and pain on urination. She agreed to an HIV test since she reported unprotected sex with her current partner who she thought had a negative HIV test. Faith’s HIV test result was positive, and she began taking ART (EFV/TDF/3TC=FDC).
Faith has returned to the clinic prior to her scheduled appointment to meet with the HTC counselor. She has not disclosed her HIV status to anyone, including her current partner who she has not seen or talked too since his work takes him back and forth to South Africa.
At the last clinic visit, Faith’s provider asked her to complete the Shona Symptom Questionnaire. Faith’s score was 7. Her provider discussed the results with Faith and based on her continued symptoms of depression, she was referred for counselling. Her provider also increased the dose of her antidepressant. Faith has also lost another 1 kg since beginning her ARVs and told her provider that she just does not have a good appetite and sometimes forgets to eat since she falls asleep as soon as she finishes her classes. Sometimes she sleeps so late that she does not have time for breakfast.
Outreach Services
As a healthcare worker, it’s vital for you to provide comprehensive care for children, adolescents, and adults living with HIV. Depending on the clinic and healthcare centre where you work, it may not be possible to directly provide these services yourself. In these instances, you will need to know which services are essential for PLHIV so that you can refer clients appropriately.
For example, in the story above, we met Faith. She has significant signs of depression that have not adequately responded to the antidepressant that the provider prescribed. In her situation, she would greatly benefit from comprehensive mental health and psychosocial support from a psychologist (if available) or a counselor. Food and nutrition programmes may also be valuable for her to address her continued weight loss and poor appetite. Keep in mind that her poor appetite may be due to her depression, which supports the need for a referral to a counselor.
In order to ensure that ART and prophylactic medications are taken properly, you will see PLHIV clients at regular intervals. Depending on the situation, you may need to refer clients for additional services during one or several points while they are under your care. The need for referrals may occur during initial testing and counselling, at the beginning of treatment, or even after an ART regimen has been established.
Throughout this training you will learn about key services that should be offered to persons living with HIV (PLHIV) as part of their basic package of care.
-
Case Study: Faith (5 min)
Let’s return to Faith. She has been taking ART for six months. Initially she came to her appointments on time and in fact, was seeing the HTC counselor weekly. The last three months, she has been late for her appointment, but always reported that she had not missed any doses of medication stating that “she had pills left in her container, so she did not run out”. She continued to complain about feeling sad, but also angry and confused about her diagnosis. Her partner has not returned from his work in South Africa, and she has not heard from him so has not disclosed her status. She decreased the number of classes she was taking since she was having trouble concentrating. Her weight during the initial three months on ART remained the same, but she was not able to put back the weight she lost initially.
Faith is in clinic today for her six-month appointment. She reports trouble swallowing for the past week, increased fatigue, and just not feeling well. She thought she might have gotten a cold from some of her classmates since many at the school were sick. On examination, it was noted that Faith had oral thrush and possibly esophageal candidiasis. She had lost an additional 2 kg of weight and her temperature was slightly elevated at 37.7C. She also reports missing the last two days of her ART medication due to trouble swallowing.
-
Video: Nutrition and PLHIV (10 min)
Watch the following video on the importance of nutrition for PLHIV:
-
Reading: HIV and Its Impact on Nutrition (10 min)
HIV can have a significant impact on an individual's nutritional status. It can cause reduced food intake, lower food absorption, and increase energy requirements. Tap on the following tabs to learn more.
Reducing food intake
There are a variety of reasons why PLHIV may experience reduced food intake. First, painful sores in the mouth or throat may cause difficulties eating or swallowing. In addition, PLHIV may experience altered food taste, nausea, vomiting, diarrhoea, or abdominal cramps. Often these conditions are caused by medication side effects. All around, PLHIV may have poor appetite due to tiredness, depression, and other psychological factors. Their illness may also result in less quality and quantity of food in the household due to insufficient money, inability to grow crops, or difficulties in shopping and preparing food.
Lowering food absorption
During digestion, the food we eat is broken down into small parts called nutrients. These nutrients are absorbed through the gut and sent into the bloodstream where they are used by the body. HIV, as with other infections, can damage the gut and breakdown cells, both of which reduce the body’s ability to absorb nutrients. In addition, PLHIV frequently experience co-infections such as diarrhoea that make food pass too quickly through the gut, reducing the time for digestion and absorption. For PLHIV, poor absorption can cause difficulty in controlling blood sugar levels, which may lead to diabetes.
Increasing energy requirements
PLHIV have higher energy needs than healthy HIV-negative adults. These energy needs are influenced by the client’s age, clinical stage, and symptoms. If food intake and absorption are not sufficient for meeting these increased needs, muscles break down. This breakdown is referred to as muscle wasting . In turn, muscle wasting leads to weight loss and swelling of the feet or other parts of the body. It also causes reduced production of saliva and other digestive fluids needed to break down foods into nutrients, which further reduces the absorption of food.
Nutritional Requirements for PLHIV
The nutritional requirements of PLHIV are influenced by age and physiological changes caused by pregnancy, breastfeeding, physical activity, clinical stages of health, metabolism, and viral load count. See the following table for more details about nutritional requirements:
Client Daily Energy Requirements Dietary Recommendations HIV-negative healthy adults 1999-2580 kilocalories HIV-negative adults who are serving as caregivers for PLHIV need to know about the importance of nutrition for PLHIV. Educate them on the importance of having PLHIV eat a variety of foods and show them how to store and prepare foods safely. PLHIV adults (early/asymptomatic) 10% more energy (additional 210 kilocalories) These clients need one additional fistful of maize meal or one cup of porridge daily. PLHIV adults (late/symptomatic stage) 20-30% more energy (additional 420-630 kilocalories) These clients need two to three additional fistfuls of maize meal or two to three cups of porridge daily. PLHIV children (early/asymptomatic) 10% more energy Focus on alleviating symptoms and providing support to the client and caregiver. PLHIV children (symptomatic with poor weight gain) 20-30% more energy PLHIV children (severely malnourished) 50-100% more energy -
Reading: ART and Its Impact on Nutrition (10 min)
Just as there is a close link between HIV and a person’s nutritional status, there is also a similar connection between ART and nutrition. For example, foods can impact a clients's ability to absorb, distribute, and metabolise medications. On the other hand, medications can impact a client's ability to absorb, distribute, and metabolise nutrients. In addition, the side effects caused by certain ART medications are also linked to food intake and absorption just as the combination of certin foods and medications can cause unhealthy side effects.
For ART to be effective and for clients to adhere to their medications, there must be good nutrition. But, this can be difficult when ART side effects like oral sores, altered taste, loss of appetite, nausea, and diarrhoea reduce food intake. Conversely, for most clients who take ART properly, nutritional well-being improves as their viral load becomes suppressed and HIV-related symptoms which can lead to reduced food intake dissipate.
Given that ART and nutrition are so closely linked, you should offer care and support on both topics when you meet with PLHIV clients. Encourage your clients on ART to maintain adequate nutrition as it is one of the most important things a newly infected person can do to prolong their general well-being. It can lead to a healthy lifestyle, preservation of health, improved quality of life, prolonged independence, and a delay in disease progression. In addition, talk to your clients about strategies to prevent food and water-borne infections, as doing this will reduce the risk of diarrhoea. Also help your clients manage common HIV-related symptoms so that these symptoms do not negatively impact their nutritional status. Finally, work with them to continue physical activity and exercise, which will lead to an increase in energy, appetite stimulation, and the building up and preservation of lean body mass.
You will also want to counsel your clients on specific dietary restrictions that they should follow depending on the ART medications that they are taking. The following chart shows important dietary recommendations that you will want to make your clients aware of according to their medications:
ART Dietary Recommendations Zidovudine (AZT) Take on an empty stomach. If this is not possible take with low fat meals as high-fat meal reduce drug absorption. Avoid alcohol. Stavudine (d4T) No dietary restrictions. Nevirapine (NVP) No dietary restrictions. Avoid St. John’s wort. Lamivudine (3TC) No dietary restrictions. Avoid alcohol. Efavirenz (Ef2) Avoid fatty foods. Avoid alcohol. Didanosine (ddl) Take 1 hour before or 2 hours after a meal. Drink at least 1.5 liters of fluids daily. Do not drink grapefruit juice, as it may lower the level of medical effect in the blood. Avoid St. John’s wort. Indinavir (IDV) To be taken 1 hour before or 2 hours after a meal. Drink at least 1.5 liters of fluid daily. Do not drink grapefruit juice, as it may lower the level of medical effect in the blood. Avoid St. John’s wort. Atazanavir Take with food Tenofovir No dietary restrictions Abacavir No dietary restrictions Lopinavir No dietary restrictions Dolutegravir No dietary restrictions -
Reading: Nutrition Care and Support for PLHIV (5 min)
As a healthcare provider, there are many opportunities where you can provide nutritional care and support to PLHIV clients.
The following image shows key moments during a client's care where this kind of support can be offered.
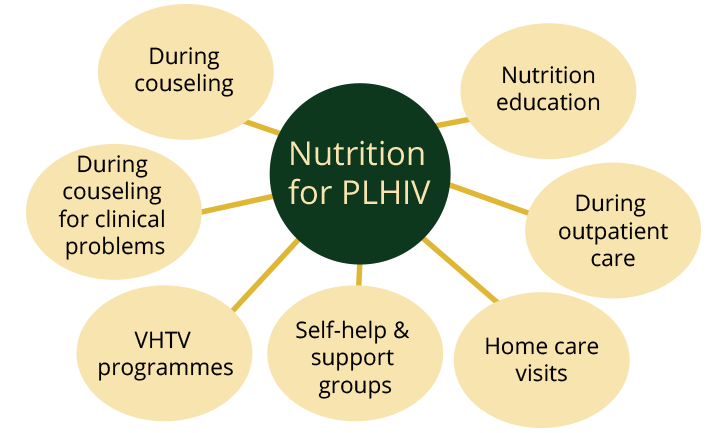
The type of care that you provide a client may also depend on the stage of their disease. Good nutrition is particularly important at the initial stages of HIV infection. Nutrition counselling and education at this early stage gives the client a chance to build up healthy eating habits and to take action to improve access to food and adopt other healthy practices. In the early stages of HIV, encourage the client to “stay healthy”, build stores of essential nutrients, maintain weight and lean body mass, and ensure a correct understanding of food and water safety. As the client enters the middle stages of the disease, focus on minimising the consequences by maintaining dietary intake during acute illness, increasing the nutrient intake for recovery/weight gain, and the continuation of physical activity. During the late stages of HIV, provide comfort for the client. Also, treat opportunistic infections, modify the diet according to symptoms, and encourage eating and physical activity.
-
Reading: Nutritional Education (10 min)
Let’s go back to Faith. If you were meeting with her to counsel her on nutrition, you would want to start by explaining to her about what makes up a balanced diet, focusing on readily available foods.
You could also help her think of ways to adapt her diet for times when she is unwell, especially for times when she is experiencing diarrhoea, nausea, vomiting, or oral thrush.
Tap on each symptom to read about its causes and how to manage through nutrition.Diarrhoea
Symptoms of diarrhoea include loose watery stools, more frequent than usual.
Causes
- Bacterial or viral and fungal infections
- Food poisoning
- Medications (especially antibiotics)
- Poor absorption or intolerant to nutrients (e.g., lactose and sugar)
Dietary Management
- Drink oral rehydration salts
- Drink sufficient fluids (e.g., water)
- Eat small, frequent meals
- Eat fermented foods (e.g., mahewu, sour porridge)
- Include soluble fiber found in bananas, oats, peeled apples and pears, carrots, and pumpkins
- Avoid fatty foods
Fat Intolerance, Steatorrhoea (fat in the stool)
Causes
- Malabsorption of fat
- Incomplete digestion of fat
- Malnutrition
Dietary Management
- Eat soft, mashed, liquid foods like soup, porridge
- Squeeze lemon juice on meat and fish to improve digestion
- Eat lean meat
- Do not fry foods or add a lot of cooking oil
- Avoid fatty foods such as potato chips, butter, mayonnaise, and cream
Nausea and Vomiting
Causes
- Medications
- Infections
- Food with wrong aromas
- Food intolerance
Dietary Management
- Take small frequent meals
- Cool or cold meals are better tolerated than hot meals
- Take fresh lemon juice in the morning
- Sour or salty foods are better tolerated than sweet food
- Avoid greasy, high fat, and spicy food
- Avoid taking fluids with meals
- Do not lie down right after eating
- Avoid the smell of cooking and foods with strong aromas
Change in Taste
Causes
- Stress
- Side effects to medication
- Illness like colds, flu, and malaria
Dietary Management
- Add seasoning to give more flavour to food
- Marinate meat and poultry
- Use lemon, raw tomatoes, and tonic water to stimulate taste buds
- Use a straw to bypass taste buds
- Try different meals
- Chew food well
Candida, Thrush, Mouth Sores, Chewing Difficulties
Causes
- Infection
- Weakened immune system
- Antibiotic therapy
Dietary Management
- Try soft non-irritating foods such as scrambled eggs, pureed pumpkin, pawpaw
- Eat fermented food such as yoghurt, mahewu, sour milk
- Avoid hot food. Cold food can be soothing
- Yeast promoting food such as sugar, bread, and beer should be avoided
- Avoid acidic foods such as citrus fruit, vinegar, and spicy foods
Loss of Appetite or Anorexia
Causes
- Chronic infection
- Drugs or medication
- Malnutrition
- Monotonous meals
- Stress, anxiety, and depression
- Noxious smells and odours
Dietary Management
- Eat small frequent meals and nutritious snacks
- Try to make meals attractive and appetizing
- Eat foods that are more energy dense
- Avoid drinking liquids before taking a meal or during a meal
- Avoid fatty food and sweets
- Avoid preparing meals
Fatigue
Symptoms of fatigue include poor performance, inactivity, loss of concentration, looking miserable, and burnout.
Causes
- Pain or illness
- Stress
- Depression
Dietary Management
- Eat food that is easy to prepare and easy to chew
- Eat fresh fruit that does not require preparation
- Eat nutritious snacks throughout the day
- Drink high energy and high protein liquids such as mahewu
- Have someone else prepare food to avoid fatigue
- Rest as much as is possible
Fever
Symptoms of a fever include a high temperature, fast breathing, dry mouth, looking ill, and/or feeling lethargic.
Causes
- Infection
Dietary Management
- Eat high energy and high protein meals such mutakura and nhopi
- Drink plenty of fluids and fruit juice
- Drink nutritious fluids often such as milk, sour milk, and mahewu
Cold, Flu, Coughs, Sneezing, Running or Blocked Nose, Sore Throat
Causes
- Infection
- Allergies
- Tuberculosis
Dietary Management
- Take high energy high protein fluids
- Eat fruit or drink fruit juice
- Sprinkle sugar onto an onion that has been cut in small pieces and let it soak in water to make syrup. Drink this slowly to soothe the throat
- Drink ginger, cinnamon, or lemon tea with honey
- Avoid very cold foods and drink
In addition to talking to Faith about nutrition, you will want to go over food hygiene practices including strategies for handling food safely. You could focus this discussion on handwashing, preparing food on clean surfaces, using clean utensils, and washing fruit and vegetables.
Next, you will want to explain to Faith the importance of physical exercise. If excising is something she doesn’t do on a regular basis, you could help her establish a physical exercise routine that would help her to develop her muscles.
Last, you will want to encourage her to consult a health care worker early if there are any signs of infection.
-
Reading: Eating Wisely Guidelines (10 min)
You can use the following Eating Wisely Guidelines when working with clients like Faith. Let them know that eating wisely will help them live healthy longer. Following the guidelines below will also ensure that their food intake is adequate for meeting their nutritional needs.
Enjoy a variety of foods
When working with clients, educate them on the importance of eating a variety of different foods in order to get essential nutrients. No single food or group of foods contains all the nutrients that the body needs in the right quantities and combinations, except breast milk for infants up to six months. For this reason, it’s important for clients to eat a variety of foods from the different food groups and alter their methods of preparing their meals.
While it might not be possible to have variety of foods at each meal, encourage them to try to include a variety of foods throughout their day. Clients should try to select foods that are in season and locally available. They can buy fruits and vegetables that are in season, such as oranges and traditional green leafy vegetables. This can make eating enjoyable, healthy, and affordable. Fruits and vegetables can also be grown at home.
In addition, recommend that clients try different methods for cooking their food. For example, instead of always frying food in fat or oil, clients can try steaming, baking, and grilling. Remind clients that vegetables need not always to be cooked and can be consumed raw as long as they are cleaned thoroughly. For example, instead of always stewing vegetables, they can be eaten fresh as a salad.
An example of a mixed meal of optimal variety is one made up of maize-meal, chicken, pumpkin and spinach. Foods in this meal can be replaced with other foods on different days. For example, instead of always making this dish with chicken, other meats, animal products, or legumes can be used in place of the chicken.
Make staples or starchy foods the largest part of your meal (maize meal/sadza)
In addition to recommending that clients eat a variety of foods in their diets, inform them that staple foods or starchy foods, such as maize meal or sadza, should be eaten with every meal. These foods are relatively cheap and are a good source of energy. For this reason, they should make up the main food of each meal. Clients can plan the rest of their meals around these staples. Staples eaten alone, however, are not enough to ensure adequate variety of food or to provide all the nutrients that the body needs. For this reason, a healthy diet needs to include other foods as well. The following chart shows examples of staples or starchy foods:
Cereals and Grains Starchy Roots or Tubers Starchy Fruits Maize/Corn Meal
Millet
Rice
Sorghum
Wheat flour
Cassava (fresh)
Cassava (flour)
Potato
Sweet potato
Yam
Breadfruit
Plantain
Eat pulses and legumes, nuts and oilseeds, if possible every day
Pulses, legumes, nuts, and oilseeds help develop and repair the body as well as build strong muscles. As they are cheaper sources of protein than animal products, such as beef and chicken, you should recommend that clients eat these foods every day, if possible. To help with digestion, these foods may require thorough cooking. Inform clients that soaking beans and peas in water prior to cooking them and using locally-made, fuel-efficient cookers will reduce the amount of firewood needed to cook them well. The following chart shows examples of pulses, legumes, nuts, and oilseeds:
Pulses and Legumes Nuts and Oilseeds Chickpeas
Cowpeas
Kidney beans
Lentils
Pigeon peas
Ground nuts
Melon seeds
Peanuts
Peanuts
Pumpkin seeds
Sesames
Soybeans
Eat poultry, meat, fish, eggs, milk, and milk products regularly
Poultry, meat, fish, eggs, milk, and milk products are useful for growth and repair. They help with the formation of blood and strengthen muscles and the immune system, which in turn fights infections. While these foods may be relatively expensive, it is important for clients to include even small portions of these foods in their meals as often as possible.
When educating clients about nutrition, inform them that liver and other organ meats, or offal, are particularly valuable for the formation of blood. Additionally, let them know that fermented milk is beneficial if they have diarrhoea because it is easily digested. It may also help in digestion and absorption of other foods and is a good source of energy. An added advantage to fermented milk is that it does not need refrigeration.
For clients or caregivers providing care for infants and young children, reinforce that breast milk is a great food for these age groups. The following chart shows examples of poultry, meat, fish eggs, milk, and milk products:
Milk and Milk Products Poultry, Meat, and Fish Cow milk (fresh)
Goat milk (fresh)
Fermented milk
Cheese
Curd
Yoghurt
Breast milk (for infants and young children)
Chicken, turkey, duck, geese, etc.
Beef (cow, bull)
Goat
Lamb (sheep)
Pork
Rabbit
Deer
Fish
Insects
Organ meats/offal (e.g., liver)
Eggs
Eat a wide variety of vegetables and fruits everyday
Educate clients on the importance of including vegetables and fruits as part of a healthy diet. Not only do these foods keep the body functioning, they also keep the immune system strong and help with preventing and fighting infections. For this reason, they are referred to as “protective foods” and are essential for PLHIV. Most vegetables and fruits can be easily grown in home gardens. Encourage clients who do not have access to land for a home garden to consider organising communal gardens.
When working with clients, inform them of the beneficial properties of different types of vegetables and fruits. For example, those that are dark-green, yellow, orange, or red in colour are rich in vitamin A, which is an essential nutrient for good vision and growth. Green leafy vegetables, such as spinach, pumpkin, cassava leaves, green pepper, apricot, papaya, mango, and carrots are all foods that fit in this category.
Additionally, vegetables and fruits that are rich in vitamin C, such as cabbage, tomatoes, baobab fruit, guava, lemons, oranges, and pineapples are valuable for fighting infections. In order to ensure that vegetables do not lose some of their nutritional value during cooking, recommend that clients only cook them for as short a time as possible and reuse the cooking water in soups and other foods.
Use fats and oils as well as sugar and sugary foods regularly, but in moderation
As explained in previous sections, quite frequently PLHIV will have poor appetite because of their illness or as a result of the medications that they are taking. Oils, fats, sugar, and sugary foods add flavour to food, thereby stimulating appetite. Encourage clients who need to increase their body weight to add extra quantities of oil, fat, and sugar to their diets. Foods in this category are also rich in energy and therefore are important foods for clients to eat to improve energy intake.
There are two special cases where clients will need to be cautious with their intake of fats, oils, and sugars. Clients with candida (oral thrush), should limit the amount of sweet foods such as sugar, honey, and sweet fruits and drinks that they ingest as sugar intake can worsen this condition. In addition, clients with excess weight gain should also be advised to limit their consumption of these types of foods as weight gain can lead to health problems, such as heart disease. With these clients, closely monitor their weight and advise them to adjust their fat and sugar intake as appropriate.
Drink plenty of clean and safe water
Water is important for life and is necessary every day. An average adult needs about two to three litres or eight large cups of fluids each day. This daily requirement is increased when it’s very hot outside or when a person is working or sweating.
As a healthcare work worker, it’s important to keep in mind that some medications may not work well if the person is dehydrated. PLHIV who are suffering from diarrhoea, vomiting, or fever need to drink even more liquids to replace the water that they have lost. If you are working with a client who is breastfeeding, she will also need extra water.
Children also need adequate water. Let their caregivers know that it’s important that children stay hydrated so that their medications work properly. Infants below six months of age who are exclusively breastfed do not need extra water.
When educating patients about water, start by going over water sterilization processes. If a client is drinking water that is collected from a protected well or river, the water should be boiled for at least 10 minutes and stored in a clean container. Also teach them how to monitor if they are drinking enough fluids. They can let thirst be their guide. If they are frequently thirsty, then this is a sign that they should increase their fluid intake significantly. Last, let clients know that in addition to drinking clean water, fluids can also come from juices, soups, vegetables and fruit, as well as meals that have gravy or sauces. Clients should be cautious, however, on relying only on tea, coffee, and alcohol drinks as source of water as these beverages can interfere with absorption of nutrients and may interact poorly with medicines. Alcoholic drinks remove water from the body making them an ineffective source of fluids.
Ensure that you are eating the optimal quantity of meals at the right frequency
As explained in previous sections, PLHIV have increased energy needs. For this reason, you should encourage clients to increase the frequency of their meals and snacks. Explain to them that it’s easier to eat wisely if they eat three or more times daily, rather than having large meals once or twice in the day. Having small and frequent meals about three to four hours apart every day helps to increase energy intake.
They should also increase the amount and variety of food consumed during each meal. Clients may feel uncertain about if they are eating the right amount of food. Tell them that the simplest way of knowing if they are eating enough food is to monitor their weight. If their weight is within the “normal range” for their age group and height, then they are eating the right amount of food. They can also use common utensils, such as cups and spoons, to measure portion sizes to ensure that they are getting the right quantities of different food types in each meal. Client can also enhance their diet with nutrient-rich foods such as foods fortified with essential nutrients.
-
Reading: Monitoring Nutritional Status (10 min)
When working with PLHIV, it’s important to monitor their nutritional status as part of their routine clinical care. This applies to HIV-positive adults, adolescents, and children.
For example, if Faith came for a visit to your clinic, you would want to take her weight, height, and BMI (body mass index). This would tell you how well she was doing nutritionally. If Faith became pregnant or instead if you were working with a child, you would also want to take a MUAC (mid-upper-arm circumference) measurement. Tap on the following tabs to learn more.
Weight
When monitoring clients, you will want to measure their weight on each visit.
Height
The frequency that you measure clients’ height depends on their age. For adults, you will only need to measure their height on their initial visit. For children and adolescents, you will want to measure their height on each visit. If the child is below five years of age, plot his or her height on the Child Health Card. If the child is older than five, compare his or her height against standard charts of height available at your health centre.
BMI
During each visit, you will want to calculate a client’s BMI or body mass index. This calculation is done by dividing a client’s weight in kilograms by their height squared:
BMI = weight (kg) ∕ height2(m2)The BMI gives an indication of the client’s nutritional status. For example, a BMI of 18.5 to 25 may indicate optimal weight, but a BMI of lower than 18.5 suggests that the client is underweight. A BMI of above 25 indicates that the client is overweight.
MUAC

MUAC, or mid-upper-arm circumference, is an ideal screening measure for assessing undernutrition as it uses simple equipment that is easy to carry to field sites and requires minimal training. The MUAC should be measured in all children between the ages of 1 to 13 years and in pregnant women. Unfortunately, MUAC cutoffs for undernutrition are only available for children and adults and for this reason MUAC is not an appropriate strategy for monitoring adolescent clients.
To measure MUAC, you will wrap a flexible measuring tape around the midpoint of the client’s mid-upper arm. You can find the midpoint by first locating the tip of the shoulder. Then, with the elbow bent, find the tip of the elbow. Next, place the tape or string at the tip of the shoulder and extend it to the tip of the elbow. Mark the midpoint between the tip of the shoulder and the tip of the elbow. Last, slide the tape around the midpoint and take the reading.
Source: UNICEF. Nutrition in Emergencies. Measuring under-nutrition in individuals. Minilesson 3.1.3. Measuring Mid-Upper Arm Circumference.There are many types of MUAC tapes including some with colours and numbers and ones with just colours. The colours red, yellow, and green indicate the level of malnutrition. It is recommended that you use the MUAC tape released in 2009 that is shown in the picture below.

This tape uses the following measurements:
- Red < 115 mm
- Yellow 115 mm to 125 mm
- Green > 125 mm (corresponding with the new cut- off of severe acute malnutrition of less than 115 mm)
-
Case Study: Kamail (5 min)

Kamali is two years old and is brought to the clinic by her grandmother, Mudiwa, who tells you that Kamali has not been eating well for several weeks and seems tired all the time.
Kamali’s mother died shortly after she was born apparently from prolonged bleeding. She was not able to get to the hospital in time since they lived very far. Kamali’s father could not care for her so her grandmother has been raising her. Mudiwa has tried to keep the clinic appointments for vaccinations but it has been very hard since she has health problems which affect her walking. Mudiwa also has a small Tuck shop that she must work at to have the money that is needed to raise Kamali.
Reviewing Kamali’s clinic booklet you notice that she has been seen in the clinic for frequent ear infections. You also note that Kamali has not been gaining weight and in fact, her weight today is 9 kg; a 2 kg weight loss since her last visit 7 months ago. On examination you note that Kamali has a moderate amount of oral thrush, her lungs are clear, abdomen soft with no tenderness noted. Her temperature is 37.2C.
At her last visit, another clinic provider suggested that Kamali be tested for HIV but Mudiwa became very upset and refused the test saying that “her daughter did not have the virus and died after giving birth”. After discussing Kamali’s symptoms with Mudiwa and offering support and counseling, she agreed to the HIV test, which was positive.
If you are working with a childlike Kamali who is experiencing growth failure, this could be a sign of an undiagnosed HIV infection. The clinic providers were wise to suggest HIV testing when measurements showed that Kamali was losing weight as it’s common for children who are HIV-positive to experience reduced weight and height. As you work with HIV-positive children, you will notice that their faltering in growth often occurs before OIs or other symptoms. Initially the wasting occurs in lean body tissue and later on impacts the child’s fat mass. Children with severe growth failure and loss of muscle (lean body tissue) are at increased risk of mortality.
-
Reading: Monitoring and Management of Children (10 min)
You will want to assess an HIV-positive child’s growth on a regular basis. This can help you to monitor the HIV disease progression and will allow you to identify complications early on and get the child the necessary counseling and treatment. You will want to plot a child’s growth on the Child Health Card and measure the child’s weight and height every month.
Management of Increased Energy Requirements
As soon as a child is infected with HIV, there is an increased energy requirement of 10%. When counselling a child’s caregiver, let them know of this increased need. More specific nutritional needs for HIV-infected children and adolescents depend on their age, stage of disease, the presence of acute or chronic infections, and their treatment.
The World Health Organisation (WHO) recommends that children with symptomatic HIV need 20-30% more energy. Symptomatic children with severe malnutrition, however, require up to 100% more energy. Providing this kind of increase in energy is only possible through the provision of supplements, such as F75 or F100 for inpatients, and plumpy nut for children who are being managed as outpatients. The nutritional needs of children and adolescents are best met through a sufficient, balanced, and varied diet. Furthermore, in order for ART regimens to achieve full benefits, children and adolescents require appropriate and adequate nutrition.
Impact and Management of ART
When you first initiate an ART regimen with a child, he or she will begin to gain weight and height, although height gain is slower than weight. While the child is on ART, it’s important to continue to monitor his or her growth as it is often an indicator of treatment failure. ART can change the way a child’s body uses fats, proteins, and energy, but these metabolic changes can be managed by nutrition counselling. If a child is doing well on ART and their viral load becomes suppressed, their losses in weight and height will begin to reverse. For this reason, if a child on ART is experiencing growth failure or severe malnutrition not due to food insufficiency, it may be a indicator of the presence of an OI or treatment failure. As a child on ART begins to gain weight, make sure to adjust his or her dosage of ART as the dosing of ART is weight dependent.
-
Quiz: Knowledge Check (10 min)
-
Reading: Key Points (5 min)
- Poor nutrition in PLHIV worsens the effects of HIV by further weakening the immune system, leading to more rapid disease progression.
- Nutritional care and support, which includes counselling, education, monitoring, and the provision of food, is an important component of the care of PLHIV.
- Monitoring of the nutritional status of PLHIV is an important part of routine clinical care.
