Session 6: Sexual and Reproductive Health Rights
This session will cover the benefits of integrating sexual and reproductive health rights (SRHR) and HIV services. You will review the services offered in both areas and see examples of SRHR and HIV integration for different levels of care. You will also learn about the value of integrating SRHR and HIV services at programming and policy levels. Next, you will learn about the minimum package of services for SRHR and HIV integration developed by the Ministry of Health and Child Care. Last, you will learn about how to work with PLHIV clients in regards to family planning.
Learning Objectives
By the end of this session you will be able to:
- Provide basic SRHR information and management of SRHR needs of PLHIV.
- Discuss the components of an SRHR service.
- Describe family planning.
-
Case Study: Nyasha (5 min)
Nyasha is a 24 year-old HIV-positive woman. She works as a primary school teacher in Gweru. Although she has known about her status for several months, this is the first time she was able to come to clinic and would like to begin taking HIV medications. During the visit, she mentions that she is pregnant. A test confirms that she is and estimates her to be about 22 weeks along. The health care worker counsels her on the ART medication that she will need to take and about adherence, possible side effects, and steps to take to prevent transmitting HIV to her baby.
Following this session, she is sent to another room where she meets with another health worker who talks to her about antenatal care. This worker goes over proper nutrition and vitamins she should take to make sure that she and the baby stay healthy. The worker also encourages Nyasha to continue to come back throughout her pregnancy and afterwards for continued pregnancy and HIV support and care.
Nyasha is particularly pleased with being able to meet with two healthcare specialists in one place and at one time instead of scheduling multiple visits. She also likes feeling like there was a health care team there to support her. Before Nyasha leaves the clinic, the workers suggest that she bring her husband in for the next appointment so that he can get tested and be part of the counselling and educational services that she will receive.
-
Reading: SRHR and HIV Integration (5 min)
Sexual and reproductive health rights (SRHR) and HIV integration refers to the delivery of HIV and reproductive health services within the same setting, during the same hours, and preferably under the same roof or as part of a facilitated referral within the same facility or to off-site facilities. Thus, clients receive both services in one visit.
For clients, integrated care has many benefits. As Nyasha mentioned, she appreciated that she was able to meet with two healthcare specialists in one place and at one time instead of scheduling multiple visits. Integrated care allows for seamless, smooth, and easy-to-navigate healthcare similar to what Nyasha experienced. It also minimizes the number of stages in an appointment and the number of separate visits required to a health facility. In addition, it shows clients that health workers are concerned about their whole health rather than just one clinical aspect. It also shows clients that health workers from different levels and services are working as a team to care for their health. In short, integrated care provides clients with continuity of care.
For providers, integrated care means that separate technical services and their management support systems are provided, managed, financed, and evaluated either together or in a closely coordinated way.
-
Reading: SRHR and HIV Services (5 min)
Now, let's take a look at the types of HIV and SRHR services that can be integrated. As you have been learning throughout this training, HIV services include services related to prevention, treatment, care, and support. Tap on each tab to read more.
Prevention
Prevention services are targeted to PLHIV as well as to HIV-negative individuals. They focus on HIV testing and counseling, prevention of mother-to-child transmission, and social and behaviour change. Services include condom promotion and distribution, voluntary medical male circumcision, post-exposure prophylaxis, and education about blood safety, injection safety, and infection prevention in clinical settings (covered in session 1).
Treatment
Treatment services include establishing and monitoring ART regimens as well as preventing and managing opportunistic infections (OIs) and HIV complications (covered in sessions 8 through 11).
Care and support
Care and support services include home-based care, psychosocial support, and preventing and managing sexually transmitted infections and reproductive tract infections (covered in sesson 13).
SRHR services include a wide range of services such as providing family planning counselling, offering counselling and health services to pregnant women, educating adolescents about sexual and reproductive health, and preventing sexual and gender-based violence.
The Safe Motherhood Initiative, in particular, is a SRHR service that focuses on improving the health and well-being of mothers and newborns. It includes family planning education, antenatal and postnatal care counselling and services, safe assisted delivery, and newborn care.
Additional SRHR services include:
- Preventing unsafe abortions and providing post-abortion care.
- Screening and management of cancers of the reproductive tract such as cervical, breast, and prostate cancers.
- Preventing and managing subfertility and infertility.
- Addressing SRHR needs of men and promotion of male involvement in SRHR.
-
Reading: Integration at Different Levels of Care (5 min)
Remember, a key feature of integrated services is that during one session or single visit a client receives both HIV and SRHR services. As the picture below demonstrates, this means that a client can receive family planning (fp), ART, and HIV treatment and counselling services (HTC) in a way that appears to the client as one integrated experience.
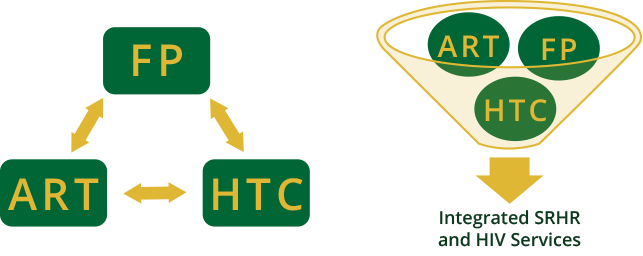
Another important feature is that there is a bi-directionality between the two types of services.
As the image below demonstrates, a healthcare provider seeing a client for HIV treatment and counselling may refer the client for family planning. Or, it is just as likely that a healthcare worker seeing a client for family planning may refer a client for HIV treatment and counselling. The services are bi-directional, or they go both ways.
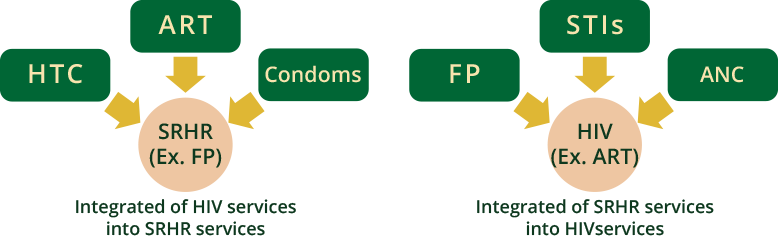
SRHR and HIV integration may look different depending on where the services are delivered. Tap each tab to read more.
- Community level
- Maternal child health or family planning clinic
- HIV testing and counselling (HTC) centres
- Comprehensive care centres
Community level
At a community level, integrated services could consist of a combined session on condoms and family planning methods. Or, they could contain an information, education, and communication (IEC) session focusing on preventing, treating, and caring for HIV that also addresses issues related to family planning.
Maternal child health or family planning clinic
Integrated care at a maternal child health or family planning clinic could include a combination of HIV testing and counselling with antenatal or postpartum care. It could also be the combination of STI screening services and ARV prophylaxis education.
HIV testing and counselling (HTC) centres
Integrated care at a HIV testing and counselling centre could be a combination of HIV testing and counselling and family planning services.
Comprehensive care centres
Integrated care at a comprehensive care centre could include TB screening combined with ART counselling, treatment, and care. It could also be the integration of ART counselling, treatment, and care integrated with family planning services.
-
Activity: SRHR and HIV Integration (10 min)
For each of the following clients, list 1-2 examples of how SRHR and HIV services could be integrated. Tap the compare answer button to compare your answer to an expert’s.
-
Reading: Programming and Policy Levels (5 min)
Having a linked response to SRHR and HIV issues is beneficial not only on a service level, but also on programming and policy levels. There is a growing body of evidence that suggests that better linking of HIV and SRHR efforts produces mutually reinforcing progress in both areas, given that the majority of HIV infections are sexually transmitted or associated with pregnancy, childbirth, and breastfeeding. Likewise, the risk of HIV transmission and acquisition can be further increased due to the presence of certain STIs. In addition, sexual and reproductive ill-health and HIV share root causes, including poverty, limited access to appropriate information, gender inequalities including gender-based violence, cultural norms, and social marginalisation of the most vulnerable populations. Moreover, many management and procurement issues are the same for SRH and HIV-related interventions.
A combination of better maternal and child health, reproductive health, and HIV services on the one hand, with structural measures to create a more enabling environment and greater demand for these services on the other, is required to bring about lasting changes to these long-standing problems. Linkages between core HIV services and SRH services in national programmes are thought to generate important public health benefits.
-
Reading: Minimum Package of Services (10 min)
To help with the integration of SRHR and HIV services on a large scale and to standardise what is offered, the Ministry of Health and Child Care developed a minimum package of services that outlines priority elements of integrated SRHR and HIV services for different levels of care. Tap on the following levels to read more.
Community level
Community based health care providers include village health workers (VHs), community based distributors (CBDs), HIV- and AIDS-related service providers, as well as other specific health service providers, such as secondary caregivers and behavioural change facilitators. These various groups predominantly provide health promotion services, and some preventive services at the household level. Some provide limited curative services for minor ailments.
The basic assumption at this level of care is that all providers are expected to provide integrated SRHR and HIV services and information to clients and community at all times. Messages on HIV need to include information on SRHR, and vice versa.
Rural and urban clinics
Rural and urban clinics are usually run by a very small staff consisting of one or two nurses. For this reason, all health services are provided using a one-stop or supermarket approach. This approach naturally integrates SRHR and HIV services in the overall health delivery system. As services are already integrated, for the sake of standardisation, minimum packages are proposed based on client’s reason for visit-index service.
Sexual and reproductive health services being provided in rural and urban clinics include:
- Family planning information, counselling, and services
- ANC
- Labour and safe delivery
- Newborn care
- PNC
- Prevention and management of STIs/RTIs, including HIV and AIDS
- Information and screening or referral for screening and management of cancers of the reproductive system such as cervical, breast, and prostate cancers
- Addressing SRHR needs of men and promotion of male involvement in SRHR
The HIV services provided at rural and urban clinics include:
- HIV counselling and testing
- Prevention of mother-to-child transmission (PMTCT)—(covered in session 12)
- HIV prevention information and education
- Condom promotion and distribution
- Injection safety and infection prevention
- TB screening and management (covered in session 9)
- Psychosocial support
Rural hospital
Just as with rural and urban clinics, health services in rural hospitals are provided using a one-stop, or supermarket approach. SRHR and HIV services are integrated in the overall health delivery system. Services are presented in an unpacked form, assuming that clients usually visit facilities seeking help for a specific SRHR or HIV-related care. The reason for the visit is taken as an entry point for other SRHR and HIV services and information provision.
Sexual and reproductive health services being provided in rural hospitals include:
- Family planning information, counselling, and services
- ANC
- Safe delivery
- Newborn care
- PNC
- Prevention and management of STIs/RTIs
- Information and referral for screening and management of cancers of the reproductive tract (cervical, breast, and prostate cancers)
- Adolescent sexual and reproductive health at a separate youth corner
- Promoting SRHR needs of men and male involvement in SRHR
Rural hospitals have diagnostic facilities, which allow them to perform HIV rapid tests and syphilis screening tests, as well as test CD4 counts and hemoglobin. Additional HIV services provided at rural hospitals include:
- HIV counselling and testing
- Prevention of mother-to-child transmission (PMTCT)
- HIV prevention information and education
- Condom promotion and distribution
- Injection safety and infection prevention
- OI management
- ART initiation as outreach site for district hospital
- TB screening and management
- Psychosocial support
Secondary, tertiary, and referral levels
At these levels of health care, SRHR and HIV services are mainly provided by different providers. The provincial (tertiary) and referral hospitals also manage complicated SRHR and HIV-related cases referred from district hospitals.
The following SRHR services are provided at these levels:
- Family planning information, counselling, and services
- ANC
- Safe delivery
- Newborn care
- PNC
- Adolescent sexual and reproductive health
- Prevention of unsafe abortion, and post-abortion care
- Prevention and management of STIs/RTIs
- Screening and management of cancers of the reproductive tract (cervical, breast, and prostate cancers)
- Treatment and management of subfertility
- Comprehensive post-rape care
- Promotion of SRHR needs of men and male involvement in SRHR
Rural hospitals have diagnostic facilities, which allow them to perform HIV rapid tests and syphilis screening tests, as well as test CD4 counts and hemoglobin. Additional HIV services provided at rural hospitals include:
- HIV counselling and testing
- Prevention of mother-to-child transmission (PMTCT)
- HIV prevention information and education
- Condom promotion and distribution
- Injection safety and infection prevention
- Blood safety
- OI/ART for both pediatric and adult cases
- TB screening and management
- Psychosocial support
-
Reading: Family Planning (15 min)
Nyasha has continued to come to the clinic regularly for prenatal care and counselling and treatment related to her HIV and ART regimen. During her most recent visit to the clinic, the healthcare worker asked her if she would like to discuss family planning. The worker explained that even though Nyasha is currently pregnant, learning about family planning methods now would give her time to think about her options, make an informed decision, and be prepared after she had her baby. That evening Nyasha spoke to her husband and he agreed to attend a family planning session with her during the next visit
Family Planning
Providing treatment, counseling, and monitoring care to PLHIV clients is an ideal time to integrate family planning services. As the healthcare worker explained to Nyasha, family planning counselling promotes informed decision making. By offering clients like Nyasha information about family planning during antenatal care, they will have time to consider their options, discuss with their partners, family, or friends, and be prepared to use their method of choice during the postpartum period.
Short-Term Family Planning
When talking to PLHIV clients about family planning, let them know that there are many options available to them. The resources section has more information on family planning. Tap on each contraception method to learn more.
Oral contraceptive pills
How to use Effectiveness (pregnancies per 100 women) Common side effects Consideration for PLHIV Take a pill every day. Highly effective when used correctly (less than 1 pregnancy/year). Menstrual changes, spotting, headaches, nausea. HIV-positive women, including those on ART, should use pills in combination with condoms to protect against pregnancy and STIs (dual protection). ART considerations:
If a woman is taking rifampicin or rifabutin, she should not rely on pills as her only method of contraception, as these drugs can reduce the effectiveness of combined and progestogen only pills. If she doesn’t want another contraceptive method, she should be encouraged to use condoms along with pills for extra protection against pregnancy.
Ritonavir or ritonavir boosted protease inhibitors may also reduce the effectiveness of pills. If the client does not want another method, she should be encouraged to use condoms along with either pills for extra protection against pregnancy.
Injectables
How to use Effectiveness (pregnancies per 100 women) Common side effects Consideration for PLHIV Get an injection every 3 months. Highly effective when used correctly ( less than 1 pregnancy/year). Spotting initially, then amenorrhoea; weight gain. HIV-positive women, including those on ART, should use pills in combination with condoms to protect. ART considerations:
If a woman is taking rifampicin or rifabutin, she should not rely on pills as her only method of contraception, as these drugs can reduce the effectiveness of combined and progestogen-only pills. If she doesn’t want another contraceptive method, she should be encouraged to use condoms along with pills for extra protection against pregnancy.
Ritonavir or ritonavir boosted protease inhibitors may also reduce the effectiveness of monthly injectables. If the client does not want another method, she should be encouraged to use condoms along with either pill for extra protection against pregnancy. A woman taking ritonavir can use progestogen-only injectables or a long-term family planning method.
Emergency contraception pills
How to use Effectiveness (pregnancies per 100 women) Common side effects Consideration for PLHIV Take within 5 days after condom breakage/other unprotected sex. Reduces chances of pregnancy from that one act of unprotected sex to 1/4 or 1/8 of chances if not used. Nausea Not as effective as other methods for regular use. Spermicides
Spermicides, or diaphragms or caps with spermicide, should not be used by women living with HIV and AIDS.
Long-Term Family Planning
You can also let clients know about long-term family planning methods that are available to them. These methods can safely be used by women with HIV. What distinguished long-term methods from short-term methods is that the former requires a procedure to be performed by a healthcare worker. The benefit to using long-term methods is that they provide long-term highly effective contraception (less than 1 pregnancy per 100 women per year). Tap on the following methods to learn more.
Implant
There is no contraindication for the use of hormonal implants in HIV-infected women, and should be considered for women requiring medium-term to long-term contraception. Examples include Norplant, Jadelle, and Implanon.
IUCD
An IUCD (copper-T) should not be inserted in a woman with gonorrhoea or chlamydia, or if a woman is at high individual risk of these infections. Women with HIV, or successfully treated advanced HIV disease, can have an IUCD inserted even within 24 hours post-delivery.
Vasectomy
A vasectomy provides a permanent method for couples who know they will not want more children. Clients should use this method in combination with condoms for dual protection.
Tubal Ligation
Tubal ligation is a permanent method for women that know they will not want more children. Clients should use this method in combination with condoms for dual protection.
-
Quiz: Knowledge Check (10 min)
-
Reading: Key Points (5 min)
- Linking SRHR and HIV services is important and can generate important public health benefits.
- SRHR services should include safe motherhood, family planning, screening and management of STIs and malignancies of the genital tract, sexual and gender-based violence care, and specialised services for men and adolescents.
- SRHR services can be provided from community level to hospital setting and are a key component of care for PLHIV.
