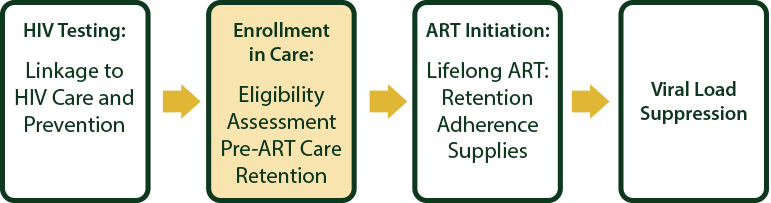
Session 7: Enrolment into Care
In this session, we will discuss the need for ART in all HIV-infected clients, the WHO HIV stages and ART eligibility criteria for adults, adolescents, and children.
Learning Objectives
By the end of this session, you will be able to:
- Understand principles of good chronic care.
- Clinically stage HIV-infected adults, adolescents and children using the WHO Staging system.
- Understand the TREAT ALL concept.
- Describe clinical criteria for when to start ART in infants and young children.
- Determine the WHO HIV clinical staging for children.
- Determine immunological criteria for when to start ART in infants and young children.
Learning Activities
-
Introduction to Enrolment into Care (5 min)
In this session, we will discuss the need for ART in all HIV-infected clients, the WHO HIV stages and ART eligibility criteria for adults, adolescents, and children.
Principles of Good Chronic Care
Good chronic care implies that clients must understand and learn to manage their own chronic condition. The HIV infection and slow progression to AIDS requires a considerable amount of education and support, in particular to give clients the skills they need to manage their own condition. Good HIV “self-management” is widely recognized as the key to achieving long-term treatment success.

Although the clinical team and others at home and in the community can help, clients need to learn to cope with the illness, open up to those they trust in order to get further help, practice prevention and positive living, and understand the importance of strict adherence to HIV treatment regimens.
The following principles can be used in managing many chronic and risk conditions:
- Understand principles of good chronic care.
- Clinically stage HIV-infected adults, adolescents and children using the WHO Staging system.
- Understand the TREAT ALL concept.
- Describe clinical criteria for when to start ART in infants and young children.
- Determine the WHO HIV clinical staging for children.
- Determine immunological criteria for when to start ART in infants and young children.
The 5A's
Let’s take a closer look at the 5 A’s you should use at every patient consultation.Tap each tab below to learn more.
Assess the client
Most health care workers are familiar with the process of assessing the client’s symptoms and signs, classifying (or diagnosing) the illness, and deciding what treatments to recommend.
● “What would you like to address today?” “What do you know about HIV/AIDS?” “Tell me about a typical day including your problem and what you are doing to manage it.” “To ensure we have the same understanding, could you tell me about the Treatment Plan in your own words?”, “Many people have trouble taking their medications regularly. What trouble are you having?”
Advise the client
This includes recommending treatments and educating and preparing the client for self-management. It is important to discuss the options the client has, not to just tell him or her what to do. It is also important to evaluate how ready the client is to adopt the treatment and to ask questions to make sure that he or she has understood. If your client is a child, you must educate, advise, and prepare his or her parents or caretaker instead.
● “I have some information about ________. Would you like to hear it?”, “What questions do you have about what I just told you?”
The client agrees
Agree means that the client understands, wants, and agrees to the treatment plan. This is a step we often skip! Agreeing is forming a partnership with the client and supporting his or her good self-management. In the case of young children in need of acute care, we try to tell them what is happening, but we often do not ask for their consent (and would still treat them even if they screamed, “No!”—which they often do). Therefore, you should agree with the parents or caretaker about the management of young children.
● “Among the options we’ve discussed, what would you like to do?”, Followed by: “Okay. So, as I understand it, we’ve agreed that you will _______. Is this correct?”
Assist the client
This includes treatments (through medication and other forms), advice, and counselling, but also includes help that you can provide the client in terms of skills to carry out the treatments or to overcome barriers. An important way to assist the client is to get other help, by linking him or her to available support in the community, peer support groups, or someone else to help support him/her during the treatment. Clients often require skilled support if they choose to disclose their HIV status to partners, family, friends, employer, etc. Most parents might find it difficult to communicate with their child on chronic care. They too often require support and skill to communicate with the child about his/her illness and the need to take medication regularly.
● “What problems might arise when you follow this plan?”, “How do you think you could handle that?”, “What questions do you have about the plan or how to follow it?”
Arranging a follow-up
This step involves defining a follow-up visit, scheduling an appointment, arranging how the medication can be picked up on the next visit, and recording what happened on the current visit. HIV is often a family illness. When one family member is HIV-positive, other family members are affected and some may already be infected by the virus as well.
If need be, arrange family-focused care to take place on the same date and at the same clinic for the whole family. Similarly, arrange and coordinate care with other services when clients require linkage to other services within the same facility or referral to another facility.
-
WHO Clinical Stages of HIV (5 min)
The World Health Organization (WHO) has developed case definitions for HIV surveillance and clinical staging and immunological classification of HIV-related disease in adults and children. This staging system is important because it uses standardized clinical parameters to direct medical decision making for patients with HIV/AIDS. It helps to determine the prognosis, strengthens the diagnosis when laboratory testing is unavailable or delayed, and guides decisions regarding the initiation, success, or failure of ART..
This screening strategy allows for efficient identification of early infection and aggressive management and is therefore a useful tool for health care workers for improving access to and implementation of care
The WHO staging system is based on the clinical status as well the past medical history. It is important to note that the accuracy may be limited if the past medical history is unavailable. A good clinical examination is essential for accurate staging, and staging should be conducted at every clinical visit in order to identify disease progression or treatment failure.
Four Clinical Stages
The WHO system for adults sorts patients into one of four hierarchical clinical stages. Patients are assigned to a particular stage when they demonstrate at least one clinical condition in that stage’s criteria. Patients remain at a higher stage after they recover from the clinical condition which placed them in that stage. Tap on each stage to read about it.
SourceStage 1: Asymptomatic
- Asymptomatic
- Persistent generalized lymphadenopathy
Stage 2: Mild Symptoms
- Moderate unexplained weight loss (10% presumed or measured body weight)
- Recurrent upper respiratory tract infections (sinusitis, bronchitis, otitis media, pharyngitis)
- Herpes zoster
- Anglar cheilitis
- Recurrent oral ulcerations
- Papular pruritic eruptions
- Seborrhoeic dermatitis
- Fungal nail infections
Stage 3: Moderate Severity
- Unexplained severe weight loss (>10% of presumed or measured body weight)
- Unexplained chronic diarrhoea for longer than one month
- Unexplained persistent fever (intermittent or constant, for longer than one month)
- Persistent oral candidiasis
- Oral hairy leukoplakia
- Pulmonary tuberculosis (current or within the last 2 years)
- TB Adenitis
- Severe bacterial infections (such as pneumonia, empyema, pyomyositis, bone or joint infection, meningitis or bacteraemia)
- Acute necrotizing ulcerative stomatitis, gingivitis or periodontitis
- Unexplained anaemia (<8 g/dL), neutropaenia (<1,000/mm³) and/or chronic thrombocytopaenia (<50,000/mm³) for more than 1 month.
Stage 4: Severe
- HIV wasting syndrome
- Pneumocystis pneumonia
- Recurrent bacterial pneumonia
- Chronic herpes simplex infection (orolabial, genital, or anorectal of more than 1 month’s duration) or visceral at any site
- Oesophageal candidiasis (or candida of trachea, bronchi, or lungs
- Extrapulmonary TB
- Kaposi’s sarcoma
- Central nervous system toxoplasmosis
- HIV encephalogpathy
- Extrapulmonary cryptococcosis, including meningitis
- Disseminated nontuberculous mycobacteria infection
- Progressive multifocal leukoencephalopathy
- Chronic cryptosporidiosis
- Chronic isosporiasis
- Cytomegalovirus (CMV) infection (retinitis, or CMV infection affecting another organ)
- Disseminated mycosis (e.g., extrapulmonary histoplasmosis, coccidiomycosis)
- Recurrent septicaemia (including nontyphoidal salmonella)
- Lymphoma (cerebral or B-cell non-Hodgkin’s)
- Invasive cervical carcinoma
- Atypical disseminated leishmaniasis
- Symptomatic HIV-associated nephropathy or HIV-associated cardiomyopathy
Guidelines for Antiretroviral Therapy for the Prevention and Treatment of HIV in Zimbabwe. Adapted from WHO, WHO Case Definitions of HIV for Surveillance and Revised Clinical Staging and Immunological Classification of HIV-Related Disease in Adults and Children, 2007. -
ART Eligibility in Adults and Adolescents (5 min)
Now that you have learned the clinical stages of HIV-infected adolescents and adults based on the WHO staging system, let’s take a look at when you would start antiretroviral therapy (ART) in adults and adolescents.
As of June 2016, close to 80 low and middle-income countries have adopted the “TREAT ALL” policies outlined in the Consolidated Guidelines On The Use of Antiretroviral Drugs For Treating And Preventing HIV Infection. The guidelines contain key recommendations to “treat all” people living with HIV, including children, adolescents, adults, pregnant and breastfeeding women, and people with coinfections. The recommendations aim to improve the quality of HIV treatment and to bring us closer to the universal health coverage ideals of integrated services, community-centred and community-led health care approaches, and shared responsibility for effective programme delivery.
Seven Requirements to Initiate ART
Requirement 1: HIV-positive client holding written documentation (of positive test result)
If the client has had a positive HIV test at another facility, but does not have written documentation, the test should be repeated. Clients should not start ART if there is only a clinical suspicion of HIV infection.Requirement 2: Verify HIV test result
All patients starting ART should have a repeat confirmatory HIV test done using the same testing algorithm, preferably by a different tester on the day of ART initiation.Requirement 3: Client fits the criteria to be started on ART at a first-level facility
This means that the patient has no severe disease, no stage 4 disease, no active TB, no anemia, no jaundice, no diabetes or liver disease, is not a drug abuser, and has not taken ARVs before.Requirement 4: All opportunistic infections have been treated or stabilized
Requirement 5: The client is ready for ARV therapy
This is the most important and difficult requirement. Preparation for ART and assessment of the client’s readiness to start ART is necessary. ARV treatment is rarely an emergency. It is essential for adherence that a partnership be formed with the client whereby he or she is responsible for taking ARV drugs regularly. It will almost always take several visits to arrive at this readiness. When the client is ready, ART should be discussed at a clinical team meeting. If the decision is that the client is both eligible and ready, put the date in the upper-right corner of the HIV care/ART card.Requirement 6: Supportive clinical team prepared for chronic care
People living with HIV require good chronic care and long-term follow-up.Requirement 7: Reliable drug supply
Starting ART for just a short period of time does not make any sense as the virus remains in the body forever. Continuous high blood levels of antiretroviral drugs are needed to stop the virus from making new copies of itself.
Interrupting ART because drugs are out of stock is not acceptable since it can create resistance. A virus that is resistant will not be sensitive to the drugs anymore, and the client will become sick again or die from new OIs. In addition, clients who are resistant may spread the resistant virus to others. These newly infected people will also be resistant to the ARV drugs (and thus not get better with treatment), even if they have not been on ART before. If one drug is out of stock, all drugs must be stopped at the same time.
Clients with CD4 cell count below 100 should be fast-tracked for treatment initiation. Clients should be screened for symptomatic TB and cryptococcal disease, receive cotrimoxazole and INH prophylaxis like all other clients, and be closely monitored for three months, as this is their highest risk period for contracting bacterial infections and TB or cryptococcal IRIS.
As a health care worker, you should educate clients and their families to report immediately to a health facility if they are unwell whilst their CD4 is <100.
-
Kuda (5 min)

Kuda just completed antibiotic course for treating an infection in his lungs. At discharge the doctor tests for HIV. The results are positive. Kuda’s CD4 cell count is 664 and he has no other medical complaints. He admits that three months ago, he was treated for ‘white things’ in his mouth and throat. He had difficulty swallowing but the medication they gave him worked in about a week.
-
Shona (5 min)

Shona is a 47-year-old man who tested HIV positive two years ago. He’s a heavy drinker and does not come to the clinic regularly. Since his wife died two years ago, Shona stays home alone and has not disclosed his status to anyone. He has a sexual partner and occasionally uses condoms with her. His CD4 count is 89.
-
Tendai and Mary (10 min)

Tendai and Mary have been married five years and have one child. Mary is five months pregnant and is offered an HIV test as part of her routine antenatal care. Mary’s test results are negative. The clinic nurse advised that Tendai be tested as well. Unfortunately, Tendai’s test is positive. Both Tendai and Mary report that they are healthy and have not been sick with any serious illnesses. They occasionally have colds usually passed on by their child.
When you examine Tendai you find a few lymph nodes in the axilla and cervical region. Tendai’s CD4 count is 549.
-
Knowledge Check (10 min)
-
ART Eligibility in Children (5 min)
All children confirmed to be HIV-infected should be initiated on ART regardless of the CD4 count or WHO clinical stage. Priority should be given to less than two years old and with those with CD4 count below 350.
Presumptive diagnosis in children below 18 months of age

ART should be initiated in any child under the age of 18 months who has been given a presumptive clinical diagnosis of HIV infection. The presumptive diagnosis of HIV involves the following steps:
1. Any infant or child under the age of 18 months with signs and symptoms suggestive of HIV infection should have an HIV antibody test. These signs and symptoms include oral thrush, severe pneumonia, severe sepsis or any other AIDS-defining condition. Other factors include advanced immune suppression (CD4 <20% or recent maternal death).
2. If the antibody test is positive, a presumptive clinical diagnosis of severe HIV-infection should be made, and ART started as soon as possible.
3. Confirm the diagnosis of HIV infection as soon as possible with an HIV DNA PCR test.
Clinical criteria for when to start ART in infants and young children
Many HIV-infected children develop severe HIV-related signs and symptoms in the first year of life, while others remain asymptomatic or mildly symptomatic for more than a year and may survive for several years. The clinical expression of HIV in young children is highly variable; therefore, it is important to understand how HIV can present in children.
The conditions listed below provide guidance in the clinical diagnosis of HIV infection in children. Tap on each tab to view the signs/conditions.
- Recurrent infection: Three or more severe episodes of infection (such as pneumonia, meningitis, sepsis, cellulitis) in the past 12 months.
- Oral thrush: Erythema and white-beige pseudomembranous plaques on the palate, gums, and buccal mucosa. After the neonatal period, the presence of oral thrush is highly suggestive of HIV infection in the following situations:
- Presenting for more than 30 days, despite treatment or recurrent oral thrush
- Extending beyond the tongue
- Presenting as oesophageal candidiasis
- Chronic parotitis: Unilateral or bilateral parotid swelling for more than 14 days, with or without associated pain or fever.
- Generalized lymphadenopathy: Enlarged lymph nodes in two or more extra-inguinal regions without any apparent underlying cause.
- Hepatomegaly with no apparent cause: In the absence of concurrent viral infections, such as cytomegalovirus (CMV).
- Persistent and/or recurrent fever: Fever (>38°C) lasting more than seven days or occurring more than once over a period of seven days.
- Neurological dysfunction: Progressive neurological impairment, microcephaly, delay in achieving developmental milestones, hypertonia, or mental confusion.
- Herpes zoster (shingles): Painful rash with blisters confined to one dermatome on one side.
- Skin rashes: Typical skin rashes include extensive fungal infections of the skin, nails and scalp, molluscum contagiosum, flat warts, erythematous papular rash.
- Chronic suppurative lung disease.
- Pneumocystis pneumonia (PCP)
- Oesophageal candidiasis
- Lymphoid interstitial pneumonitis (LIP)
- Kaposi’s sarcoma
- In girls, acquired recto-vaginal fistula
- Chronic otitis media: Ear discharge lasting more than 14 days.
- Persistent diarrhoea: Diarrhoea lasting more than 14 days.
- Moderate or severe malnutrition: Weight loss, or a gradual but steady deterioration in weight gain from expected growth, as indicated on the child’s growth card.
- Newborn: suspect HIV infection in breastfed infants under the age of six months who fail to thrive.
-
WHO Clinical Staging for Children (5 min)
The WHO has developed a four-stage system intended for use in children with established HIV-infection, where each stage indicates the degree of immune suppression. Tap on each stage to learn about the WHO staging criteria for children.
SourcePrimary HIV Infection
- Asymptomatic
- Acute retroviral syndrome
Stage 1: Asymptomatic
- Asymptomatic
- Persistent generalized lymphadenopathy
Stage 2: Mild Symptoms
- Unexplained persistent hepatosplenomegaly
- Papular pruritic eruptions
- Extensive wart virus infection
- Extensive molluscum contagiosum
- Recurrent oral ulcerations
- Unexplained persistent parotid enlargement
- Lineal gingival erythema
- Herpes zoster
- Recurrent or chronic upper respiratory tract infections (otitis media, otorrhoea, sinusitis, tonsillitis)
- Fungal nail infections
Stage 3: Moderate Severity
- Moderate unexplained malnutrition not adequately responding to standard therapy
- Unexplained persistent diarrhoea (14 days or more)
- Unexplained persistent fever (above 37.5°C intermittent or constant, for longer than 1 month)
- Persistent oral candida (outside first 6 to 8 weeks of life)
- Oral hairy leukoplakia
- Acute necrotizing ulcerative gingivitis/periodontitis
- Lymph node TB
- Pulmonary TB
- Severe recurrent presumed bacterial pneumonia
- Symptomatic lymphoid interstitial pneumonitis
- Chronic HIV-associated lung disease, including bronchiectasis
- Unexplained anaemia (<8 g/dL), neutropenia (<500/mm³), or chronic thrombocytopenia (<50,000/mm³)
- HIV-associated cardiomyopathy or HIV-associated nephropathy
Stage 4: Severe
- Unexplained severe wasting, stunting, or severe malnutrition or not responding to standard therapy Pneumocystis pneumonia
- Recurrent severe presumed bacterial infections (e.g., empyema, pyomyositis, bone or joint infection, or meningitis, but excluding pneumonia)
- Chronic herpes simplex infection (orolabial, or cutaneous of more than one month’s duration or visceral at any site)
- Extrapulmonary TB
- Kaposi’s sarcoma
- Oesophageal candidiasis (or candida of trachea, bronchi, or lungs)
- Central nervous system toxoplasmosis (outside the neonatal period)
- HIV encephalogpathy
- Cytomegalovirus (CMV) infection; retinitis or CMV infection affecting another organ, with onset at age over one month
- Extrapulmonary cryptococcosis, including meningitis
- Disseminated endemic mycosis (extrapulmonary histoplasmosis, coccidiomycosis, penicilliosis)
- Chronic cryptosporidiosis
- Chronic isosporiasis
- Disseminated nontuberculous mycobacteria infection
- Acquired HIV-associated rectal fistula
- Cerebral or B-cell non-Hodgkin’s lymphoma
- Progressive multifocal leukoencephalopathy
It was adapted from WHO, WHO Case Definitions of HIV for Surveillance and Revised Clinical Staging and Immunological Classification of HIVRelated Disease in Adults and Children, 2007..

Immunological Staging in Infants and Young Children
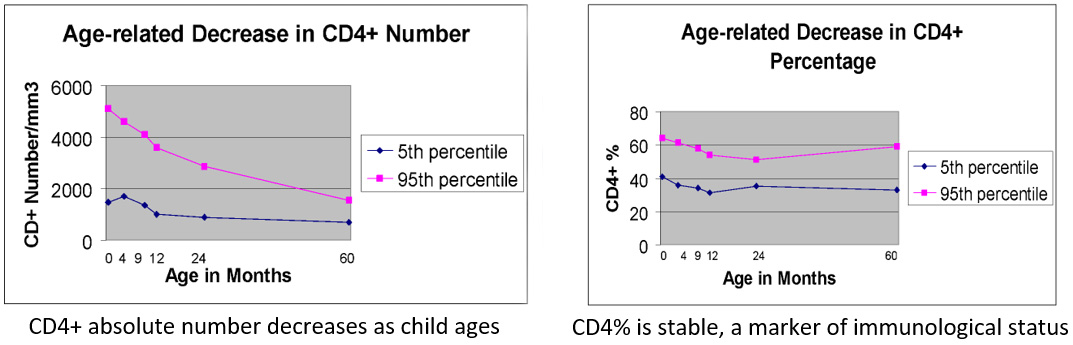
Immunological staging for adults cannot be used to assess immune suppression in infants and young children.
Children generally have greater thymic function and a greater proportion of circulating CD4 cells than adults, which gradually decline to adult levels by about six years of age. In contrast, the percent of lymphocytes that are CD4-positive among normal children is not age related. Thus, the levels of CD4 count that identify stages of immune suppression vary with age; the levels of CD4 percent do not.
Absolute CD4 Count vs. CD4 Percentage
CD4 count identifies risk of the development of OIs and can be used in children above five years of age. CD4 percentage is a more stable measurement in children for monitoring treatment success and is preferred for children under five years. The CD4 percentage can be found by multiplying the absolute CD4 count by 100 and dividing by the total number of lympohocyte count.
The graphs below show the difference in CD4 count vs. CD4 percentage.
When Is CD4 Measurement Necessary?
CD4 measurement in children below the age of five years is NOT essential for ART eligibility assessment as all these children must be commenced on ART. CD4 measurement is essential however for monitoring response to treatment.
-
Knowledge Check (10 min)
-
Key Points (5 min)
- Treat all HIV positive clients regardless of CD4 count and WHO clinical stage.
- Priority for ART initiation should be given to clients with CD4<350 cells/mm³.
- Clients with CD4<100 cells/mm³ should be carefully screened for OI’s and closely monitored for three months.
- WHO staging is important for monitoring and initiation of cotrimoxazole (CTX).
- Presentation of HIV disease is highly variable in infants and young children.
- Initiate ART in all children under the age of 18 months of age with a presumptive HIV diagnosis.
- Initiate ART in all children who are confirmed to be HIV infected, regardless of WHO stage or CD4 count.
