-
Role Play: Frequently Asked Questions
[activity type]
Ask the mentee the following frequently asked questions that he or she may hear from several different clients. Remind mentee to answer in ‘client language,’ not medical terminology. After completing all questions, discuss what the mentee did well, what could be improved, and any questions the mentee has. Sample answers for each question are included below.
Ask the mentee:
How can I possibly remember to take medication every day for the rest of my life even when I am not feeling sick?
- It is important for you to decide what will be the best way for you to remember to take your medication. Here are some suggestions:
- Choose a regular activity that you do every day that will be linked to taking your medicine. For example, if you take your medication before bedtime put the bottle near your toothbrush or on a table near your bed. If your medication is taken in the morning and evening, put it in the kitchen where you will see it when you eat your breakfast.
- Use the alarm on your mobile phone as a reminder.
- Use a calendar to mark off that you have taken your medicine each day.
What is the purpose of taking lifelong treatment if I will not be cured?
- The medicines to treat HIV strengthen your immune system (your solider cells) that will lower the amount of HIV in your blood and keep you healthy for a very long time. We know that these medicines fight HIV and improve the health of those people that take them every day for life.
- If you are told you need to take the medications and decide not to take them, you will become sick and not able to work or care for yourself or your family.
- Research is working on a cure but until then, it is important for you to stay healthy and strong, and that can only be done if you take all of the medicines and follow-up in the clinic as directed by your healthcare worker.
What if I go away for a few days and I forget to take the medication with me?
- If you know you will be traveling, put a reminder in the calendar of your mobile phone that will alert you before you leave to bring your medicines.
- If you go away and realize you have forgotten your pills, try to get the medicines brought to you if possible by a family member or your treatment supporter.
- If that is not possible and you will be away from your home for an extended period of time, go to the nearest clinic and talk to the provider about your situation and the need for more medication. It may be necessary to contact your clinic so be sure to have your provider’s name and contact information with you at all times.
Since my wife is HIV positive and taking medicine, can I also start taking the same medication even if I have not yet been tested since she is my sexual partner?
- Even though you have been sexually active with your wife who is HIV positive it does not necessarily mean that you are HIV positive as well. There are many couples where one partner is negative and one is positive.
- Taking the HIV medicine your wife is taking when you are not HIV positive can be dangerous to your health. You would also be taking medicine that she needs to keep her healthy and she cannot miss any of her doses.
- The only way to tell if you are positive is to have an HIV test. If you are HIV negative, it will be important for you to stay negative by wearing a condom every time you have sexual intercourse. If you are not circumcised, I can talk to you about how that can also help lower the risk of becoming HIV positive.
- What am I going to feel like when I start taking this medicine? I’ve heard that some people have terrible dreams and “get high” from one of the medicines. Is that true?Some people may have colorful or unusual dreams the first few nights after taking one of the HIV medicines. These dreams can last up to a week but should lessen over time. The medicine can actually benefit people that have trouble sleeping.
- It is important that the medicine have 6-8 hours of “rest” or “sleep” time so if there are any side effects, they will not bother you since you will be asleep. Taking your medicines at night will prevent you from feeling “high” or dizzy, which can happen to some people.
- It is also very important that you do not drink alcohol or take any type of sleeping pills or herbs along with the medication. That will make any possible side effect worse.
- Remember that not everyone will experience these side effects and if they do occur, they will lessen after a short time. If they continue, come back to the clinic so I can examine you and change the medicine if needed.
What if other people can see that I am taking medicine?
- It is important that we talk about who you can and should tell about your HIV status and this will avoid you having to hide your medicine. This is especially important if you are living with family and do not have a secure place to keep your medicine.
- If you have not or will not disclose your status, you will have to tell your family that you are taking medicine for a health problem. Your relationship with them may be difficult since they will not understand why you are hiding information. They will worry that you have a serious or life-threatening illness or continually wonder why you are on medication. You have an opportunity to teach others about how the medication allows a person to live a long and healthy life.
- I can help you tell your family by having you practice with me. You can also bring your family member with you the next time and we can tell them together.
What if people see me when I come to get my medicine at the clinic?
- You do not have to say anything to a person you see in the clinic that you may know from your community. People in this clinic are here for a variety of reasons. The medicine that you are getting could be for many reasons.
Why is it important for me to tell at least one person that I am HIV-positive as you say?
- Disclosing to at least one person is important for many reasons:
- You can get the love and support you need to help you live with HIV disease
- You will not have to constantly “hide” your health problems
- You will reduce the chances of transmitting the virus to others
- You will have someone who you can talk to about your concerns or fears
What if I decide not to tell anyone about my HIV status? Why would I need anybody to support me when I can do it all on my own?
- If you feel you are adjusting to your diagnosis and can follow the instructions for your medicine and follow-up, then it is your decision not to tell anyone else.
- It is important though to talk to your healthcare provider if you have any questions or if you feel that you are becoming depressed or unable to take your medicine.
My wife does not have time to come to meet you since we have three children and one of them is sick. Can she still be my treatment supporter?
- Let’s try to schedule another time for her to come and talk with me but until then, make sure she knows about the medicine you are taking, the time it should be taken, and any possible side effects that I have discussed with you.
- Take the information about HIV and the medication and ask her to read it. If she has any questions, she can ask you or we can discuss it when she comes in the next time.
Why are you giving cotrimoxazole to my infant while she is healthy and you are not even sure she is HIV-infected?
- Infants born to women who are HIV positive are at risk for a serious lung infection that can be prevented by giving cotrimoxazole. Since it is not possible to know which HIV-exposed infants are HIV infected until they are older, the current Zimbabwe and World Health Organization guidelines recommend that all HIV-exposed infants begin taking cotrimoxazole at 6 weeks of age.
When my wife and I are both taking antiretroviral medication, is it necessary for us to use condoms when we have sex?
- YES! HIV reinfection or superinfection can develop as a result to unprotected sexual intercourse between two HIV positive persons. Even though you are both taking antiretroviral medication, you each may have a different strain of HIV or your virus may not be controlled by the medicine you are taking now. You will not know this and you can transmit this different or resistant virus to your partner. It is therefore very important that you practice safer sex by using a condom every time you have sexual intercourse.
- It is important for you to decide what will be the best way for you to remember to take your medication. Here are some suggestions:
-
Case study: ART Initiation Adult Man
[activity type]
Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in ART initiation.
Tendai and Mary have been married 5 years and have one child. Mary is 5 months pregnant and is offered HIV test as part of ANC. Her test results are negative. Tendai is tested too. Unfortunately his test is positive. Both Tendai and Mary report that they are healthy and have not been sick with any serious illnesses. They occasionally have colds usually passed on by their child.
When you examine Tendai you find a few enlarged lymph nodes in the axilla and cervical region. His CD4 cell count is 549.
-
In what WHO clinical stage is Tendai?
WHO clinical stage 1 -
Does Tendai qualify for ART according to Zimbabwe national guidelines? Why?
Yes. Tendai qualifies for ART according to the Zimbabwe guidelines because he is in a discordant relationship. -
What further advice would you give this couple?
- Adherence counselling that includes importance of not only ART adherence for Tendai but adherence to antenatal appointments for Mary to monitor her condition and that of their unborn baby.
- Correct and consistent use of condoms each time they have sex.
- HIV testing for their child.
- Retesting for Mary after 3 months to rule out the window period and also ensure that she has a valid test result when she delivers her baby.
- The need for Mary to offer psychological support to Tendai and remind him to always take his medication.
- Information on medication side effects and when to come back to the clinic.
- The importance of not missing clinic appointments.
-
In what WHO clinical stage is Tendai?
-
Case study: WHO Clinical Staging
[activity type]
Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in ART initiation.
Kuda just completed antibiotic course for treating an infection in his lungs. At discharge the doctor tests for HIV. The results are positive.
Kuda’s CD4 cell count is 664 and he has no other medical complaints. He admits that three months ago he was treated for “white things” in his mouth and throat. He had difficulty swallowing but the medication they gave him worked in about a week.
-
In what WHO clinical stage is Kuda?
WHO clinical stage 4 -
Does Kuda qualify for ART according to Zimbabwe national guidelines? Why?
Yes. He is Clinical Stage 4 due to a history of oesophageal candidiasis which qualifies him to begin ART. -
Why has Kuda been developing OIs at a high CD4 count?
This is only a single CD4 count and it is possible that Kuda’s CD4 count is lower. There can be fluctuations due to the transport of the blood, laboratory testing process, or timing of when the blood is drawn (morning vs. late afternoon). A CD4 count done when he was treated for oesophageal candidiasis could have been much lower.
-
In what WHO clinical stage is Kuda?
-
Case Study: Adult Man Heavy Drinker
[activity type]
Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in ART initiation.
Shona is a 47-year-old man who tested HIV + 2 years ago. He’s a heavy drinker and does not come to the clinic regularly. Since his wife died 2 years ago, Shona stays home alone and has not disclosed his status to anyone. He has a sexual partner and occasionally uses condoms with her.
His CD4 count is 89.
-
Is he eligible for ART? Why?
Yes. He is eligible for ART because he tested HIV+ 2 years ago and he has a CD4 count of 89. A thorough physical and psychosocial assessment is needed to exclude OIs such as TB and to assess how his current alcohol use will affect his adherence to care and treatment. -
How you would prepare him for ART commencement?
- Intensive readiness and psychosocial counselling and risk reduction focusing on his alcohol abuse.
- Counselling on correct and consistent use of condoms each time he has sex.
- Disclosure discussion and assistance in identifying a treatment supporter.
- Encouragement to refer his sexual partner for testing.
- Counselling on the importance of not missing clinic appointments and referral to support group if possible.
- Cotrimoxazole prophylaxis in view of the low CD4 count of 89 to prevent occurrence of opportunistic infections.
- Assessment to exclude TB before ART initiation.
- Adherence assessment can include whether or not he attends the counselling sessions, clinic appointments.
-
Is he eligible for ART? Why?
-
Role Play: Counselling and Education
[activity type]
Tell your mentee that you are going to engage in a role play to help him or her start a client on ART. He or she will play the role of health care provider, and you will be the client.
Show the mentee the instructions below for the health worker. Then, tap on the box for the client (mentor) instructions. Do not show this to the mentee.
The client in front of you is a 36-year-old man who was tested HIV+ one year ago. He just moved to this district because of his work. He tells you that before he moved, the doctor at his former health centre told him that he could start ART soon.-
Patient instructions (mentor). Do not show this to the mentee.
You are a 36-year-old man who tested HIV+ one year ago. You just moved to this district because of your work. Before you moved, you were told at your former health centre that you could start ART soon. You are worried because you have not told anybody at work that you are HIV positive. You do not want people at work to find out that you take medication for HIV. You have come to this health centre to make sure that this will not happen.
Questions to ask as the health care worker:
- “Do I have to wait a few months until I get used to my new job to start the medicine?”
- “Is it necessary for me to tell my boss or anyone I work with that I have HIV? If so, will I be fired from my job?”
- “What are the medicines for HIV and how frequently do I need to take them?”
- “If I have side effects from the medicines, will people know that the HIV medicines are what caused the side effects?”
- “If I start the medicines, will I still be able to work full time and in my current job?”
If you are asked, respond with the following answers:
- You tested HIV+ one year ago. You had oesophageal thrush 2 weeks ago.
- You think that you will be able to take the medicines as prescribed. In the past, you have been very good taking medicine for other problems and in showing up at the health centre for your follow-up appointments.
- You have not disclosed your status at work because you are afraid to lose your job.
- You are used to taking care of the little problems you have regarding your health.
- You live with your parents, who know you are HIV+ and are very supportive and help you in any way possible.
- Your father would be your treatment supporter.
- You have a girlfriend. She does not know you are HIV+, but you use condoms when having sex.
If there is a clinical review:
- You have no new symptoms.
- You take cotrimoxazole 960 mgs once daily.
- You used to weigh 69 kg before you had the thrush, but you lost a lot of weight at that time.
Results during the visit:
- Physical exam: Weight 60 kg. Rest of physical examination is normal.
- CD4 count: 280
-
Antiretroviral Therapy (ART): ART Initiation
Learning Objective:
- Prescribe the correct ARVs for the first line regimen
-
Assessment
Case study
Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in ART initiation.
Nancy is a 29-year-old woman, who started treatment for PTB 2 months ago (she was coughing, had lost weight, and her sputum was + AAFBs). The nurse told her she needed to start ART because she had TB. Nancy tested HIV+ last year and was diagnosed with PTB.
Nancy is a teacher but is not able to work due to continued fatigue. Her husband and 2 children have not been tested for HIV or TB. Nancy has not had a CD4 count yet and she is currently on TB treatment.
Nancy’s weight is 58 kg (prior to starting TB treatment she was 56 kg).
-
Does she need ART?
Yes, lifelong. -
Why?
Patients with TB/HIV require both TB and ART to cure the TB and control the HIV. -
Should she take her children for screening for TB? HIV?
Yes. Her children and husband must be screened for TB and HIV. If negative for both, IPT should be initiated. If HIV positive, follow the guidelines for initiation of ART and IPT. If there are any other family members who were in close contact with Nancy, they should be advised to have TB screening as well. -
When is CD4 testing done with a client co-infected with TB/HIV?
CD4 testing should have been done when TB treatment was started along with other baseline laboratory tests, such as liver function tests, full blood count, and urea and creatinine. -
What do you think about the timing of ART with Nancy? Could she have started sooner?
ART initiation should be started at least 2 weeks after the start of TB treatment and within 8 weeks once the client has stabilized on TB treatment.
-
Does she need ART?
-
Activities
-
Mentor Resources
-
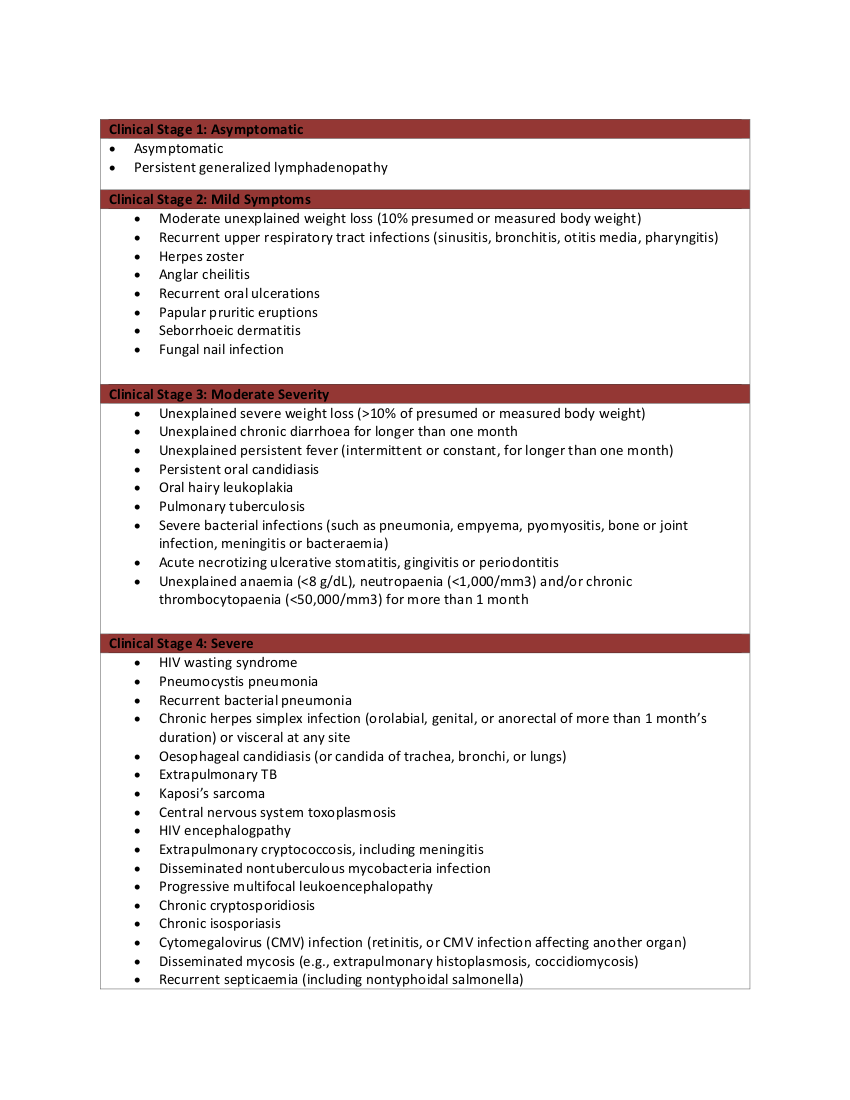
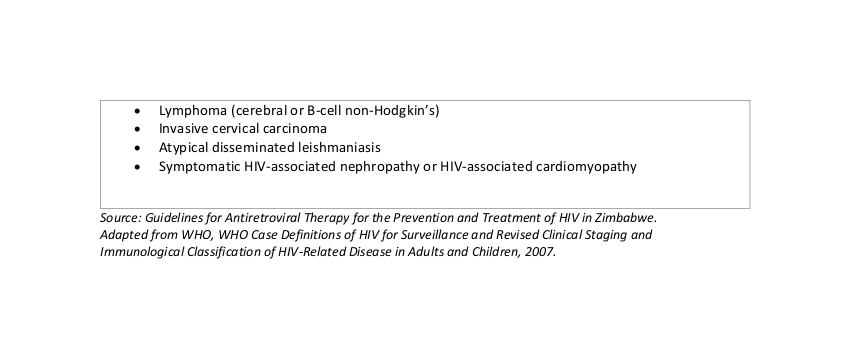
Revised WHO Clinical Staging of HIV/AIDS for Adults and Adolescents with Established HIV Infection
Revised WHO Clinical Staging of HIV/AIDS for Adults and Adolescents with Established HIV Infection
 ×
×
-