Discussion questions/quiz
Tell your mentee you would like to assess his or her knowledge related to ART monitoring with the following questions. The text in italics are answers and notes for the mentor.
-
Question 1
An HIV-positive client, Kuda, has been taking ART and coming to your clinic for a couple of years. According to the Zimbabwe guidelines, what type of monitoring should you be doing to assess whether or not his ART is working and how often is this monitoring done?
If the mentee describes any of these options, you could ask him/her the broader term for each area.- Clinical monitoring (clinical improvement)
Clinical monitoring is done at every visit. If he is maintaining > 95% adherence his visits can be every 3 months. - Immunological monitoring (CD4 count)
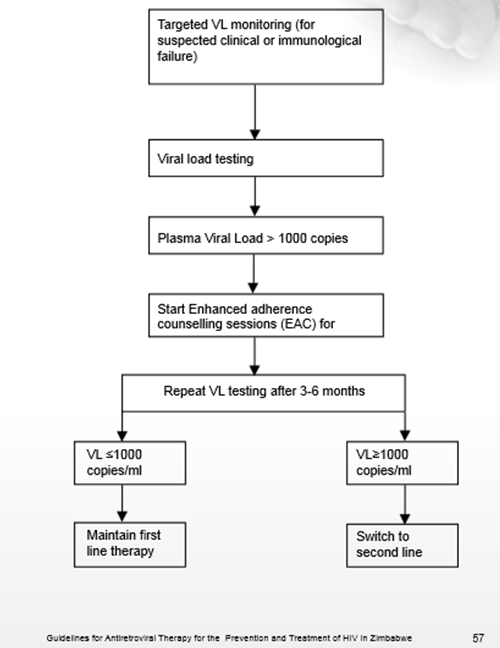
CD4 count should be done at six-monthly intervals. - Virological monitoring (HIV viral load)
Due to limited resources, Zimbabwe conducts targeted viral load testing for suspected clinical or immunological failure. This is primarily done by the medical officers.
- Clinical monitoring (clinical improvement)
-
Question 2
What specifically would you look at when doing clinical monitoring for Kuda?
[note text]Ask whether he:- Feels better.
- Is gaining weight.
- Is seeing an improvement in symptoms and signs of the original presenting illness.
When the number of CD4s increases, the body's defence will improve. If the body's defence works better, fewer OIs should occur. That is why looking at the clinical status of the client (evaluating the occurrence of OIs) is a good way of evaluating if the therapy is effective. -
Question 3
How often do you monitor Kuda’s CD4 count?
[note text]Every 6 months
-
Question 4
Kuda is frustrated that his CD4 count is improving so slowly. What would you tell him?
[note text]The time it takes to see the number of CD4 cells increase varies from person to person. The number of CD4 may rise by between 100 and 200 in the first year if you have never taken ART before and are taking the drugs with an adherence rate of 95% or more. It depends a lot on where you start: sometimes a lower CD4 when you start ART means it will take longer before the CD4 rises substantially.
-
Question 5
What would you do if Kuda’s CD4 count persistently declines?
[note text]Persistently declining CD4 counts, as measured on two occasions, at least three to six months apart and a clinical deterioration indicate that he may be experiencing treatment failure. Consult with your clinical mentor or HO or refer to a higher-level facility.
-
Question 6
What are some ways you can monitor a client’s antiretroviral intake?
[note text]- Pill count
- Pharmacy refill tracking
- Client self-reporting although the client may not admit to missed doses
-
Question 7
Kuda wonders what successful treatment looks like. What do you say in response?
[note text]If therapy reaches its goal (success), the client’s weight should increase and no new OIs would occur. We say a client has treatment failure when a new opportunistic infection develops, or prior opportunistic infections relapse, or symptoms do not disappear over time. Successful treatment is also when the CD4 count rises from baseline and either continues to rise or maintains a consistent level.