-
Quiz
[activity type]
Ask the mentee what course of action he or she would take for the following side effects.
Early side effects
-
Headache
Mild – Paracetamol 1g 6 hourly OR Ibuprofen 400mg 8 hourly with food. -
Nausea
Take medication with or immediately following a meal. Avoid spicy foods, citrus, coffee. -
Vomiting
Bland diet, small frequent meals. If vomiting persists, return to the clinic for an evaluation. -
Tiredness
Common for the first week or two following initiation with Efavirenz. Important to make sure the client has at least 6-8 hours of “sleep” or quiet time after taking Efavirenz. It is generally recommended that the client takes his/her medication 2-3 hours before going to bed. -
Diarrhoea
Increase fluid intake especially water. Rice and/or rice-water will help control loose stool. Limit the amount of fruits and fruit juice. -
Dry mouth
Increase fluid intake throughout the day. Sour candy may help keep mouth moist. Maintain good dental care, especially by brushing teeth at least twice a day. -
Rash
Clients who develop a rash especially when taking NVP or Abacavir should return to the clinic for an evaluation. Rashes can also be a result of scabies, lice or eczema which require specific treatment. Mild rashes can be managed with Calamine lotion or Chlorpheniramine 4mg at night.
Long-term side effects
-
Lipodystrophy/Fat redistribution
For clients on a zidovudine-containing regimen, consider switching to a tenofovir-based regimen. -
Peripheral neuropathy
- Clients on stavudine should be switched to either tenofovir or zidovudine.
- Clients taking INH for IPT should be on pyridoxine 25mg.
- Review current medications to ensure that the client is not taking any other neurotoxic medication that can be contributing to the symptoms of peripheral neuropathy.
-
Nausea and loss of appetite (possibly as a result of liver damage)
- Assessment for Hepatitis B or C , opportunistic infections (e.g., TB), other GI complications, cancer.
- Ensure that the offending medication, e.g., NVP, is stopped.
-
Nausea, decreased appetite, unexplained weight loss, vomiting, abdominal pain, tiredness, muscle pains and difficulty in breathing (possibility resulting from lactic acidosis)
Refer client to your clinical mentor or higher-level facility. -
Anaemia (client looks pale, feels weak and dizzy)
- Clients on zidovudine must be switched to tenofovir (check creatinine) or abacavir.
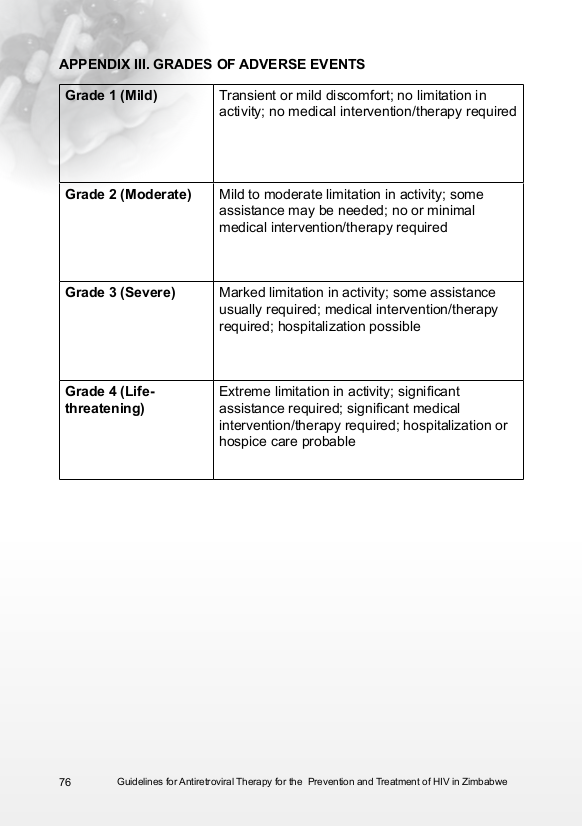
- Monitor FBC and refer for transfusion if Grade 3 or 4 Adverse Event.
-
Headache
-
Case Study: Side Effects Changing Client's Physical Appearance
[activity type]
Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in managing side effects in clients.
Your client, Melody is a single, never-married 27-year-old woman who has been on ART for 4 years. She has been on Stalanev for 3 years and recently switched to Tenolam and NVP. At her last visit, she told you, “these drugs have affected the way I look and men no longer notice me.” Her friend advised her to stop these toxic drugs and start looking at herbal remedies that are available.
Melody has since missed 2 clinic appointments.
-
Which side effect is likely to be affecting her and what advice would you give her?
Stavudine, which is in Stalanev, most likely caused the cosmetic changes (lipodystrophy/fat redistribution) that Melody is concerned about and that is why she was changed to Tenofovir which is in Tenolam. The switch may help reverse some of the changes but unfortunately, the changes may be permanent. Adherence counselling and support are essential in this case. Melody needs to understand that without ART, she is at risk for progressing to AIDS and becoming sick. -
What side effects of ARVs should be discussed that may affect a client’s adherence to medications?
- Lipodystrophy/fat redistribution
- GI upset
- Fatigue
- Dizziness
-
What should you discuss related to use of herbal remedies in the management of HIV?
Treatment for HIV is with antiretroviral medications. When clients take herbal medicines in conjunction with ART, there is a potential risk of interactions that may affect the efficacy of the ART and cause treatment failure. At each visit, the nurse should assess what additional prescription and herbal medications clients are taking.
-
Which side effect is likely to be affecting her and what advice would you give her?
-
Case Study: History of TB
[activity type]
Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in managing side effects in clients.
Bonani was diagnosed HIV+ and her CD4 count was 26 cells/mm³ at baseline. Her record shows that she had a history of TB 3 years prior to her diagnosis but was otherwise asymptomatic. There is no record of a physical examination done at baseline. She started taking 3TC/TDF/EFV = FDC 2 weeks ago and is in clinic today complaining of fevers, night sweats and swollen glands in her neck. Bonani says, “I feel worse than I felt before I began on this medicine. I think they are making me sick so I stopped taking them 2 days ago.”
-
What do you think is causing the symptoms that Bonani is experiencing?
Possible TB IRIS especially due to her low CD4 count at ART initiation -
What subjective and objective information is missing and would have been important in the management of this case?
- TB screening
- Complete physical examination including skin and chest examination
-
What will be included in the management of this case?
- Sputum examination
- Chest x-ray, if available
- TB treatment, if confirmed
- Continue FDC
- Client education and support about the management of IRIS
-
What do you think is causing the symptoms that Bonani is experiencing?
-
Case Study: Early Side Effects
[activity type]
Instructions: Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in managing side effects in clients.
Ngoni is a 31-year-old HIV positive man who just started on a drug regimen of 3TC/TDF/EFV. He shows up at the clinic a week later complaining of a headache and dizziness. He says he has trouble sleeping because he has vivid dreams.
-
What do you think are causing these problems?
CNS toxicity to Efavirenz -
What would you do to minimise these side effects?
- Reassure him that the side effects should decrease over the next week. If not, he should return to the clinic.
- Review how he is taking the FDC: At least 6-8 hours of sleep/quiet time, avoid taking FDC with alcohol, allow sufficient time in the morning to adjust to being awake before driving or using equipment.
-
What do you think are causing these problems?
Antiretroviral Therapy (ART): ART Side Effects
Learning Objectives:
- Assess clients for common and serious side effects of each ARV
- Substitute regimens in adverse reaction cases
-
Assessment
Discussion questions
Tell your mentee you would like to assess his/her knowledge related to ARV side effects.
-
What are common side effects your clients have experienced while on ARVs?
- Headache
- Fatigue
- GI upset
- Diarrhoea
- Dizziness
- Restless sleep
- Abnormal dreams
-
What do you suggest to minimise these common side effects?
- Remind clients that most mild side effects go away in time. If they persist or worsen, return to the clinic for an evaluation.
- Fatigue, dizziness, abnormal dreams, restless sleep are most often caused by EFV. Suggest patient take the FDC earlier in the evening (2-3 hours before going to bed) and avoid drinking alcohol when taking the FDC.
- Gastrointestinal upset (nausea, diarrhoea) – unless instructed, take medication either with a meal or immediately after a meal. Avoid spicy foods. Increase intake of water/fluids especially when taking the ARVs.
-
What are some serious side effects your clients have experienced while on ARVs?
- Renal impairment
- Metabolic abnormalities
- Depression
- Anaemia
-
What action do you take when your client is experiencing a more serious side effects?
Refer client to your mentor or medical officer for assessment and consideration for the substitution of the offending medicine. -
One of your HIV-positive clients who started ART approximately 2 weeks ago presents with fever, sweats, a skin rash, and has been losing weight. What do you think is going on?
IRIS -
What will you do for this client who is experiencing IRIS?
Treat underlying OI. Not stop ARTs. Refer client to medical officer for assessment and treatment. -
One of your HIV-positive clients is on AZT. Her Hb drops to 5 g/dl and she has anaemia. What alternative drug would you prescribe?
Tenofovir, after checking creatinine.
-
What are common side effects your clients have experienced while on ARVs?
-
Activities
-
Mentor Resources