-
Case Study: Adult Male Truck Driver
[activity type]
Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in monitoring and managing treatment failure.
Tafadzwa is a 38-year-old long distance truck driver who stays alone. He has been on first line ART for the past 4½ years. During the first year he was on Stalanev and was then switched to Tenolam-N. His baseline CD4 count at ART commencement was 129.
He has had only one more CD4 count test 2 years ago and it was 375. He admits that occasionally his drug supply has run out while he is on the road. He has had several sexual partners in the last 2 years and he occasionally uses condoms. Tafadzwa presents to your clinic complaining of pain on swallowing for the past 1 week. He admits to unintentional weight loss and intermittent fever.
-
What are the possible reasons for Tafadzwa’s symptoms?
- Oral and/or oesophageal candidiasis
- Possible TB
- Possible treatment failure due to poor adherence
-
What laboratory test or test would you offer Tafadzwa and why?
Since you want to rule out treatment failure, the best test will be a viral load. If viral load is not available, do a CD4 count and compare it with previous results. If he is producing sputum, do TB sputum investigations. Do a CXR if available, if the sputum is negative. -
What factors contributed to Tafadzwa’s first line ART treatment failure?
- Poor adherence, development of drug resistant HIV, possible drug -drug interactions if he is taking medication prescribed by another provider, or herbal medication.
- Possible substance use leading to poor adherence.
- Possible infection from an already resistant strain since Tafadzwa has multiple sexual partners and is not consistently using protection.
-
Tafadzwa has a viral load of > 1000 copies / ml. How would you manage him?
- Thorough assessment of additional medications, herbal pills/drinks.
- Substance use assessment and risk reduction counselling.
- Client education about development & prevention of treatment resistance.
- Increase clinic appointments to monthly if he has been receiving medication every 3 months. If this is not possible with his work, explore other clinic options within his truck route.
- Enhanced adherence support and repeat VL after 3 months. If VL remains high with good adherence, switch to second line. If adherence does not improve, continue adherence counselling until good adherence before switching. If VL suppresses after adherence support, continue first line. Treat and manage any active OIs.
-
What are the possible reasons for Tafadzwa’s symptoms?
-
Case Study: Adult Male with Rash
[activity type]
Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in monitoring and managing treatment failure.
You are covering for the nurse who usually works in the HIV clinic. Moses is a 25-year-old male who presents with a history of NVP/3TC/TDF for 13 months. He is also taking cotrimoxazole and finished TB treatment 2 months ago. His baseline CD4 count was 110 and clinical stage 1 according to the clinic record. His record also shows that Moses has maintained > 95% adherence to his ART medications and completed his TB treatment without any problems.
He comes to clinic today complaining of a painful rash on the right side of his face including his right eye. This started 2 days ago with a “funny sensation” along his face and then small bumps that were itching then painful and spread really fast.
Vital signs:
- B/P 110/75
- Pulse 67 and regular
- RR 16
- Temperature 37.2
- Weight 64kg (down from 67kg 2 months ago)
Physical Exam:
- Thin, speaking slowly and holding the right side of his head in obvious pain.
- EENT: Diffuse rash noted across right side of face stopping below the right eyelid. Open blisters noted especially at the chin area.
- Chest: clear to auscultation.
-
Do you see any potential problems with the management of this case?
TB treatment was initiated and he was kept on NVP. Rifampicin interacts with NVP potentially lowering the required level of NVP needed to control HIV. As per the Zimbabwe guidelines, NVP should be switched to EFV. As long as his adherence was > 95% prior to the switch, the TDF and 3TC could continue. If there is any doubt about his adherence, consult with your clinical mentor or HO about changing to the second-line regimen.Remember: You can only switch a single drug in a HIV regimen if you are certain about the client’s adherence. Switching a single drug when a client has NOT been adherent will lead to the entire regimen becoming resistant.
-
What will you include in your assessment/ differential diagnoses?
- Herpes Zoster.
- Possible treatment failure due to drug-drug interactions between NVP and rifampicin used for TB treatment.
-
What is your plan?
- Acyclovir should be started early. If given from 5 days after onset, it is usually ineffective in altering the course of the illness.
- Paracetamol 1g 6 hourly for pain. If no response, add indomethacin 25mg tds.
- Calamine topical lotion for skin care.
- Consult with clinical mentor about discontinuing current ART regimen.
- Check Hb.
- Do not switch to second line at this point. There is a need to confirm the failure before starting the second line regimen. Addressing adherence issues and consulting with expert support (clinical mentor) is necessary.
- Client education to address new ART regimen, dosing, schedule, food requirements.
- Stepped up adherence counselling.
- Amitriptyline 25mg at night. Increase by 25mg every 2 weeks if needed to 75mg.
- Follow-up in one week to evaluate HZV response to acyclovir, pain management and tolerance to new ART regimen. Remind client to come back to clinic sooner if condition worsens or if he has trouble with his medications.
Antiretroviral Therapy (ART): ART Treatment Failure/Resistance
Learning Objectives:
- Identify treatment failure and manage it appropriately
- Prescribe the correct ARVs for the alternative first line according to national guidelines
- Manage clients failing on second line therapy.
-
Assessment
Case study
[assessment description]
Nyasha is a 25-year-old-woman who has been taking AZT + 3TC + NVP for 3 ½ years. She was diagnosed during her first ANC clinic visit 4 years ago. She started taking AZT 300mg twice daily at 28 weeks of her pregnancy and was given (Sd) NVP 200mg + AZT and 3TC during labour. Her baby tested HIV negative.
A note in her ANC clinic record indicates that postpartum she was given AZT and 3TC twice daily for 7 days but she “refused to take any additional medication especially since she was breastfeeding.”
Six months after delivering her baby she returned to the HIV clinic complaining of fatigue and oral candidiasis. She was treated successfully for the candidiasis and started on AZT + 3TC + NVP, which is her current regimen. She returns today for her scheduled clinic appointment complaining of the same “white stuff” on her tongue that she had a few years ago.
-
What are some of the treatment issues Nyasha is facing?
- ART drug resistance
- Has new OIs oral candidiasis
-
What are the steps you need to take to determine if Nyasha’s virus has become resistant to her current ART regimen?
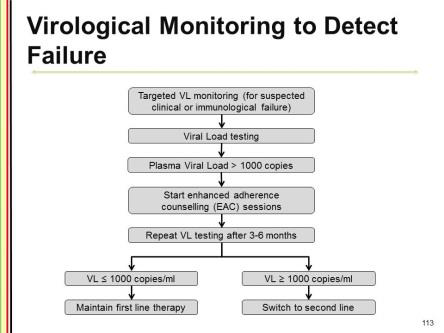
Viral load (VL) testing is the gold standard for monitoring response to ARV medicines but due to limited resources, Zimbabwe will do targeted VL testing. Viral load tests can determine from a blood sample how much virus is replicating in the body. If viral load increases substantially while a person is on a combination of ART, the most likely reason is drug resistance. Unfortunately, viral load tests cannot tell which particular drug the HIV is resistant to. If there has been a threefold increase in the VL from the lowest point following treatment, it is an indication of treatment failure. In such situations, one must review the treatment regimen and consider changing the regimen.In the absence of VL testing, measuring her CD4 count and clinical monitoring are ways to identify possible HIV treatment failure due to resistance. Persistently declining CD4 counts as measured on two occasions, at least three to six months apart and clinical deterioration are suggestive of treatment failure.
A thorough assessment of her adherence is critical to determining potential treatment failure/resistance although even client’s with > 95% adherence can develop resistance. This can be due to either the client being initially infected with an already resistant virus OR the virus developing mutations despite effective ARV drug levels.
-
How do you know that Nyasha is in clinical failure and doesn’t have IRIS?
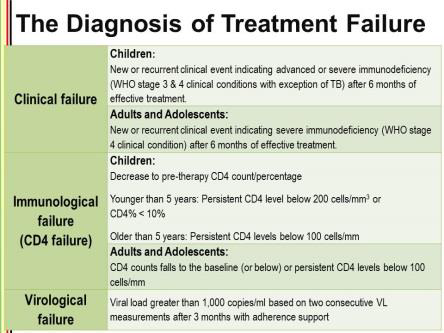
- ART treatment failure can be identified three ways: 1) virologic failure, 2) immunologic failure, and 3) clinical failure.
Clinical failure generally occurs after the individual has been on ART for over 3 months and is the last of the three failures to be identified. Once new clinical symptoms or an OI appears, the viral load has already increased and the CD4 count has dropped. - In most cases (but not always), new symptoms appearing shortly after starting ART are due to the immune reconstitution syndrome, drug-drug interactions or drug side-effects. New symptoms appearing a long time after starting ART are more likely to be an indication of treatment failure/resistance.
- ART treatment failure can be identified three ways: 1) virologic failure, 2) immunologic failure, and 3) clinical failure.
-
When should you change ART?
There are a few options available for adjusting or altering the ART regimen when necessary. Of course, this is always done in close consultation with the health care team. Switching to a second line regimen should only occur after attempting identify the causes of poor adherence including a thorough assessment of possible substance use. Intensive adherence counselling is needed before switching regimens as poor adherence to treatment is the most common cause of ART failure. It is advisable to repeat the viral load test after sessions of adherence counselling just to make sure that the viral non suppression was not a result of missing doses. Changing 1 drug in a failing regimen leads to early resistance of the new drug, so you must change all 3 drugs. If poor adherence continues despite counselling, try improving adherence by using of a mobile phone alarm or treatment supporter. Consult with your clinical mentor or HO to decide the best management. REMEMBER: Poor adherence to a first-line regimen may continue when the client is switched to a second-line regimen and there are a limited number of ARVs available! -
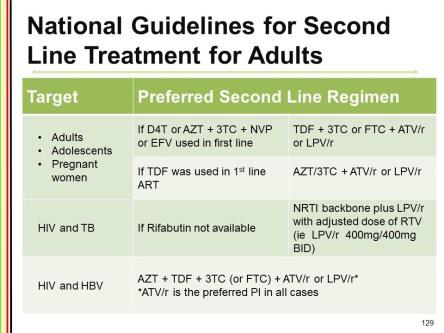
After intensive adherence counselling and monthly follow-up that includes a pill count, if Nyasha’s repeat VL or CD4 count in 3 months does not improve according to the guidelines, what second line ARVs would you prescribe (after consultation with your clinical mentor or HO)?
TDF + 3TC or ATV/r or LPV/r -
What third line drugs would be prescribed by the specialist (after viral load and genotype testing)?
Raltegravir (400mg) twice daily, darunavir (800mg)/ritonavir (100mg) once daily, plus any other medicines as determined by the lab tests (where available). Note that laboratory back up is very crucial in this case. There is no emergency in starting third line. Instead of blindly starting ARVs, medicines should be selected based on the results of a thorough evaluation of the client. Ensure that there are no adherence issues.
-
What are some of the treatment issues Nyasha is facing?
-
Activities
-
Mentor Resources
-
The Diagnosis of Treatment Failure
-
Virological Monitoring to Detect Failure
-
Second Line Treatment for Adults
-
Third Line Regimen
Those failing second-line therapy will need to be referred for Specialist assessment prior to recommending the third-line medicines.
Third Line Regimen
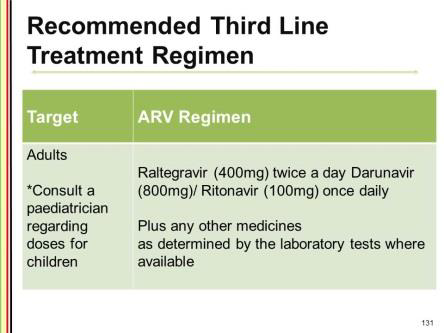
Those failing second-line therapy will need to be referred for Specialist assessment prior to recommending the third-line medicines.
×
-