-
Case Study: HIV Positive Man
[activity type]
Tell your mentee that you will review a case and ask some questions to assess his or her knowledge in TB treatment.
A 30-year-old HIV-positive man came to the clinic on Monday. He complained of a cough that lasted for 1 week. He reports purulent expectoration, chest pain, shortness of breath, and chills last night. You conducted a patient history and physical exam. You considered bacterial pneumonia and TB as the differential diagnoses. You conducted an AFB, and because your clinic has no x-ray machine, a chest examination. Chest examination: No wheezing heard. Rales noted RLL. Coughing on inspiration. Spot sputum specimen – negative.
-
What questions would you ask him?
Do you take ARVs?
Ever had an OI?
Do you know your CD4?
Case continues…
Patient reports that he does not take ARVs, has not had a previous OI, and does not know his CD4 count.-
How will you manage the patient?
Amoxicillin 500mg three times a day for 5 days. -
How will you follow up?
Advise patient to return to hospital for review after completing the antibiotic to see if he has responded to the antibiotics. Advise to return sooner if his condition worsens.
Case continues…
After 4 days of antibiotic treatment, the patient comes back with increased shortness of breath. The fever is still high (39 degrees C). He has some white patches inside his mouth.-
What will you do?
- Give the patient Clotrimazole or Miconazole topical application or Fluconazole 400mgs as a single dose for the white patches (oral candidiasis) in his mouth.
- Did he bring the second sputum specimen to the clinic as instructed? If so, check the results. If negative, further assessment needed to establish whether or not TB is “likely” or “unlikely.” Consultation with your HO and/or mentor is recommended if you are unsure. If TB is likely, initiate TB treatment. If unlikely, look for other diseases and treat appropriately. Assess his current CD4 count results and if not done in the past 6 months, repeat today.
- Comprehensive assessment of adherence challenges and disclosure and discuss strategies for improvement, e.g., treatment supporter.
- Close follow-up is needed with this case.
-
What questions would you ask him?
-
Case Study: HIV Positive Pregnant Woman
[activity type]
Tell your mentee that you will review a case study and ask some questions to help him/her improve skills in TB treatment.
-
Part A
Mary Sima, a 35-year-old mother of four who is married, comes to the clinic for the first time. She shows you written confirmation of her HIV test (done on January 12, 2004) that indicates that she is HIV+. At that time, the VCT clinic recommended that she come to the health centre but she felt "fine.” She has come today because she has had a painful rash on one side of her chest for the past 2 days, which has not been helped by the cream she has at home. She has never been on ART.
She and her husband would like to have children. Her last menstrual period was over one month ago. She thinks that she could be pregnant, but is not sure.
Except for the rash her clinical review is negative. Her weight is 54 kg. On physical exam you see a dark red vesicular (blistering) rash over the right side of her chest extending to her back but does not cross the midline. She has no rash in her eye or the rest of her body. Her rapid pregnancy test is positive, and she is in her first trimester of pregnancy.
-
What clinical stage is Mary?
Stage 2 (Herpes Zoster) -
Are there any additional laboratory tests that need to be done at this visit?
Yes. CD4 count, Hb, creatinine, RPR, glucose/urine microscopy, culture and sensitivity (m/c/s) since she is pregnant, blood group, and hepatitis screen, which are antenatal investigations. -
What treatments or prophylaxis would you recommend?
- ART initiation – EFV 600mg/TDF 300mg/3TC 300mg FDC once daily at bedtime
- Cotrimoxazole prophylaxis and acyclovir for the herpes zoster
- Acyclovir for the HZV
- Give analgesia such as paracetamol around the clock not PRN for the herpes zoster
-
Does Mary qualify for IPT and if so, what mediations will you prescribe and when will this start?
Mary qualifies for IPT in principle but she has to be commenced about 3 months after starting ARVs and upon undergoing a TB screening process to exclude active TB. Exclude history of excessive alcohol intake and active liver disease. So for this current visit she does not qualify for IPT.
-
What clinical stage is Mary?
-
Part B
Mary returns one week later as scheduled and tells you that her rash has improved. You do a clinical review, which is negative. Her weight remains the same and her rash has visibly improved. Her CD4 count is 180cells/mm³. She is still working at home and has gone to PMTCT as was recommended by you at the last visit.
-
When would you recommend this patient to follow-up?
- In 2 weeks’ time to check on the treatment progress
- Screen for TB again
- Check for weight changes
- Review all investigation results and manage accordingly
- Address all her adherence issues
- Discuss infant feeding
-
When would you recommend this patient to follow-up?
-
Part C
Mary returns earlier than her scheduled follow-up, because she had developed a cough and fever for the last 2 weeks. She tells you that she feels very sick. On her clinical review besides the cough and fever she also has night sweats and poor appetite. Her weight is now 52 kg. Right now she is unable to do housework but is able to move around. She has not missed any doses of the cotrimoxazole.
-
What are your recommendations for management of her current problem and follow-up?
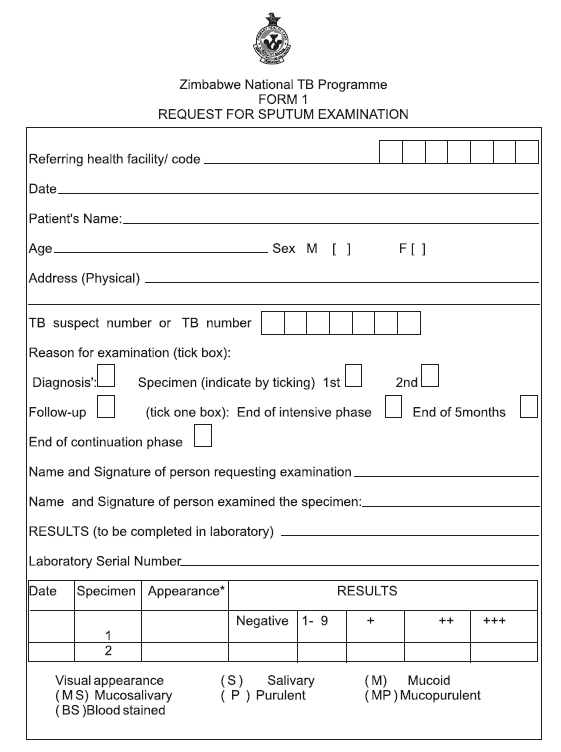
She has signs and symptoms suggestive of TB, possibly due to IRIS, and needs further investigations – sputum for AAFBs and CXR.
-
What are your recommendations for management of her current problem and follow-up?
-
Part D
Mary’s first spot sputum specimen is positive.
-
What are your recommendations for management of her current problem and follow-up?
She has TB and should be commenced on Cat 1 anti TB medication. -
Will you need to make any changes to her antiretroviral medication?
No! It is important that Mary understand the importance of continuing her ART. A simple explanation about IRIS is also helpful. One way to explain could be: “Sometimes when a person’s soldier cells (CD4 cells) are very low, the ART wakes up the cells and any infection such as TB that may not have been making a person sick. The ART is helping the “soldier cells” work hard to improve and strengthen her immune system, the system that keeps us healthy. So it is very important that you continue her ART and not miss any doses. The ART along with the TB medication will cure the TB and have you feeling stronger very soon. It is important for you to continue taking your medication without skipping dosses, both for your own health and to reduce the risk of passing TB and HIV to your unborn baby.” -
Mary was never started on IPT since she developed TB prior to initiation. In this case, would Mary need IPT in the future? If so, when would she be eligible and what would you prescribe? If not, explain why.
Mary will be eligible for IPT following the successful completion of her TB treatment. This is called secondary prevention. She will be prescribed INH 300mg daily and Pyridoxine 25mg daily for 6 months. As with ART, adherence to IPT will be closely monitored.
-
What are your recommendations for management of her current problem and follow-up?
-
-
Case Study: Side Effects
[activity type]
[activity instructions]
Mduduzi presented to the clinic complaining of a productive cough, weight loss, and night sweats. He had no previous history of TB and no TB contacts that he was aware of. His evaluation included an HIV test that was negative and sputa sent that were 2+, AFB positive x 2. He was started on RHZE 4 tabs daily 2 weeks ago. He returns to the clinic today complaining of orange-red urine, joint pains, and nausea with the medication.
-
What medications do you suspect could be causing each of the problems identified by Mduduzi?
Joint Pains ‐ Arthralgia can be caused by several of the medications used to treat TB including isoniazid, rifampicin, and pyrazinamide. Pyrazinamide can cause gout with elevations of uric acid, which may require treatment with allopurinol if severe.
Nausea ‐ Nausea is a common problem and is often from rifampicin but can also be from any of the TB medications.
Orange-red urine ‐ Discolored body fluids including urine are normal side effects of rifampicin and is not harmful.
-
What patient education can you provide to decrease or eliminate the problems Mduduzi is experiencing?
Arthralgia can often be managed with aspirin or NSAIDS.
Nausea can be managed or eliminated by instructing patients to take the TB medication with food or at night before bed. Patients should avoid drinking alcohol while taking TB medicine and eliminate spicy foods and coffee from their diet. Anti-emetics may be used temporarily until the nausea subsides. It is important to instruct patients to return to the clinic if the nausea continues or increases or if they are vomiting as this may indicate hepatotoxicity.
Case continues…
Mduduzi returns 2 days later and tells you that he started developing an itchy rash yesterday that seems to be getting worse. He also tells you that his feet are burning at night especially after he has been working all day. He thought his shoes were too small since they felt very tight but he realized that all of these new problems he is having is ever since he started the TB medication. He is visibly upset, telling you that he is having trouble working and his boss is asking him what is wrong. He is concerned that he may lose his job and will not be able to provide for his family. He tells you that you must do something to make this treatment better or he does not think he can continue.Your examination reveals a faint macular rash over his arms and chest. Vital signs are normal. Targeted neurologic exam reveals diminished temperature, light touch and vibratory sensation on both feet L>R.
-
Which medication do you suspect is causing the rash?
Rashes are common and can be caused by rifampicin, isoniazid, or streptomycin. -
What care management is needed for his rash and what patient education will you provide?
Rashes from TB medication are usually mild and can be managed with antihistamines and calamine lotion.
TB medication can and should continue when a mild rash develops.
Patients must be instructed to return to the clinic or nearest hospital if the rash worsens or if they develop a fever or mucous membrane involvement occurs (such as blisters or mouth sores).
-
Which medication do you suspect is causing the pain in his feet?
Burning sensation and foot pain which are signs of peripheral neuropathy is caused by Isoniazid -
What treatment is needed for peripheral neuropathy that develops as a side effect of Isoniazid?
Pyridoxine 50mg up to three times daily -
Who are more at risk for developing peripheral neuropathy during TB treatment?
Pregnant women, alcoholics, patients with chronic liver disease, HIV, malnutrition and diabetics -
How can peripheral neuropathy be prevented in patients requiring TB treatment?
In patients at risk for peripheral neuropathy, give Pyridoxine 10mg daily for the duration of treatment.
-
What medications do you suspect could be causing each of the problems identified by Mduduzi?
-
Role Play: HIV Positive Woman
[activity type]
Explain to the mentee that you are going to engage in a role play to help him or her learn how to improve TB treatment skills. He or she will play the role of health care provider, and you will be the patient.
Show the mentee the instructions below for the health worker. Then tap on the box for the patient instructions. Do not show this to the mentee.
A 46 year-old-woman has come to the health facility. She tested HIV positive last month, when she was hospitalised for abdominal pain and fever. During her hospital stay she was started on TB treatment for extra pulmonary TB. She has come for follow-up after the hospitalization. She still feels weak and wants to know about her health.-
Patient instructions (mentor). Do not show this to the mentee.
Your task is to act the role of this TB patient. You are taking TB medicines and cotrimoxazole and are tired of taking so many medicines. You are unable to work because you are too weak. Your husband knows that you are HIV+ but has not had time to take his test yet. You and your husband use condoms regularly. You have 4 older children, and do not want more. Your LMP was 1 week ago.
Your job is to listen carefully during the role play so that you can comment on what was done well and what could be improved.
Check the boxes below to indicate whether the mentee asked the appropriate questions. At the end of the role play, review any problem areas with the mentee.
-
-
Role Play: DSTB
[activity type]
Explain to the mentee that you are going to engage in a role play to help him or her learn how to improve TB treatment skills. He or she will play the role of health care provider, and you will be the patient.
Show the mentee the instructions below for the health worker. Then, tap on the box for the patient instructions. Do not show this to the mentee. Note there is a Part 1 and Part 2.
Part 1
A 28-year-old woman has come to the health facility. She has been on Drug Susceptible TB (DSTB) treatment for the first time and was diagnosed 5 months ago, but 3 months ago she stopped going for treatment. However, in the last month she has started losing weight again and has been feeling very unwell and very tired. She is also coughing, which is productive.-
Patient instructions (mentor). Do not show this to the mentee.
Your task is to act the role of this TB patient. You currently do not have a partner. You had 3 in the past, including your deceased husband. You live in a small 3-room house with your sister and her children. You had an HIV test but you never returned to collect the results. You stopped going to the clinic for TB treatment because it was too far and you were feeling better. You want to know why you are feeling like this since you already have taken TB medicine.
Your job is to listen carefully during the role play so that you can comment on what was done well and what could be improved.
Check the boxes below to indicate whether the mentee asked the appropriate questions. At the end of the role play, review any problem areas with the mentee.
Part 2
She returns 3 days later. The results of her visit are:
Sputum: Sputum positive for AAFBs
Still coughing
Temperature: 39C
Previous HIV test: Positive-
Patient instructions (mentor). Do not show this to the mentee.
You ask the health care provider:
- How can I have TB again when I have been on treatment for TB before?
- Why has it not been cured?
- What does it mean now that I am also HIV positive?
Your job is to listen carefully during the role play so that you can comment on what was done well and what could be improved.
Check the boxes below to indicate whether the mentee asked the appropriate questions. At the end of the role play, review any problem areas with the mentee.
-
-
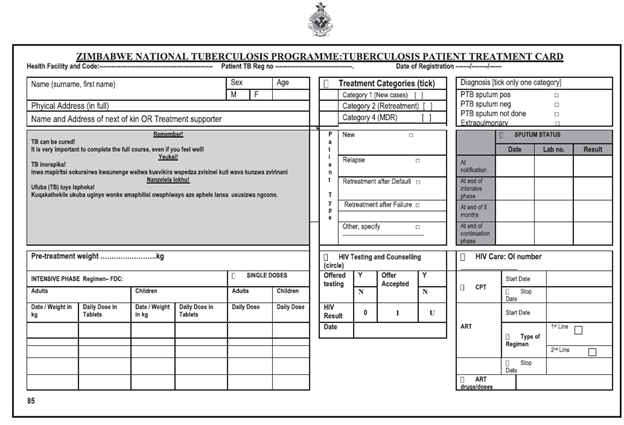
Observation: TB Treatment Card
[activity type]
Tell your mentee you would like to assess his/her knowledge related to proper completion of the TB Treatment Card, a record of the patient’s diagnosis and TB treatment. One should be created for every TB patient and kept at the health facility
Inform your mentee that the purpose of this activity is to support him/her in his/her learning and guide him/her in how he/she can improve his/her practice.
Following the observation, provide feedback to your mentee and give mentorship as needed.
Observation Checklist
-
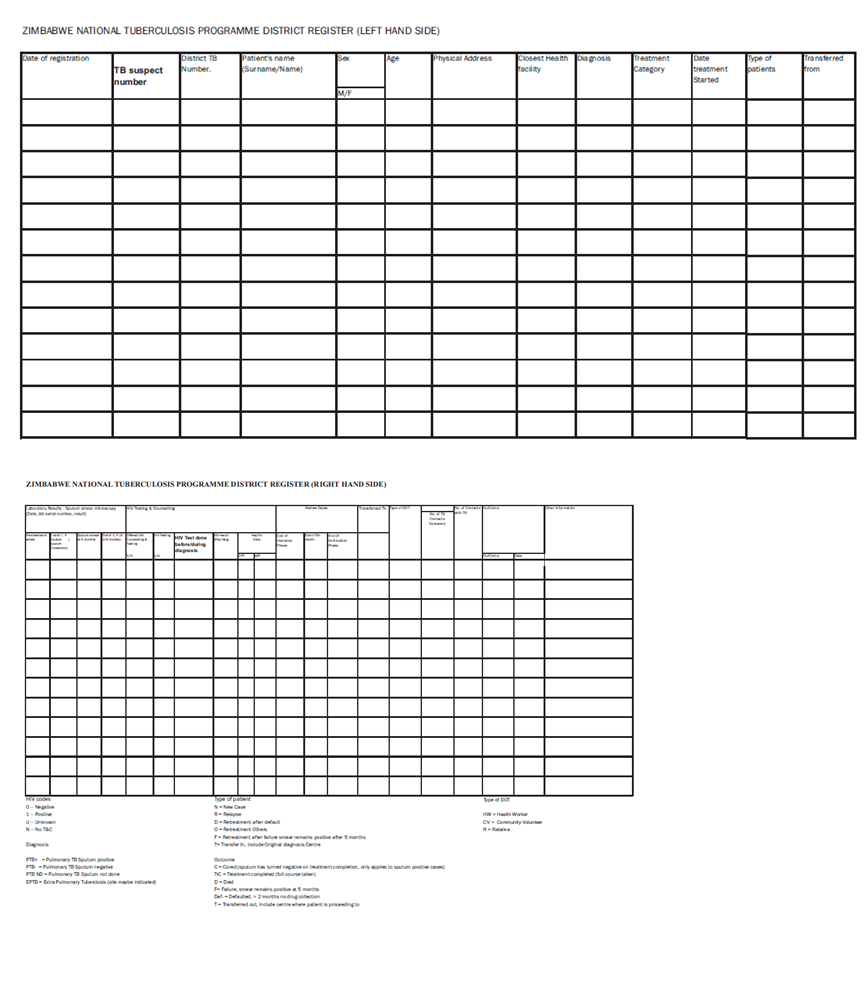
Observation: District TB Register
[activity type]
Tell your mentee you would like to assess his/her knowledge related to proper completion of the District TB Register Inform your mentee that the purpose of this activity is to support him/her in his/her learning and guide him/her in how he/she can improve his/her practice.
Following the observation, provide feedback to your mentee and give mentorship as needed.
Observation Checklist
-
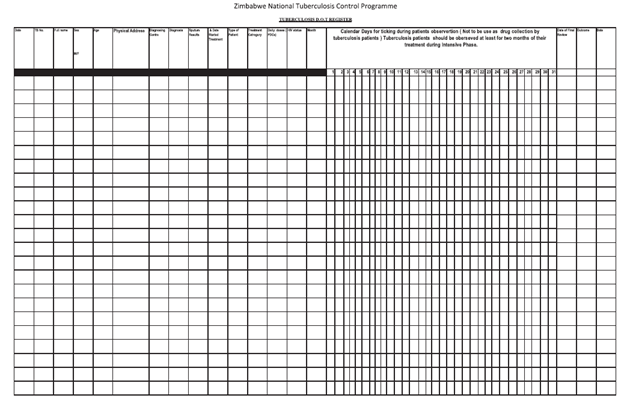
Observation: DOT Register
[activity type]
Tell your mentee you would like to assess his/her knowledge related to proper completion of the DOT Register. Inform your mentee that the purpose of this activity is to support him/her in his/her learning and guide him/her in how he/she can improve his/her practice.
Following the observation, provide feedback to your mentee and give mentorship as needed.
Observation Checklist
-
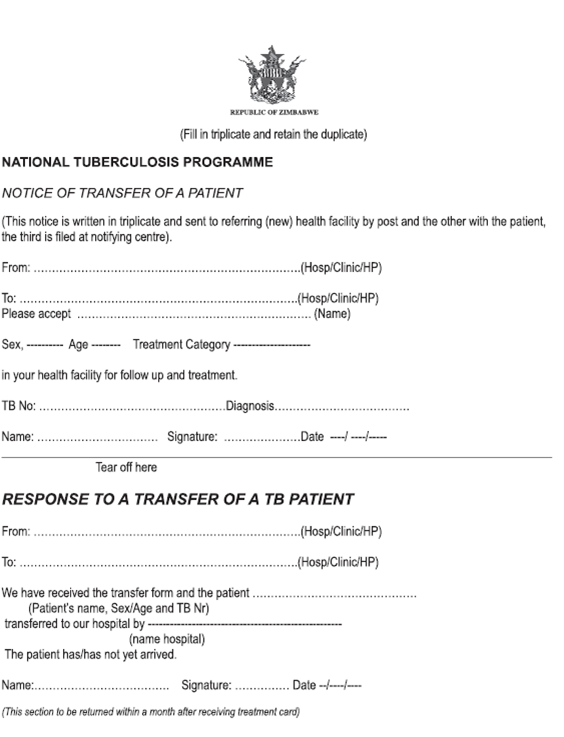
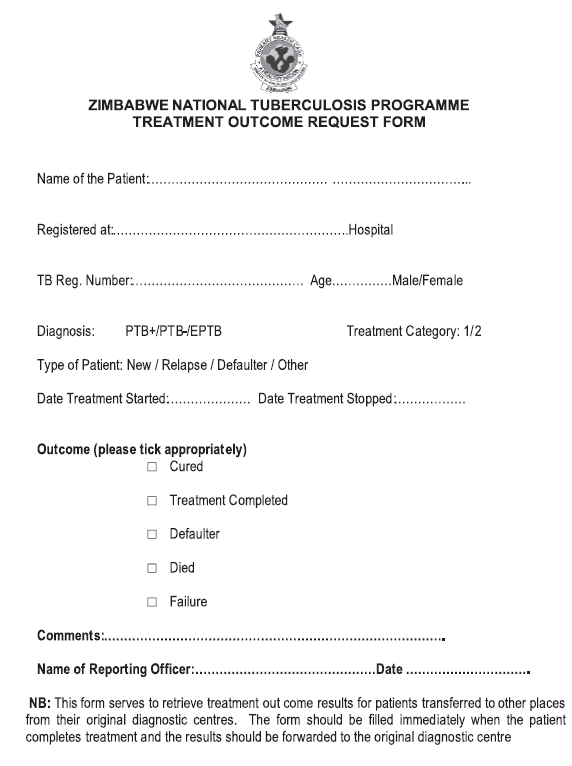
Observation: Transfer Patient Form
[activity type]
Tell your mentee you would like to assess his/her knowledge related to proper completion of the Transfer Patient Form. Inform your mentee that the purpose of this activity is to support him/her in his/her learning and guide him/her in how he/she can improve his/her practice.
Following the observation, provide feedback to your mentee and give mentorship as needed.
Observation Checklist
-
Discussion: TB Treatment Support
[activity type]
Ask your mentee to reflect on TB treatment support.
- Can most TB patients who are detected at your health facility easily come to the health facility for directly-observed treatment? If not, what could help overcome this challenge?
- Have you used community TB treatment supporters before? What worked well, and what needs improvement?
- If someone used community TB treatment supporters before:
- What types of community TB treatment supporters have been effective?
- What problems were encountered?
- If no one has used community TB treatment supporters before:
- Can you try using community TB treatment supporters in the future? What are possible barriers and how can you overcome these?
- Do patients at your facility use family treatment supporters?
- What types of family treatment supporters have been effective?
- What problems were encountered?
- What type of treatment supporters could be effective and acceptable to patients?
Summarise the discussion by emphasising how community treatment and family supporters can play a significant role in reducing the burden on health facility staff. Encourage mentee to think about how he or she can engage the community organisations at their health facilities.
-
Quiz: Treatment Regimens
[activity type]
Instructions: Tell your mentee that you will ask them some questions and discuss answers to improve their knowledge in TB treatment regimens for special cases.
-
Question 1
What TB medication interacts with ARVs?
[note text]Rifampicin interacts with certain antiretroviral drugs so it is important to assess if there needs to be a change in a regimen if a person develops TB while already taking ART. This will apply to persons who are on a Nevirapine based or Protease-based regimen.
-
Question 2
If a patient with HIV develops TB, and is not currently on ARVs, can you wait to start them until TB treatment is over?
[note text]No. ART should be started at least 2 weeks after the start of TB therapy, that is, during the intensive phase when the patient has stabilized on TB treatment regardless of their CD4 count status. TB/HIV co-infected patients with severe immunosuppression such as CD4 count < 50 cells/mm³ should receive ART early—within the first 2 weeks of initiating TB treatment. In all cases, active TB must always be treated without delay because of the high risk of disease progression and death.
-
Question 3
Are TB medications safe in pregnancy?
[note text]Every woman of childbearing age should be asked whether she is pregnant before commencing anti-TB treatment. Most anti-TB drugs are safe in pregnancy, except for streptomycin, which is ototoxic to the foetus and should be omitted. Do not give streptomycin to a pregnant woman. Streptomycin is part of the retreatment regimen. Use ethambutol instead of streptomycin. The successful outcome of pregnancy depends on the successful completion of TB treatment. If the woman is or may be pregnant and has defaulted or is a treatment failure, refer her to a clinician who can prescribe an appropriate retreatment regimen.
-
Question 4
If a pregnant woman has smear-positive TB, what treatment should the newborn baby receive? Can mother and baby stay together during treatment?
[note text]Full TB treatment is safe and is the best way to prevent transmission of TB to the baby. If the mother has smear-positive TB then the baby should receive INH preventive treatment (5 mg/kg for 6 months). When preventive therapy is completed, give the infant BCG, if not yet given. As far as possible, mother and child should stay together for the entire duration of treatment.
-
Question 5
Are there any special considerations for a woman using oral contraceptive pills and being treated for TB? What are they and what are her options?
[note text]Yes. Rifampicin reduces the efficacy of the contraceptive pill. Dual protection through both hormonal and barrier methods is recommended. A higher dose of oestrogen may be prescribed along with the recommendation for the couple to use a male or female condom every time they have sex.
There is need to intensify counselling for family planning so that the woman and her partner can understand why it is important for them to have a reliable family planning method and emphasize the need for dual protection.
-
Question 6
Can patients with liver disorders safely take TB medications?
[note text]Provided there is no clinical evidence of chronic liver disease, patients with the following conditions can receive the usual short-course chemotherapy: hepatitis virus carriage, a past history of acute hepatitis, and excessive alcohol consumption.
-
Question 7
If a patient with established chronic liver disease has TB, what is your course of action?
[note text]Refer to the clinician. These patients should not receive pyrazinamide. Safe drugs in such patients are INH, rifampicin, plus one or two non-hepatotoxic drugs such as ethambutol or streptomycin, which can be used for a total of eight months.
-
Question 8
If a patient with acute hepatitis (e.g., acute viral hepatitis) has TB, what is your course of action?
[note text]Refer to the clinician. The occurrence of TB and acute hepatitis unrelated to TB is rare. Clinical judgment is necessary. It may be prudent to defer treatment in some cases, while in others it may be necessary to continue with anti-TB treatment. Streptomycin and ethambutol given up to a maximum of three months is the safest option until the hepatitis has resolved. The patient can then receive a continuation phase of INH and rifampicin for 6 months (6HR).
-
Question 9
If a patient with renal failure, has TB, what is your course of action?
[note text]Streptomycin and ethambutol are excreted by the kidneys and should be avoided unless there is specialised care. The safest regimen to give in renal failure is 2HRZ/6HR.
-
Question 10
If a patient has had TB in the past, is there any way to prevent getting TB again?
[note text]Yes. Isoniazid Preventive Therapy (IPT) can be started after successful completion of TB treatment or at any time after a previous episode of TB. Health education is an integral part of TB prevention in the community.
-
Question 11
Can IPT be given to pregnant women?
[note text]Yes. After excluding active TB, IPT can be started at any time during the pregnancy and should be completed if a woman becomes pregnant while taking IPT.
-
-
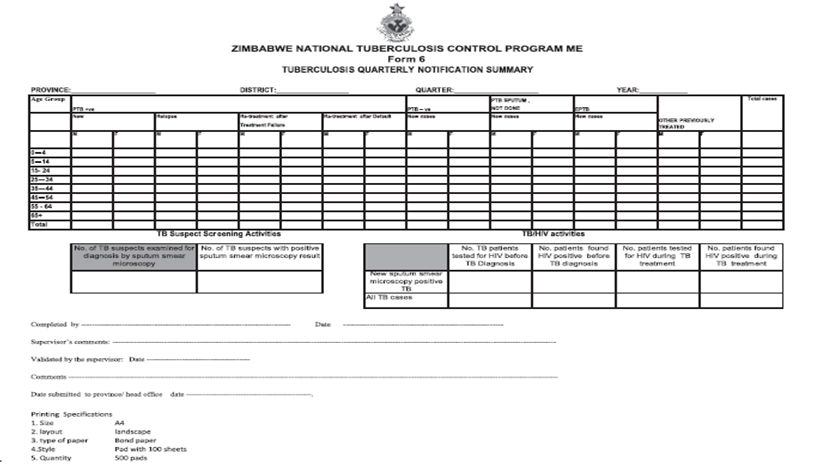
Quiz: TB Quarterly Notification Summary Form 100
[activity type]
Tell your mentee that you will have ask him/her some questions and discuss answers to improve his/her knowledge in TB Quarterly Notification Summary Form 100.
-
What is this form used for?
Reporting the status of district TB cases, including the number of new cases notified, to the provincial and national authorities each quarter.
-
Who fills out this form?
District TB coordinator.
-
When is this form filled out?
Each quarter, based on the data collected from each of the clinics in the district.
-
Look at the presumptive TB case screening activities. What do these numbers tell you? How do you know if they are they too high or too low?
-
-
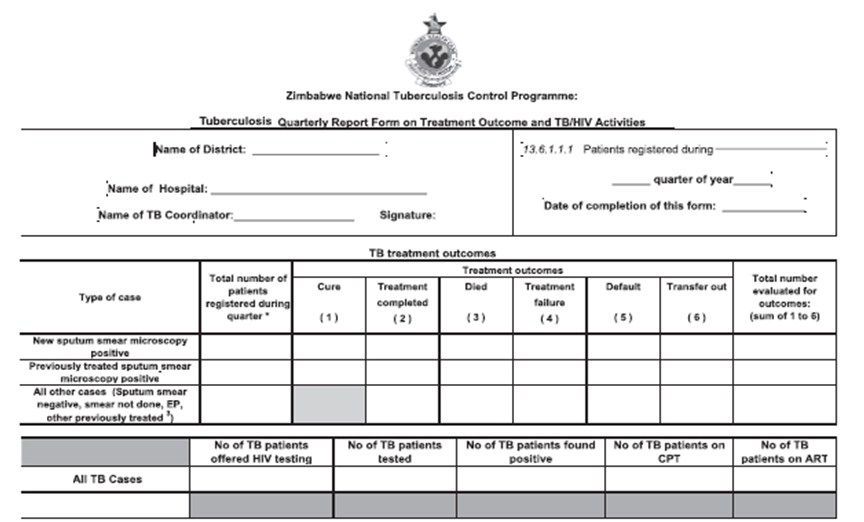
Quiz: TB Quarterly Outcome Report and TB/HIV Activities Form 102
[activity type]
Tell your mentee that you will have ask him/her some questions and discuss answers to improve his/her knowledge in TB Quarterly Outcome Report and TB/HIV Activities Form 102.
-
What is this form used for?
Reporting the treatment outcomes of all TB cases that had been registered. This report is sent to provincial and national TB programme offices.
-
Who fills out this form?
District TB coordinator.
-
When is this form filled out?
Each quarter.
-
Look at the section on TB/HIV at the bottom of the form. What do these numbers tell you? How do you know if they are they too high or too low?
-
TB/HIV Co-Infection: Treatment
Learning Objectives:
- Manage TB/HIV co-infection in adults and adolescents
- Prescribe appropriate TB regimens
- Identify community support for patients with TB and HIV
-
Assessment
Case Study
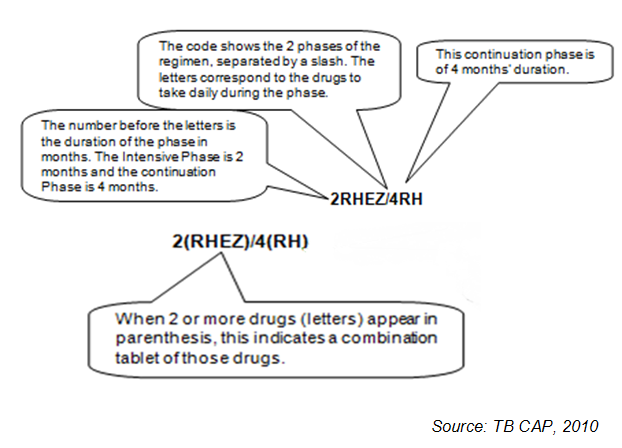
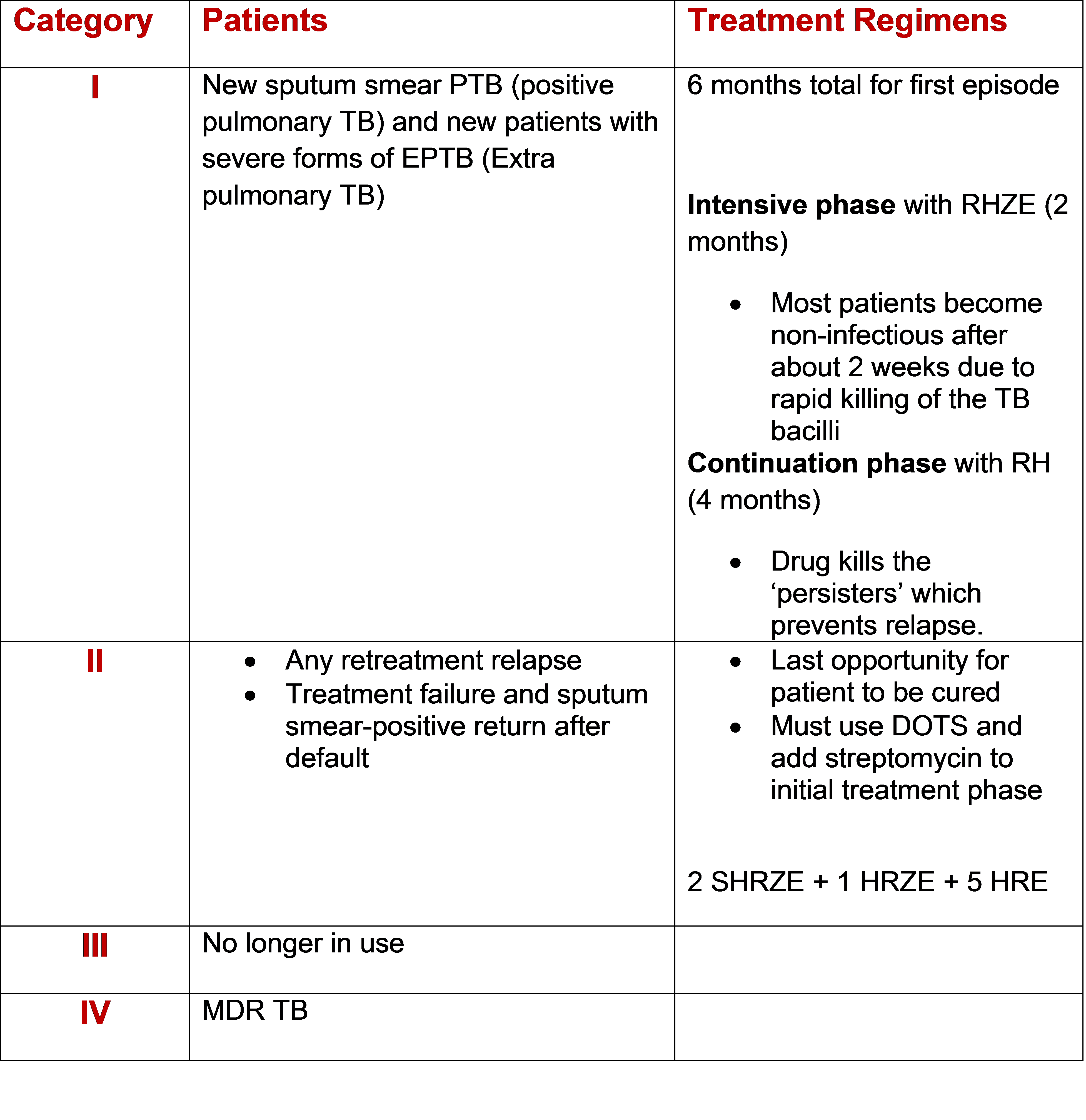
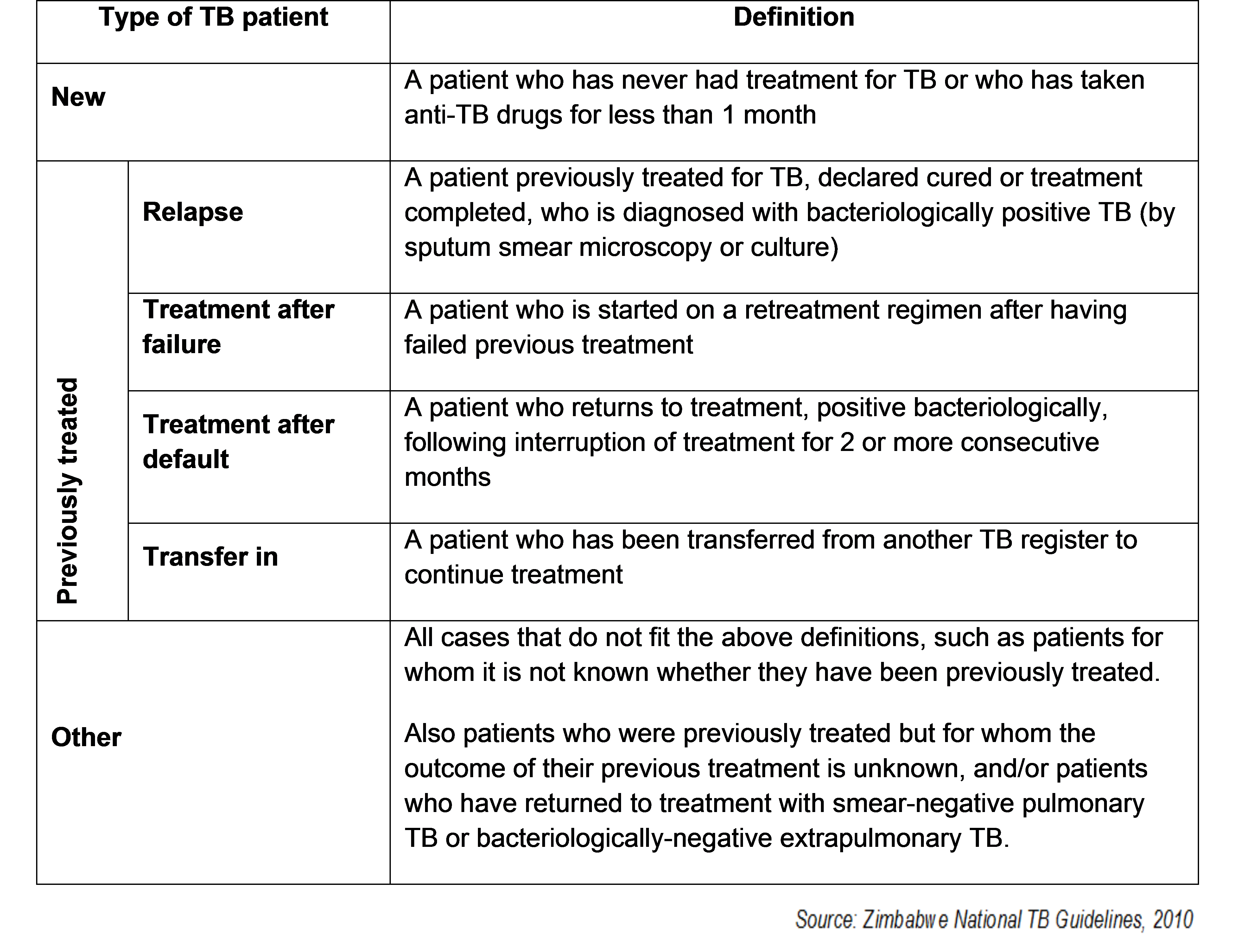
Tell your mentee that you will review 5 case studies and ask some questions to assess his or her knowledge in TB treatment. Refer to the following resources: Drug Abbreviations, How to Read the Drug Code, Treatment Categories, and Types of TB Cases in the mentor resources section.
-
Tariro has just been diagnosed with TB. She has never been treated before and in fact she has never been seriously ill in her life. What is the appropriate treatment regimen and why?
CATEGORY I: 2HRZE 4HR because she is a new case of TB.
-
T.A. is a 45-year-old male with an SS positive result. He has never taken anti-TB drugs and does not report any contact with MDR-TB patients. What is the appropriate treatment regimen and why?
CAT I: 2HRZE 4HR because he is a new smear positive pulmonary TB case.
-
P.Y. is a 38-year-old female patient with an SS positive result. She was previously treated for TB. When asked about her treatment outcome, she reports that she took the treatment for 8 months. The health care worker told her that she was cured. What is the appropriate treatment regimen and why?
CAT II: 2SHRZE 1HRZE 5HRE because she is a retreatment smear positive case.
-
G.K. is a 52-year-old male with an SS positive result. He was previously treated for TB. When asked about his treatment outcome, he reports that he took the treatment for 6 months. The health care worker at the health facility told him that the treatment did not work. What is the appropriate treatment regimen and why?
CAT II: 2SHRZE 1HRZE 5HRE because he had treatment failure.
-
A.K. is a 27-year-old female with an SS positive result. She was previously treated for TB. She took treatment for 3 months at the Central Park Health Service on and off and stopped treatment before completion. She was tested for HIV 3 months ago and the results were negative. What is the appropriate treatment regimen and why?
Cat II: 2SHRZE 1HRZE 5HRE because she is receiving retreatment after default.
-
-
Activities
-
Mentor Resources
-
TB Treatment Card
-
District TB Register
-
DOT Register
-
Notice of Transfer of a Patient
-
Treatment Outcome Request Form
-
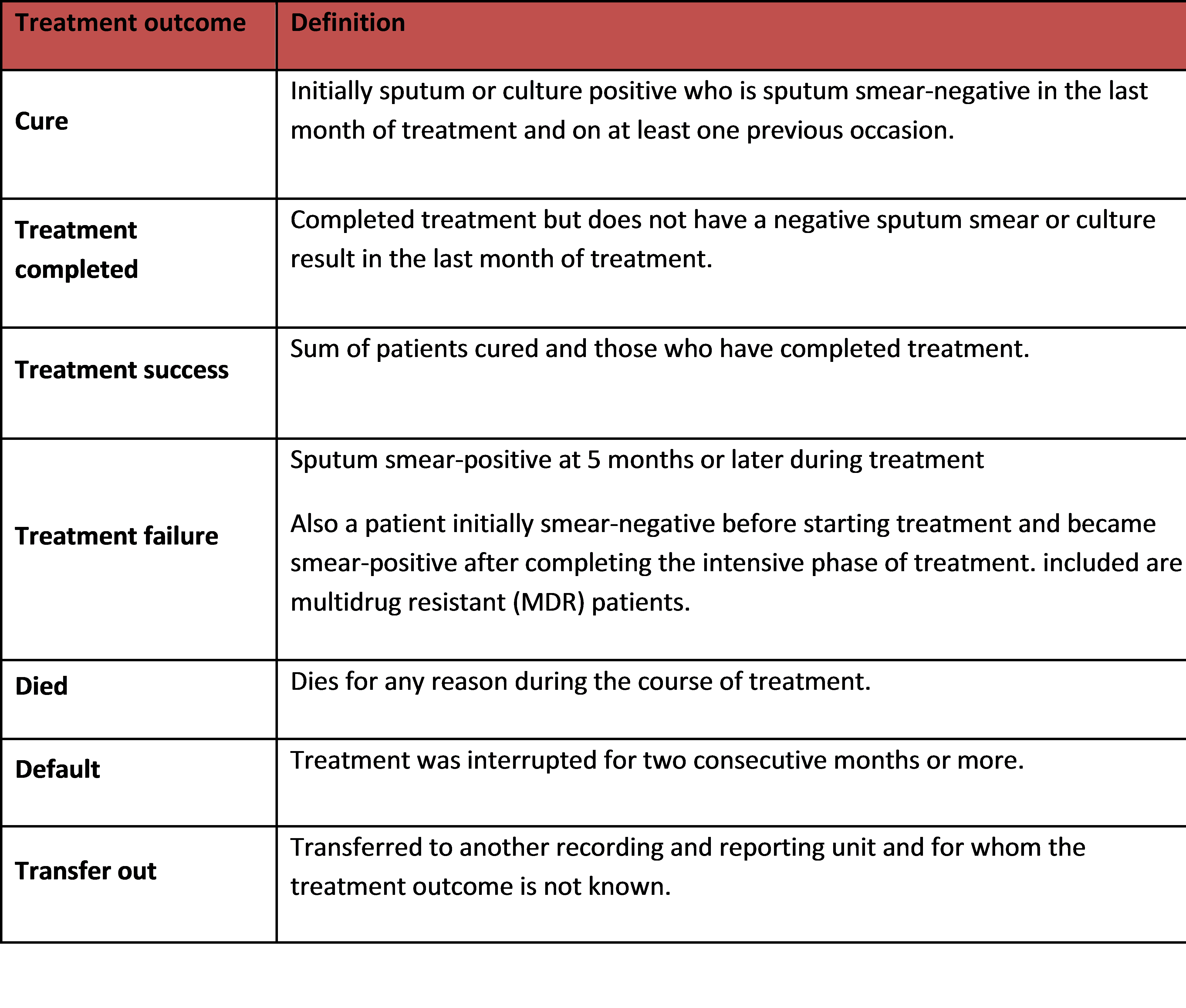
Types of Treatment Outcomes
-
TB Quarterly Notification Summary Form 100
-
TB Quarterly Outcome Report and TB/HIV Activities Form 102
-
Drug Abbreviations
TB treatment regimens are described using a standard code where each TB drug has an abbreviation.
The abbreviations for the drugs are:
-
First line anti-TB drugs: the drugs used in the standard regimens for new TB cases and retreatment cases:
- Rifampicin (R)
- Isoniazid (H)
- Pyrazinamide (Z)
- Ethambutol (E)
- Streptomycin (S)
Fixed-dose combinations (FDCs) are tablets that contain 2, 3 or 4 different anti-TB drugs in the appropriate strengths.
-
Second line anti-TB drugs: the drugs used in regimens for drug and multidrug resistance TB cases (MDR: resistance to at least isoniazid and rifampicin), the most frequently used are:
- Kanamycin (Km)
- Amikacin (Am)
- Capreomicin (Cm)
- Levofloxacin (Lfx)
- Ofloxacin (Ofx)
- Moxifloxacin (Mfx)
- Ethionamide (Eto) / Prothionamide (Pto)
- Cylcoserine (Cs)
- Para-aminosalicylic acid (PAS)
-
First line anti-TB drugs: the drugs used in the standard regimens for new TB cases and retreatment cases:
-
How to Read the Drug Code
-
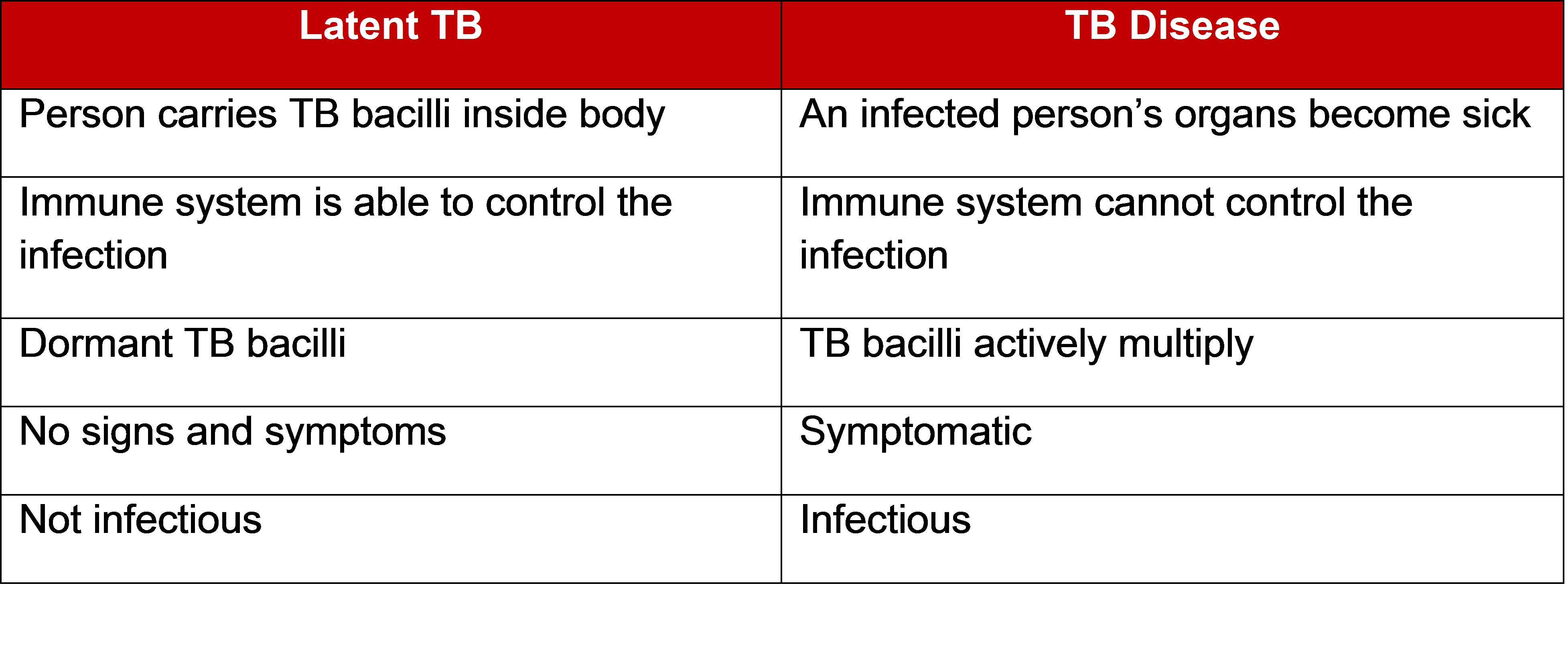
Difference Between Latent TB Infection and TB Disease
-
Treatment Categories and Regimens
-
Type of TB Cases
-