Session 1: Introduction
In this sessidon, we’ll start by looking at the context of HIV in Zimbabwe, then discuss monitoring our clients with HIV. We will also cover how HIV progresses in the body and why viral load is the gold standard for monitoring clients on ART. Finally, we’ll learn about UNAIDS 90-90-90 targets and how Zimbabwe plans to meet those targets.
Learning Objectives
By the end of this session you will be able to:
- Describe the context of HIV in Zimbabwe and the 90-90-90 treatment target to help end the AIDS epidemic.
- Describe the ways of monitoring patients on antiretroviral therapy.
- Discuss the goal of viral load monitoring.
- Describe strategies for implementing viral load monitoring.
- Explain what patient education is needed for viral load testing.
Learning Activities
-
Quiz: Pretest (10 min)
-
Reading: HIV in Zimbabwe (10 min)
In Zimbabwe, the number of people living with HIV (PLHIV) can increase for two reasons:
- More people are surviving HIV because they are on ART
- People continue to contract HIV
For more information, see Zimbabwe Factsheet, the Zimbabwe Population-based HIV Impact Assessment (ZIMPHIA) in the resources section.
Tap on each tab to read some statistics of HIV in Zimbabwe.
Prevalence
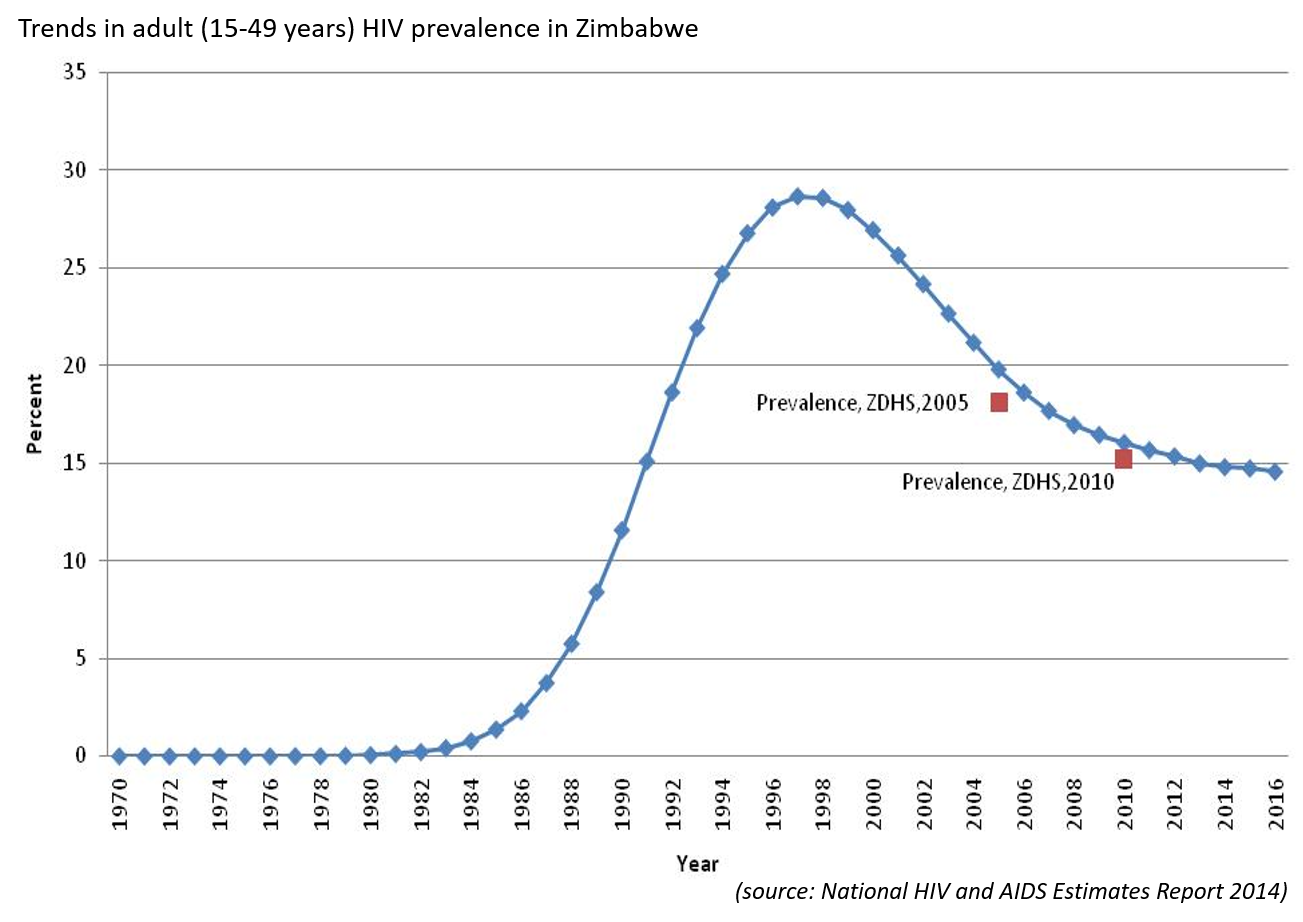
As we can see from this figure(tap on the figure to enlarge), the prevalence rose steeply from 1984, reaching a peak in 1996. After 1996, the prevalence of HIV might have decreased due to a decrease in transmission and new infections mainly due to behaviour change,or to deaths. Since 2010, the prevalence has plateaued, because more people with HIV have access to ART and are living longer. They are also less likely to transmit the virus to their contacts (Treatment as Prevention (TasP)).
Incidence
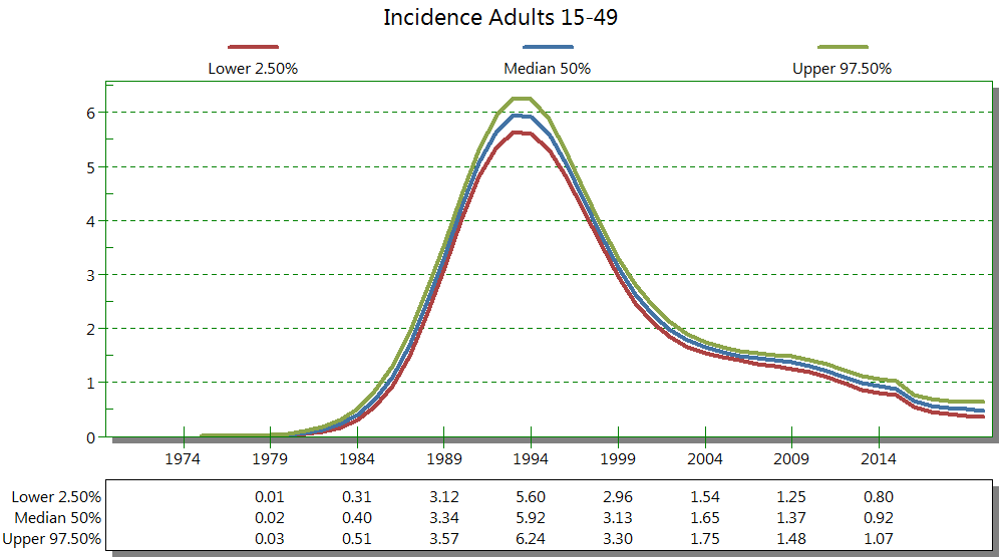
Let’s look at the incidence (or number of new cases) of HIV in Zimbabwe. In this second figure (tap on figure to enlarge), we can see that, like the prevalence graph, from 1984 the incidence of HIV was also increasing, and it peaked around 1994. Once ARV treatment was introduced and became more common, the incidence of HIV decreased. Currently, the incidence of adults 15-49 is around 0.5 because more people are on ART. This is due to using treatment as prevention (PReP, PEP) and prevention efforts through education on behaviour change, use of condoms, and voluntary medical male circumcision.
Population eligible for ART
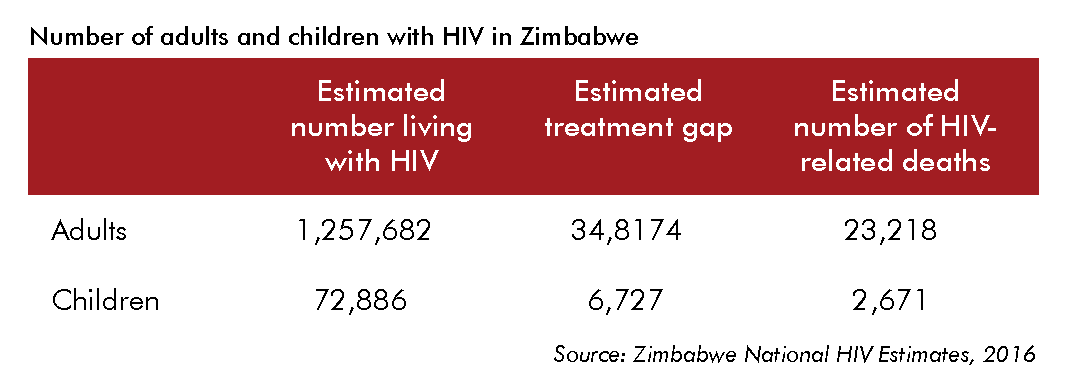
New national Guidelines for Antiretroviral Therapy for the Prevention and Treatment of HIV in Zimbabwe (December 2016) recommend a “treat all” approach, which means starting and keeping all PLHIV on ART no matter what their CD4 cell count or WHO clinical stage is at diagnosis. As we can see from this table (tap on table to enlarge), just over 39,000 children and almost 1,450,000 adults should be on ART. These estimates are higher than for 2013. We can also see that there are substantial deaths due to HIV that could be prevented with proper monitoring and ART.
-
Reading: Why Monitor? (5 min)
Monitoring HIV clients on ART is important to know whether treatment is successful or not, so that we can:
- Improve the client's health
- Keep them healthy
- Decrease their risk of developing resistance to medication
- Decrease their risk of vertical and horizontal transmission
Clients on ART should be monitored for both toxicity (side effects of drugs) and success of the treatment—that is, making sure that the drugs are not harming them and are working.
When we perform a test to monitor a client on ART, it’s not an end but rather the beginning of monitoring the client. We need to act on the result appropriately through correctly interpreting results and by helping the client understand what it means so that he or she will adhere to the treatment plan.
-
Reading: Types of Monitoring (10 min)
Tap on each category to read more about the different types of monitoring.
Clinical
In clinical monitoring, we rely on what the clients tell us (symptoms) and what we observe (signs). If they have opportunistic infections, we can then classify the HIV by stage (1, 2, 3, or 4). Ideally, we don’t want our clients to move to a higher stage than when they started. In other words, we don’t want them to become worse.
Immunological
In immunological monitoring, we assess damage to and response by the immune system to the ART medication the client is on. We track this by collecting blood to measure CD4 cell count, because the CD4 cells are responsible for detecting and attacking HIV in the body. CD4 cells also help other immune cells fight infection. Therefore, the lower the CD4 cell count, the more damage there is to the immune system. We don’t want the CD4 cell count dropping when clients are on ART.
Virological
In virological monitoring, we test to see the amount of the virus in the blood. This test is very accurate in providing early detection of whether ARVs are working. If the medication is working, we would expect the viral load to be suppressed, making it undetectable. If viral load isn’t suppressed, we would suspect that the client isn’t taking the treatment as directed (that is, adhering — we’ll talk more about this in session 3), or that the virus has developed a resistance to the medication (we’ll talk more about this in session 4).
-
Quiz: Monitoring (5 min)
-
Reading: Progression of HIV (10 min)
It’s important to know the natural progression of HIV so that we know the best way to monitor our clients. Review the images and read below to learn about the progression of HIV in people who are and aren't on ART.
Let’s first look at the progression in a person not on treatment. It’s helpful to understand what happens without treatment so that we can more easily understand what happens when a client is on treatment.
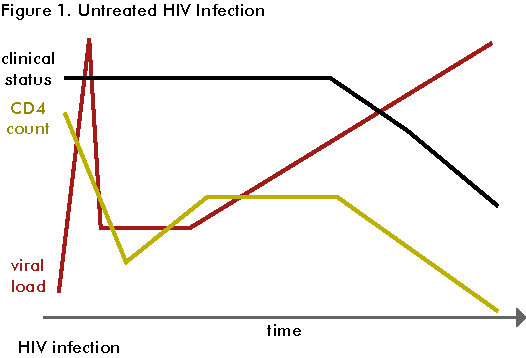
This first figure shows that when a person is infected with HIV, his or her viral load spikes immediately. Viral load is the number of viral particles found in each millilitre of blood. By viral particles, we mean the number of copies of HIV’s genetic material (RNA).
After several weeks, the viral load decreases, then plateaus and starts to increase gradually, spiking again after years.
Now let’s look at what the CD4 cell count does in a PLHIV who isn’t on treatment. Soon after infection, the CD4 cell count drops steeply. After several weeks, it increases and then stabilizes for a while. Finally, CD4 cell count starts slowly decreasing until it gets to 0. As the immune system gets weaker, OIs occur more frequently.
Clinically, a PLHIV not on treatment will have acute HIV syndrome soon after infection and then go into clinical latency for several years until he or she develops OIs.
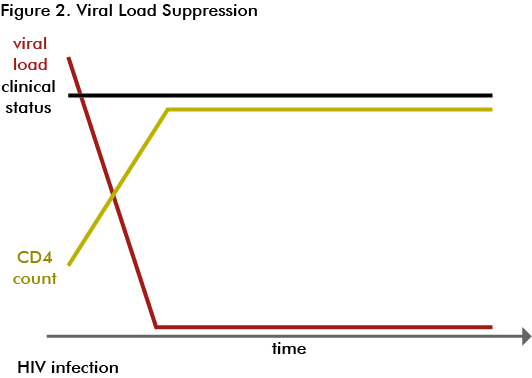
This figure shows what happens to the progression of the disease when a person starts treatment.
After a person is started on treatment, his or her viral load will decrease, followed by an increase in the CD4 cell count. If the client adheres to his or her treatment, he or she will remain healthy. If the client starts having poor adherence to treatment or if there is drug resistance, his or her viral load will increase, the CD4 cell count will decrease, and the client will develop OIs.
-
Reading: Which Test to Use (10 min)
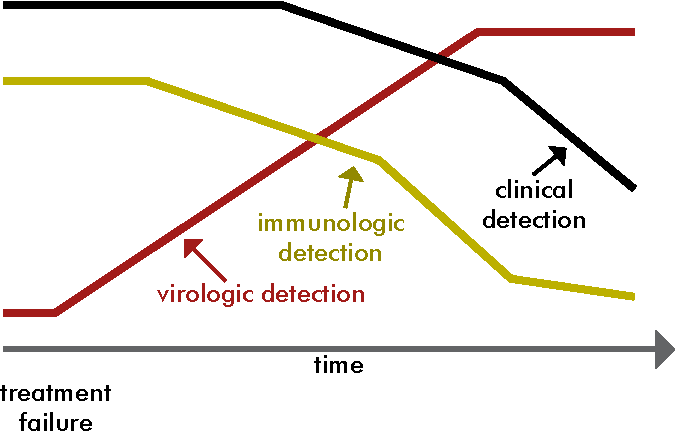
Is it better to monitor a client by looking at his or her viral load or CD4 cell count? When we conduct viral load tests, we are counting the number of copies of the virus per millilitre of blood, quantifying the actual amount of the virus in the body. Whereas when we test CD4 cell count, the results show the level of immunologic damage caused by virus, which we can use as a proxy to see the level of infection.
Let’s say that the graph shown below shows a hypothetical client, Tanaka’s, treatment failure (due to lack of adherence or drug resistance). The moment treatment starts to fail, his viral load increases (red line). But it takes a while for his CD4 cell count to start dropping (yellow line). It takes even longer for treatment failure to show up clinically (black line). So, we can see that if we monitor Tanaka’s viral load rather than his CD4 cell count or clinical picture, we can detect treatment failure earlier.
-
Quiz: Knowledge Check (5 min)
-
Reading: Achieving 90-90-90 Targets (10 min)
Monitoring VL not only helps our clients, but also helps us meet national and international goals for dealing with HIV. Tap on each circle of an image adpated from AVERT to read aabout UNAIDS’ set of “90-90-90” targets to help stop the HIV epidemic by 2020.
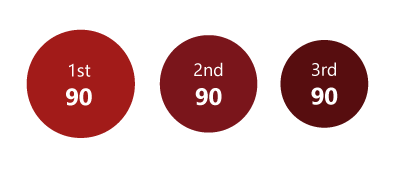
90% of all people living with HIV should
know their status, which is different than 90% should be tested.Out of the 90% who are diagnosed with HIV,
we want 90% of them to be on sustained ART.Out of 90% of people on sustained ART,
we want 90% of them to have a suppressed viral load.
We need to monitor viral load in our clients
so that we can reach the last “90” target.The Ministry of Health and Child Care (MoHCC) of Zimbabwe has a scale-up plan for rollout of viral load monitoring in the country. Their aim is to have universal access to viral load monitoring by end of 2020. The following activities need to happen so we can achieve this goal:
- Lab infrastructure must be up to date and up to scratch with functional electricity and machines.
- Procurement and supply chain must meet the needs of the clients, and commodities must be readily available.
- Transport should be available and reliable to carry samples from the site to the lab and carry the results from the lab to the site
- Data management systems must be in place to record the results and enable providers to act on that data.
- Education of PLHIV must be undertaken, so that they know what the test is for and are encouraged to ask their clinicians for it. Education will need to be intensified for clients who are newly diagnosed with HIV or who have just started ART.
- Training of healthcare workers so that they know which samples to collect, which tubes to use, and how to interpret and act on the results.
- Making sure the tests that are being done are the best quality for patients to receive accurate results (quality assurance).
- Programme management should ensure that the system is working and that the targets can be reached.
- Monitoring of the number of clients being tested and their results and evaluating the programme to see if it is working well.
The MoHCC Viral Load Scale Up Plan for Zimbabwe was created in 2014 and revised in 2018 with the following targets:

The plan has three main objectives designed to assist in accelerating the scaling up of viral load testing.
- Provide a roadmap to guide viral load testing scale-up in Zimbabwe from the 3% in 2014, when the plan was developed to 40% by the end of 2018, and 90% by 2020.
- Establish collaboration and coordination between government and partners as they scale up viral load testing in the country.
- Support resource mobilisation.
See the Zimbabwe HIV Viral Load Scale Up Plan in the resources section for more information.
-
Reading: Monitoring Strategies (10 min)
We’ve seen that monitoring VL is a better way to measure the response to ART, and that it helps us detect virological failure earlier than if we were to do immunological or clinical monitoring. By knowing our clients’ viral load results, we can address any issues, such as adherence, early. VL results can also indicate whether further tests are needed (such as HIV resistance testing or genotyping).
There are two VL monitoring strategies: targeted or routine. Tap each strategy to read more about it.
Targeted
Targeted viral load monitoring is done in settings where there isn’t access to routine viral load monitoring. We perform targeted monitoring for clients presenting with clinical or immunological failure after being on treatment for at least six months. Clients who experience any of these signs or symptoms should have targeted monitoring:
- New WHO stage 2, 3, or 4 with OIs
- A 10% drop in weight
- Recurrently unwell
Routine
In routine viral load monitoring, once a client has started ART, we would test his or her viral load at months 6 and 12 and then yearly afterwards. Routinely checking viral load is the monitoring strategy of choice in Zimbabwe.
We would also test viral load whenever we suspect clinical or immunological failure. This monitoring is considered targeted monitoring within routine testing because it’s based on whether the client is experiencing problems.
-
Self Reflection (10 min)
Take a few minutes to think about how your facility is doing with achieving the 90-90-90 targets. What challenges are there in meeting this last “90” target? In your role, are there things you might be able to do to support successful VL rollout? Feel free to jot down your ideas in your workbook.
-
Reading: What Is Undetectable Viral Load and Why Is It Important? (10 min)
A target not detected (TND) or undetectable or suppressed viral load occurs when copies of HIV can’t be detected by standard viral load tests. All viral load tests have a cut-off point below which they can’t detect HIV. This is called the limit of detection. For example, the level for Biomerieux is <182 copies/mL for DBS, and <100 copies/mL for plasma. In comparison, Roche has a lower limit of detection of <20 copies/mL. For clinical interpretation, the lower limit of detection does not make a difference as long as it is <1000 copies/mL.
The aim of HIV treatment is to reach an undetectable viral load, which usually occurs after three to six months of treatment with good adherence.
Note that viral load only gives an indication of the amount of HIV in the blood and doesn’t measure how much of the virus there is in sanctuary sites (brain and genital organs) where the effect of the drugs may vary. So, someone with an undetectable viral load hasn’t been cured of HIV; it’s still hiding in the sanctuary sites (such as the central nervous system and the testes).
-
Reading: Using Algorithms to Monitor Viral Load (10 min)
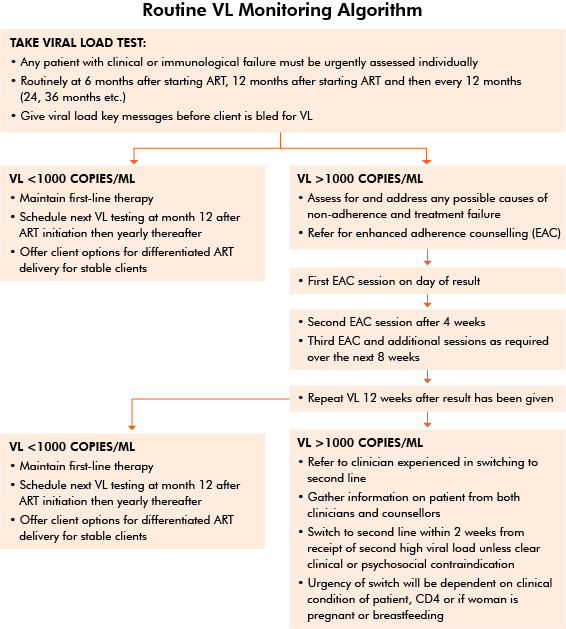
The MoHCC has created algorithms to guide health care workers on when to test a client’s viral load and what action to take based on the test results. The first algorithm, Algorithm for Routine Viral Load Testing, is designed for working with HIV-positive adults. The second algorithm is specifically for HIV-positive pregnant women. We’ll discuss the latter algorithm in session 5.
Let’s look at the Algorithm for Routine Viral Load Testing (tap to enlarge image). It starts by indicating when we should take a viral load test:
- Any patient with clinical or immunological failure (which we’ll cover in more detail in session 4) must be urgently assessed.
- Routinely at 6 and 12 months after starting ART and then every 12 months thereafter (24 months, 36 months, etc.)
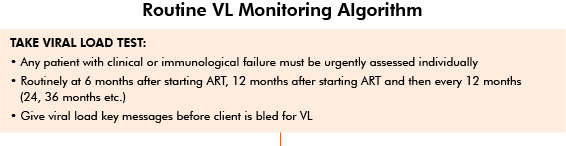
The algorithm also says that before we take the viral load test, we should educate the client about viral load monitoring and reinforce the importance of adherence.
We’ll continue discussing the algorithm in detail in session 3 when we cover interpretation of results and how to manage clients based on those results.
-
Reading: Patient Education (15 min)
Let’s discuss patient education in the context of VL. Most of us have been using the CD4 cell count results for tracking how clients are doing on ART. Now we need to educate clients on why VL testing is important—how it helps us monitor their response to treatment. The goal is to empower clients to request VL tests and understand the results.
There are several good resources to help educate clients on VL. The Patient Education on Viral Load Monitoring pamphlet explains why the test is important, how often a client should have the test taken, and what the results mean.
Different components of patient education will be covered throughout the training. For this session, let’s look at the importance of adherence and how viral load monitoring is used. This content is excerpted from the 2016 Viral Load Community Sensitisation Package (the full package can be found in the resources):
First, we need to educate clients about adherence. Clients should know that "for ARV treatment to work, it is very important that PLHIV take their medication every day, at the same time and as prescribed by their health care provider. This is called adherence, which is the most important factor that determines the success of taking HIV treatment. Adherence to an HIV regimen gives HIV medicines the chance to do their job: to prevent HIV from multiplying and destroying the immune system. ARVs should be taken every day as close to the same time as possible."
Poor adherence occurs when a client takes their pills too late, when a client forgets to take a dose, when a client does not take all their pills, or when a client stops taking treatment. Poor adherence may also be caused by health system issues, such as irregular availability of ARVs at your clinic. Currently, Zimbabwe has enough ARVs for everyone who is enrolled on ART.
We should tell our clients about the consequences of poor adherence, which include:
- Getting sick:
- If a client does not take their ARVs every day at a chosen time, they will not have enough ARVs in the blood to fight the HIV.
- The client’s viral load will be high meaning HIV is multiplying again and will be destroying the CD4 cells. This means the client cannot fight off illness and will get sick.
- Developing resistance:
- If the level of the ARVs in the blood is too low, the virus is able to transform itself and will start to multiply again. This means the HIV virus has become resistant and that the ARVs are no longer able to work to attack HIV.
- Transmitting HIV to a child or partner:
- If the viral load is high, meaning there is a lot of HIV in the blood, there is a much higher chance of passing HIV to one’s baby during pregnancy, delivery or breastfeeding.
- The chance of infecting one’s partner with HIV through unprotected sex is also a lot higher.
If a client does not take their ARVs every day at a chosen time, the client will not have enough ARVs in their body to stop HIV from multiplying. This will reduce the number of CD4 cells to fight off infections in their body. If the level of ARVs in the client’s body is too low, HIV is able to transform itself and will start multiplying again. This means that the HIV has become resistant to the ARVs the client is taking.
Next, we need to educate our clients about what viral load is. Clients should know that:
HIV viral load is the measure of the amount of HIV in a sample of blood. A viral load may be high or low. Viral load (VL) testing is the gold standard in Human Immunodeficiency Virus (HIV) treatment monitoring and ensures timely monitoring of treatment adherence and efficacy. It can be used to diagnose and minimise treatment failure in those on ART. This approach aims to ensure early indication of when enhanced adherence support is needed and when a person needs a treatment switch. Use of VL testing will prolong the use of first-line regimens, preventing drug resistance from developing, and thus ensuring the longevity of treatment programmes globally. Advantageously, it also requires that clinicians see patients less often because treatment monitoring can be simplified to an annual clinical visit for those who are virally suppressed, reducing visit burden on both patients and healthcare workers.
A viral load test measures the number of viruses in a person’s blood. The test is done by taking a sample of blood and having it processed in the lab.
Then we need to explain why testing for viral load is important. Clients should know that “doing a viral load test helps Health Care Workers to find out whether someone’s treatment is working or not (monitoring treatment success) and diagnosing treatment failure early.
Clients should also know when viral load tests should be taken. Explain that “the first viral load will be taken at 6 months after ART initiation and then again after 1 year on treatment, and after that yearly, as part of the routine follow up of HIV+ patients on ART. If there is a problem with someone’s viral load, it is taken again 3 months later (although there are exceptions to this, such as during pregnancy). During those 3 months the HIV+ individual will be working on their adherence with a counsellor and or treatment buddy and clinician.
- Getting sick:
-
Quiz: Knowledge Check (5 min)
-
Case Study: Isaac and Rumbi (10 min)
Isaac and Rumbi have been married for 15 years. Isaac is 39 years old and a farmer, while Rumbi is 34 years old and has a tuck shop that she manages with the help of their teenage son. Isaac and Rumbi do not have any significant medical problems and aren’t currently taking any medication. Isaac has been treated in the past for an STI. He doesn’t remember what medication he was given, but he remembers taking it for about a week.
Recently, there have been community health programmes in their rural area in Hurungwe District, Mashonaland West Province specifically aimed at farmers and their families. The next programme will discuss HIV and there will be HIV testing.
Rumbi attended a similar programme a few months ago when Isaac was away. She left before getting the test done. She wants to get tested at the next programme and wants Isaac to come with her and be tested. Initially he told her he was too busy, but she insisted.
Rumbi has been concerned about Isaac’s health for a long time. Several years ago, Isaac decided that he couldn’t support his family on just the income from farming, so took a job as a truck driver. Rumbi has tried to keep up with the farm work in addition to running the tuck shop. After about a year, she told Isaac that he had to stop driving.
While he was a truck driver, Isaac returned home every 4-6 weeks. While he was home, Isaac would often drink many beers, telling Rumbi that driving a truck was very stressful and he needed to relax. One time when he was home, Rumbi found condoms in his pockets. She asked him if he was having sex. He became very angry and denied it, but Rumbi always felt that Isaac wasn’t telling the truth, and this has been troubling for her.
In September, Isaac and Rumbi attend the community education programme on HIV and agree to get tested. They decide to receive their test results together. Rumbi is relieved to hear her results are negative, but shocked to learn that Isaac’s results are positive. Isaac insists that the results are wrong. They are referred to Kazangarare Rural Health Centre for repeat testing and the results are confirmed.
The adjustment to their discordant status has been difficult. Isaac hesitated going back to the clinic after the confirmatory test and didn’t begin EFV/3TC/TDF = FDC until 06/Dec/2016—several weeks after his HIV diagnosis. He became very depressed. Rumbi has many questions about why he is positive and she hasn’t been infected.
Isaac has been followed monthly at the clinic and, according to his clinic record, his adherence has been documented as “good”—between 93 – 96%. There were two occasions when he forgot to bring back the pill container, but didn’t report any missed doses. Today is his five-month clinic visit.
Isaac arrived late for his month five appointment and was very anxious to “get his pills and get back to work”. He forgot his pill container and when asked about any problems since his last visit he became angry “You ask me the same questions every time I come here and I give you the same answers. If I had any problems I would tell you!” Isaac’s behavior is unusual. He’s normally quiet and answers questions in one or two words. You notice a faint smell of alcohol on his breath.
You tell him that at next month’s visit, you’ll be taking a blood test that will show how well the medication is working. Isaac responds that he can’t come to clinic every month. He wants a two-month supply of medicine and asks if the blood test can be done when he is back.
Isaac leaves the clinic with a one-month supply of medication and his next appointment scheduled for 29 days since there is a holiday that falls on the day 30. He is visibly upset but agrees to come back on time if future appointments can be every other month.
We’ll continue with Isaac’s story in session 2.
-
Reading: Summary (5 min)
Summary
In this session, we discussed the current prevalence of HIV in Zimbabwe. We then looked at the importance of monitoring clients on ART and reviewed the three main types of monitoring — clinical, immunological, and virological. We also went through how HIV progresses in an HIV-positive client. Most important, we discussed why monitoring VL over CD4 cell count is a better approach to take, as it detects failure earlier, indicates whether further tests are needed, and helps us to meet the UNAIDS’ 90-90-90 targets. We also talked about the importance of undetected VL and how to use the algorithm to test HIV-positive clients. Finally, we read the recommendations on how to educate clients regarding the importance of medication adherence and VL testing, including what’s involved in VL testing and how often it should be conducted.
-
Quiz: Posttest (10 min)
