Session 3: Results Interpretation & EAC
This session we’ll talk about how to interpret viral load test results, how to manage clients based on those test results, and how to conduct enhanced adherence counselling (EAC).
Learning Objectives
By the end of this session you will be able to:
- Explain what a suppressed viral load result means.
- Explain what a viral load that is over 1000 copies/mL means.
- Describe possible causes for high viral load.
- Describe the approach to addressing an unsuppressed viral load with client.
- Explain the importance of enhanced adherence counselling and how to conduct it.
Learning Activities
-
Quiz: Pretest (10 min)
-
Reading: Interpreting Test Results (10 min)
Before we cover interpreting results, let’s first describe what to do upon receiving the test result. First, pull the client’s file and document the result in the VL column of the patient care and treatment book. For facilities who have EPMS, enter the results in the client’s record as well. After the information has been added, file the hard copy of the result in the client’s green book at the back (you can staple them in).
Once these steps have been completed, you can begin to interpret each viral load test result by taking into consideration all previously recorded test results. It’s important to look at the results together to see changes over time.
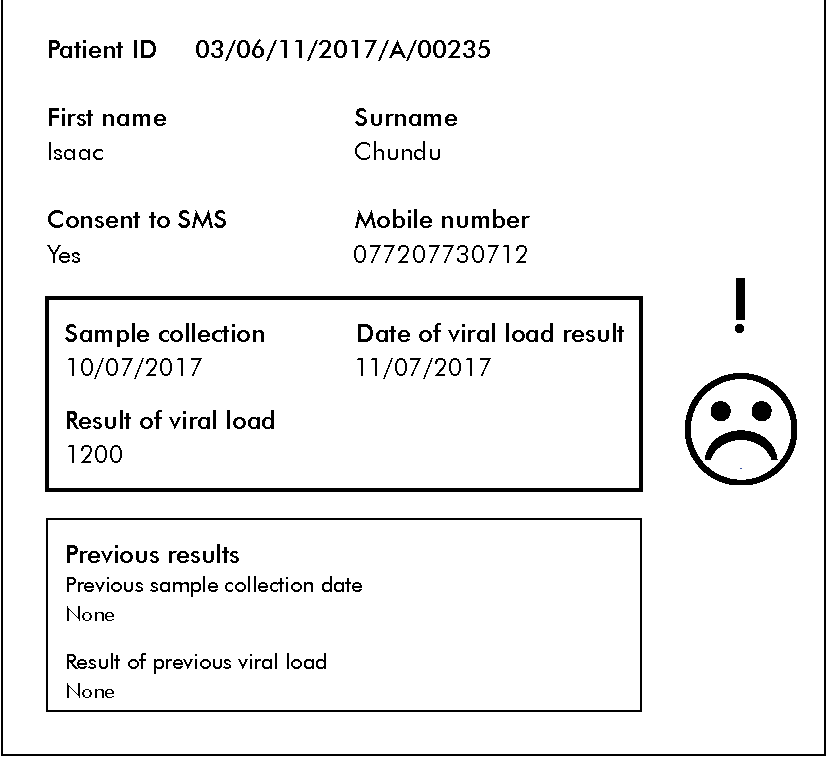
Tap on each area on the results form to read about how to interpret test results.

Clinic code:
Ask for this info from CEs of ZIM
Barcode number:
Note that the barcode number (that you affixed to the sample) will appear here.
Patient ID and name:
The patient ID and name from the request form.
SMS
If we indicated that the client consented to be contacted by SMS, the number will be included here. If the client didn’t consent, it will say no and no mobile number will be included.
Current results:
The date the sample was collected (which is pulled from request form), the date of the VL result, and the result shows in this box. If the VL is < 1000 copies/mL, a smiley face appears. If the VL is > 1000 copies/mL, a frowny face and exclamation point will appear.
Previous results:
The client’s previous VL test result will appear here.
-
Reading: Managing Clients With Viral Load < 1000 Copies/mL (10 min)
The aim of HIV treatment is to reach an undetectable viral load. This is usually after three to six months of treatment with good adherence. Having an undetectable viral load is important for a number of reasons:
- The immune system will be able to recover and become stronger.
- It lowers the risk of becoming ill.
- The risk of HIV becoming resistant to ARVs is very low.
- It reduces the risk of passing on HIV to someone else.
So, what is an undetectable viral load (also known as target not detected, or TND)? All viral load tests have a cut-off point below which they can’t reliably detect HIV. This is called the limit of detection. Most tests used have a lower limit of detection of 40 or 50 copies/mL, but there are some very sensitive tests that can measure below 20 copies/mL.
However, just because the level of HIV is too low to be measured doesn’t mean that the virus has disappeared completely from the host (that is, the person with HIV). The virus may still present in amounts too low to be measured. The tests measure levels of HIV only in the blood. The virus may be hiding in sanctuary sites (the brain, genital fluids, gut, or lymph nodes).
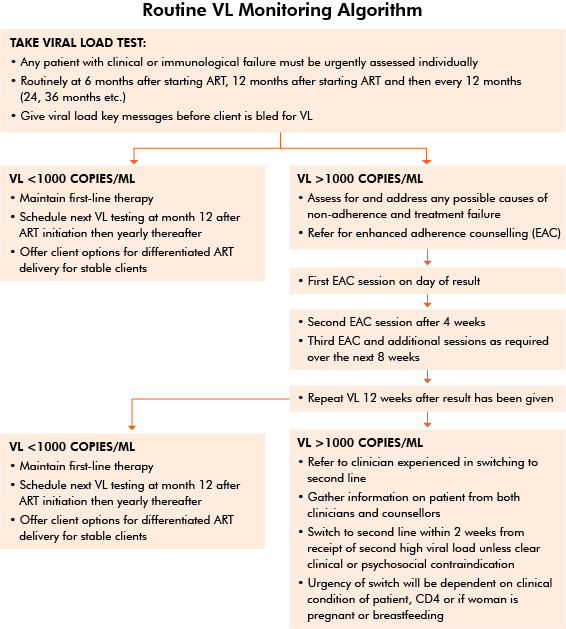
Let’s use the Algorithm for Routine Viral Load Testing to learn how to manage clients based on their test results. Note that we will cover a different algorithm in session 5 for Pregnant and Lactating Mothers.
When a client has an undetectable viral load, it’s important to congratulate him or her, provide reinforcement counselling to keep him or her on the right track, explore any barriers that may be ahead, and discuss ways that help can be provided.
From the program-level view, viral loads below 1000 show that the virus is under control. At an individual level, the goal is for clients to have an undetectable viral load. For example, if a client has a viral load of 200 copies/mL of blood (which is still detectable), that client would need adherence counseling with the goal of reaching an undetectable viral load.
According to the algorithm, we should have the client maintain first-line therapy. The client should have viral load testing at six months after starting on ART and then yearly thereafter. For stable clients, we can offer differentiated ART delivery.
-
Reading: Differentiated ART (10 min)
Differentiated ART is a component of differentiated service delivery, which is a client-centred approach that provides HIV services based on the preferences of different groups of people living with HIV while not placing added burden on the health system. Differentiated ART delivery is still being developed in Zimbabwe and not all facilities will be able to provide this yet.
Clients in different districts may have different challenges, so the OSDM provides a decision framework for differentiated ART delivery that can be tailored to the needs of clients in a particular district.
Not all clients are eligible for differentiated ART. Clients must be stable on ART (first- or second-line). Where VL testing is available, stable clients are defined as:
- Having no current OIs
- Having a VL of < 1000 copies/mL
- Being on their current regimen for at least six months
Where VL testing isn’t available, stable clients are defined as:
- Having no current OIs
- Having a CD4 cell count of > 200 cells/mm3
- Being on their current regimen for at least six months
Before starting clients on differentiated ART, you should conduct a psychosocial assessment to ensure that clients can handle being on differentiated ART.
There are several options for ART refill under differentiated ART.
Fast Track
With the fast track option, clients get their refills directly from the dispensary and don’t need to see a clinician. This option provides more convenience to the client, since he or she can collect the medication any time during the day that the dispensary is open on the day the refill is ready.
Club
This option allows clients booked for refills on the same day to get their medication as a group. A health care worker meets with the group to discuss any issues people may be having and then distributes the medication.
Outreach
For clients who live in remote areas where access to HIV facilities is difficult or in areas where outreach activities are already happening, this option may be a good solution. A nurse, primary counsellor, or an expert client delivers medication refills to a fixed outreach site.
Community ART Refill Groups (CARGs)
CARGs are self-formed group of clients, usually from the same geographical area. All members go to their clinic visits and get routine testing at the same time as a group. The group nominates one member to collect the medication from the facility and distribute to the rest of the members.
Family Member Refills or Family ART Refill Groups (FARGs)
This option is somewhat similar to CARGs. If several family members are on ART, one member collects the refills for the others.
Be sure to read Chapter 2.5 on differentiated ART in the Zimbabwe Operational and Service Delivery Manual, (included in the resources), to learn more. You should also find out what’s available at your own facility.
-
Quiz: Terms (5 min)
-
Reading: Managing Clients With Viral Load > 1000 Copies/mL (10 min)
For clients with unsuppressed VL, their files should be pulled and identified as high VL (that is, flagged with a red sticker or any other method used to flag high VL files at your facility). Unless the client is attending within the next two weeks, the client must be traced and asked to come to the clinic as soon as possible. The client may be phoned or traced via a community health worker. The community health worker should use the bi-directional referral tool to make sure the referral is complete and the client has received appropriate service at the facility.
If a client’s VL hasn’t fallen to undetectable levels (that is, it is unsuppressed) after six months of starting HIV treatment, we should first assess and address any possible causes of non-adherence and treatment failure before making any changes to the client’s treatment regimen. No client should be switched to second-line ART on the basis of one high viral load above 1000 copies.
At that appointment, start enhanced adherence counseling (EAC) sessions, involving both the counsellor and the clinician. Document any findings in the green book and the EAC register.
Once adherence issues have been resolved after three months, repeat the VL test. If the new test results show < 1000 copies/mL, manage the client’s treatment the same way as we discussed previously. In session 4 we’ll cover how to manage a client if his or her VL continues to be < 1000 copies/mL even after enhanced adherence counseling.
-
Reading (Nice to Know): Using Log Values to Measure Viral Load (10 min)
A log value is a measurement frequently used to describe the measurement of HIV viral load. It expresses the VL values as a power of ten (written log10). A log is a number multiplied to the power of 10. This scale is used because it turns large numbers of copies/mL into more manageable figures.
Changes in the amount of HIV in the blood can be referred to as either a 10 times increase or decrease log change.
For example, a decrease in viral load from 40,000 to 4000 copies/mL could be described as a one-log decrease, a tenfold decrease, or a decrease of 90%.
A decrease in viral load from 40,000 to 400 copies/mL could be described as a two-log drop (102), equivalent to a hundredfold fall, or a decrease of 99%.
And a decrease in viral load from 40,000 to 40 copies/mL would be a three-log drop (103), equivalent to a thousandfold fall, or a decrease of 99.9%.
With 95% or greater adherence to ARVs, the VL will quickly decrease within the first few days of starting medication. Over time, the decrease will continue, although at a slower pace. If the client has an opportunistic infection or a very high amount of the virus, the decrease may take longer until the level is undetectable. Even though we don’t check VL until six months after initiation, it’s estimated that the VL will decrease by 1 log within the first month. When checked at six months, it’s expected that the VL will be < 1000 copies/mL, or undetectable.
Variations of < 0.5 log (3 fold) isn’t clinically significant. For example, let’s say we have a client who has a VL result is 200 copies/mL at six months and a VL result of 635 copies/mL at 12 months. This doesn’t necessarily mean that the client is beginning to experience treatment failure. The next viral load result at 24 months should continue to be < 1000 copies/mL, indicating that the medications are working. It’s important for providers to conduct a thorough adherence assessment at each visit to ensure continued ART success.
There are several factors we must take into account that may affect the viral load results. These include laboratory variation, assay fluctuations, and client factors, such as if a client has an acute illness or has recently receive a vaccination. Each VL assay has specific characteristics. When comparing results, it’s important to make sure that the test was done at the same laboratory.
-
Quiz: Log Values (5 min)
-
Reading: Assessing Causes of High Viral Load (10 min)
It’s important to identify the cause of high viral load results before switching clients to second-line therapy. When assessing the cause, we should first look at adherence issues.
Poor Adherence
Poor adherence is the most common reason for high viral load. If a client isn’t adherent to his or her first line regimen, then he or she likely won’t be adherent to the new regimen and will run out of treatment options. In most settings, we don’t have access to genotyping, so having one-on-one sessions to rule out adherence issues is helpful.
If we determine that poor adherence isn’t the problem (through pill counts and self report), we can assess whether there might be any medical issues causing high viral load.
Poor adherence can result in development of drug resistance leading to the need to switch to medications, which may cause new or different side effects (we’ll cover drug resistance and therapy switching in session 4). Furthermore, poor adherence is costly: not only can second- and third-line therapies cost more but also managing the side effects can also be more costly. Cost increases affect the community and country.
Medical Issues
If adherence is good but the client still has an unsuppressed viral load, we’d next investigate to see whether there are any medical reasons. Tap on each category to read more.
Opportunistic infections
Clients with a very low CD4 count are especially vulnerable to developing opportunistic infections. Acute or chronic GI conditions such as diarrhea can contribute to unsuppressed viral load results.
Drug absorption
Inadequate absorption, possibly caused by chronic diarrhea or vomiting, can also cause low blood levels. If you suspect that drug absorption may be the issue, refer to your mentor or a doctor.
Drug interactions
Drug interactions can cause low blood levels, which must be maintained at optimal concentrations to be effective against HIV. If blood levels are low, this can result in a high viral load. For example, rifampicin, a common treatment for tuberculosis, has a negative interaction with ARTs, making them less effective. In these circumstances, the client might need to change drugs or change dosages of ARTs. This isn’t a reason for switching to a new regimen. If you suspect that drug interaction may be the issue, refer to your mentor or a doctor.
Drug Resistance
After verifying that poor adherence and medical issues aren’t causing the high viral load, we should recheck the client’s viral load to make sure that there wasn’t an error with the previous test result. If the viral load is still high, we should consider whether the client has developed a resistance to the medications. Drug resistance can lead to a client becoming resistant to not only the ARVs the client is currently taking, but also to similar ARVs. We’ll talk more about drug resistance in session 4.
-
Reading: Enhanced Adherence Counseling (10 min)
Enhanced Adherence Counselling (EAC)
The goal of EAC is to assess a client’s barriers to adherence and identify and evaluate strategies to overcome those barriers.
Before we cover EAC, let’s briefly review basic adherence counselling. Before clients start on ART, they receive basic adherence counselling (usually in a group setting). Counselling includes educating clients about what HIV is, what it does to the body, and how treatment can keep them healthy.
Clients undergoing EAC have already had the basic adherence counselling. Basic adherence counselling provides general information, whereas in EAC, information is tailored to each client and conducted in three one-on-one sessions over a period of three or more months. Each monthly session lasts about 15 minutes. At the end of the three months, if the client has had good adherence, we should test his or her viral load. If adherence isn’t good during the initial three months of EAC, we’ll have to continue providing EAC to help the client have good adherence before retesting the client’s viral load.
When we conduct EAC, we want to get an in-depth understanding of the client’s situation. What problems are the client experiencing that prevents adherence? Is there anything missing from the education the client received that could help him or her understand the importance of taking ARVs? What barriers do he or she face? Once we know the answers to these questions, we can help the client figure out ways to overcome these barriers. We also need to educate the client about viral load, the importance of keeping it low, and how ARVs can do that.
Enhanced Adherence Counselling Sessions
Session 1
EAC begins on the day the client receives his or her result. At the first EAC session, we want to discover any possible behavioural, cognitive, emotional, and socio-economic barriers to adherence.
According to the Operational Service and Delivery Manual for the Prevention, Care and Treatment of HIV in Zimbabwe (OSDM) (page 78):
After presenting the result, the best way to start the session is to ask the patient:
What do you think is the reason for your high viral load?
In addition, exploring the client’s motivation for taking medication often highlights reasons for non-adherence. Clients with high viral load should also have a formal mental health assessment, including the use of alcohol and other substances of misuse.
See the CAGE questionnaire in Resources for a tool to screen for alcoholism.
Two simple screening questions may be asked:
- During the past month, have you felt like you were losing interest or pleasure in doing things?
- Have you felt down, depressed or helpless?
If there is a positive answer to either of these questions or if the client presents with red-flag issues (virological failure, missed appointments, challenging psychosocial issues), carry out a formal mental health assessment using a standardised tool, such as the Shona Symptom Questionnaire (see Appendix 3 in the OSDM). Clients should then be managed with ongoing counselling interventions or, where appropriate, referred for formal mental health assessment.
See the Session 1 guidance in the OSDM.
Session 2
The second session of EAC is given four weeks after the first, and is aimed at following up the strategies put in place during the first session to check if there are any difficulties on agreed plan and solve any new issues. Session 2 guidance is in the OSDM page 82.
Session 3 and up
The third session is given four weeks after the second, and is aimed at following up the strategies put in place during the first two sessions. If the client isn’t adherent to treatment after the third session, you will need to continue EAC. Use the session 2 guidance for sessions 3 and on, tailoring each session to the individual client’s needs.
In some cases the client may require more intensive adherence support. This should be provided on a case-by-case basis. With the client’s permission, they should be offered to link with a CHW or expert client in their home area who may be able to give additional adherence support in the community. Clients who are in group models may benefit from having other group members attend their EAC sessions with them.
The Consolidated HIV and AIDS Job Aide, in the resources, has an enhanced adherence checklist on page 139.
Be sure to use all the steps in the EAC session guides, which will help you address barriers and issues the client may be experiencing.
-
Reading: Patient Education (10 min)
It’s important that we educate our clients about what the viral load test results mean. Tap on the following questions to read about what talking points to use.
How do I know if I have a suppressed viral load?

A low or lower than detectable viral load is a viral load that is too low to be measured by the current laboratory tests. WHO set a viral load of less than 1000 copies/mL as normal for intervention purposes but the most desired result should be TND (Target Not Detectable). It means that a client has very little HIV in their blood. This is because the drugs they are taking are working well and the multiplication of the virus has been stopped by the ARV treatment. A low or lower than detectable viral load does not mean a client no longer has HIV. It just means it can hardly be measured with the tests we have.
How do I know if I have high viral load?

A high viral load is a viral load of more than 1000 copies/mL. It means that there is too much HIV in the blood. This is because the client does not have enough ARVs in their blood or the ARVs are not working. When this happens HIV is able to make more HIV in the body. The most common reason for this is when clients have problems taking their medication, also called poor adherence. By solving adherence problems early, a client’s viral load should be able to go down below 1000 copies/mL. A high viral load may also mean that the client’s current treatment is not working well and they may need to be switched to a different treatment regimen.
-
Case Study: Isaac (15 min)
In session 1 we met Isaac, a 39-year-old farmer who tested positive for HIV. In session 2, at month 6 (his last visit), he had a VL test. Today he’s back for his results.
Tap to enlarge Isaac’s viral load result.
Isaac returns to clinic on his scheduled day to get his results. He asks if he can have two months of medication. You explain the viral load result and following the discussion, Isaac asks you to give him medication that will work better than what he is taking now.
We’ll continue with Isaac’s story in session 4.
-
Case Study: Tari (15 min)
Tari is a 32-year-old school teacher who presented to the clinic with central chest pain when swallowing solid and liquid foods for the past two weeks. She has associated generalized body weakness and weight loss with no history of fever or cough. Prior to the problem with swallowing, Tari noticed a white coating on her tongue, which she treated with mouthwash from the pharmacy and herbal tea her sister gave her. She is not married, doesn’t have children, and lives with her sister. Tari thought she had picked up a virus from one of her students, so she tried to treat it at home but the pain and swallowing difficulty has worsened.
You are a new provider to this clinic. Tari is due for her six-month appointment today. You review the clinic notes. When Tari initially presented to the clinic, it was noted that she was chronically unwell. Her vital signs were in the normal range and she had small posterior cervical lymph nodes, extensive oral thrush, clear chest to auscultation, and no pertinent findings in the other systems.
Tari was tested for HIV, which came back positive. Additional laboratory tests showed
- Hb 8.2g/dL CD4 count = 32mm³
- VL = 106,328 copies/mL
- CrAg = negative.
She was given treatment for oral and oesophgeal candidiasis and started on EFV/3TC/TDF = FDC.
The first few weeks after initiating ART, Tari continued to have some difficulty swallowing and experienced poor appetite and occasional nausea. She admitted to missing a few doses, especially when she fell asleep early in the evening. Overall, her adherence in the past three months has ranged from 94 – 96%. She forgot to bring her pill container one month, but reported “no missed doses”.
Tari tells you that she remembers the nurse telling her something about the viral load test she is having today and using the letters TND. She asks you what is so important about having a result that is TND.
Tari’s viral load result was TND. She returned for her month seven visit and was told the good news. She was very happy, especially since she knew she would be receiving a three-month supply of medication and wouldn’t have to come to clinic every month. She tells you that her workmates have not been happy that she is taking time off or coming in late even though she told them it was for clinic appointments. She’s very worried that she may lose this job and she can’t risk this happening.
Tari returned her pill containers with three cotrimoxazole pills and three EFV/3TC/TDF pills. “I only missed one or two doses since I was here last month” Note: She was given a 30 day supply of medication at her last visit.
-
Reading: Summary (5 min)
This concludes session 3. This session we learned how to interpret viral load test results and how to use the algorithm to manage clients with a viral load of < 1000 copies/mL and >1000 copies/mL. We also discussed possible causes for a high viral load in a client. Then, we looked at causes for high viral load such as adherence or clinical issues. Next, we went over the goal of enhanced adherence counseling (EAC) and how to conduct this type of counseling. We wrapped up this session by addressing patient education and topics to cover when educating a client on viral load test results.
-
Quiz: Posttest (10 min)