
Vector-Borne Diseases
Table of Contents
Historical Background
Vector-Borne Diseases:Parasitic Diseases Bacterial Diseases Viral Diseases
Case StudiesPlague Dengue West Nile Encephalitis Yellow Fever
Factors Responsible for ResurgenceDemographic Changes Societal Changes Genetic Changes in Pathogen Changes in Public Health Climate Change?
Reversing the Trend
Historical Background
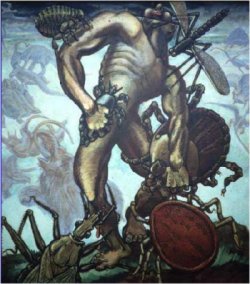 In
1973, while setting up a laboratory to work on vector competence of Aedes
aegypti for dengue viruses at Rocky Mountain Labs in Hamilton, I
found this beautiful oil painting. I call it "the scourge of mankind."
It illustrates that vector-borne diseases have truly been the scourge
of mankind from the beginning of time and, with their resurgence in the
waning years of the twentieth-century, continue to be so.
In
1973, while setting up a laboratory to work on vector competence of Aedes
aegypti for dengue viruses at Rocky Mountain Labs in Hamilton, I
found this beautiful oil painting. I call it "the scourge of mankind."
It illustrates that vector-borne diseases have truly been the scourge
of mankind from the beginning of time and, with their resurgence in the
waning years of the twentieth-century, continue to be so.
In the 18th and 19th centuries, vector-borne diseases were among the major public health problems that man faced throughout most of the world. By 1910 most of the major vector-borne disease transmission cycles had been worked out. The public health officials of the time used this information to implement highly successful vector-borne disease prevention and control programs. I have listed a series of successes:
- Yellow Fever - Cuba, 1900
- Yellow Fever - Panama, 1904
- Yellow Fever - Brazil, 1932
- Anopheles gambiae - Brazil, 1938
- Anopheles gambiae - Egypt, 1942
- Louse Borne Typhus - Italy, 1942
- Yellow Fever - Americas, 1947
- Malaria - Sardinia, 1948
- Malaria - Americas, 1954
- Malaria - Global, 1955
- Yellow Fever - West Africa, 1950s
- Onchocerciasis - West Africa, 1974
- Bancroftian Filariasis - South Pacific, 1970s
- Chagas disease - South America, 1900s
Unfortunately, success breeds failure. By the middle of the 20th century, certainly by the 1960s, most of these diseases had been effectively controlled. Plague epidemics, yellow fever, and dengue were no longer widespread and malaria had been effectively controlled in most parts of the world, except for sub-Saharan Africa. It initiated a period of complacency in the 1960s and 70s.
Sir Macfarland Burnett in 1962, declared that the war on infectious diseases had been won. The Surgeon General of the US, a few years later, made a similar declaration and set the tone for policy makers for public health officials and for the public; a period of complacency. The result was a dramatic lack of resources going into research and prevention control programs for vector-borne diseases in the 1970s, 80s, and 90s. The consequences of decreased resources and the elimination of programs in the last thirty years were decreased personnel trained to deal with vector-borne diseases in the waning years of the 20th century.
We have seen a dramatic resurgence of epidemic vector-borne infectious diseases in the past 20 years. We have seen a number of newly recognized diseases: Lyme disease and Ehrlichiosis, among others. Perhaps more importantly from a public health point of view, is the expanding geographic distribution and increased epidemic activity of these previously controlled diseases. This is what I want to focus on.
vector-borne Diseases: Parasitic, Bacterial, and Viral
Parasitic Diseases[SLIDE 1] If we focus on the last decade of the 20th century, we find that malaria is still the most important vector-borne disease of man. It occurs globally, though it doesn't often occur in major epidemics. African Trypanosomiasis and Leishmaniasis have also shown a dramatic resurgence in the past twenty years.
Bacterial Diseases[SLIDE 2] We have seen the emergence of Lyme disease and Ehrlichiosis in both the US, North America, and Europe. We have seen unique epidemics of diseases like Louse Borne Relapsing Fever and Louse Borne Typhus in Africa. Globally however, plague is still the most important vector-borne bacterial disease. It has the potential for major epidemics.
Viral DiseasesThe Arboviruses, the vector-borne viral diseases, eclipse everything else. You cannot go anywhere in the world without being at risk for some arboviral disease that has a potential for epidemic activity. Dengue is without question the most important and has a global distribution in the tropics. [SLIDE 3] The single points represent multiple epidemics. We have had localized outbreaks of yellow fever in Africa and in Latin America. We've also witnessed the emergence of Japanese Encephalitis and its geographic movement into West Asia and Australia. We have seen West Nile come into the Western Hemisphere. Arboviral diseases are without question, the most important in terms of epidemic diseases.
Case Studies
[SLIDE 4] Most experts on plague agree that the current world distribution of plague probably resulted from the last pandemic that began in the latter part of the 19th century. They think this is when plague was introduced into the US. This is probably when plague was introduced into India as well.
In the first twenty-five years of the 20th century from about 1900-25, an estimated 12 million people died from plague in India. The Indian health service implemented a very effective prevention and control program and by the 1950s and 1960s, plague was no longer a major public health problem in India. It created an atmosphere from 1960-1994 where very few people worked on plague. There was little research done and not much in the way of diagnostic testing.
The 1994 experience began in late September at the Division of vector-borne Infectious Diseases, CDC. We received a call in the middle of the night from the Regional Advisor for Communicable Diseases, WHO, at the Southeast Asia regional office in New Delhi. He was wondering where the plague reagents were that he ordered a couple of weeks ago. In fact, we had received an order of reagents from India from WHO, which was unusual for us, but there was no urgency attached to it so it was processed as a routine matter. He explained that there was a potential epidemic of pneumonic plague in the western city of Surat. [SLIDE 5] They had reported an outbreak of pneumonic plague in Surat. We responded by sending reagents. We also responded by sending two teams of researchers to India, one to work on the epidemiology/ecology of the disease and another team to work on the diagnosis of plague. Putting it altogether in retrospect, it appeared that the outbreak started in Maharashtra as an outbreak of bubonic plague. It was then brought to Surat during a holiday festival and started an outbreak there.
The initial clinical diagnosis was confused as the Indian physicians had not seen anything like this. They looked through their books and tried to find diseases that were compatible. They sent samples to New Delhi for laboratory diagnosis. The results were equivocal, and it created more confusion and a lack of confidence in the diagnostic and the epidemiologic capability. The press in India went wild and ultimately it caused public panic. There was speculation that this was biological warfare. It ended up really as an epidemic of panic rather than an epidemic of plague. Within a two-week period of time in late September and early October, an estimated 500,000 people fled the city of Surat and went to Dehli, Calcutta, Madras, and Bombay.
Within days of arriving in these cities, there were newspaper reports of secondary transmission occurring. It was total chaos. To make matters worse, people were getting on airplanes and flying out of India to all parts of the world. All of a sudden we had an international public health emergency on our hands. Fort Collins was the only remaining functional World Health Organization Collaborating Center for plague at that time, so my group at the Division of vector-borne Infectious Diseases coordinated a global response from there. We provided diagnostic reagents to approximately fourteen countries around the world. We worked closely with WHO and with the Indian government to develop enhanced surveillance and to calm some of the epidemic panic.
When the dust settled, the conclusions reached by an Indian commission and the WHO team were as follows:
- There was evidence of a limited outbreak of bubonic plague in Maharashtra state.
- There was evidence of a limited outbreak of pneumonic plague in the city of Surat, Gujarat State. However, there was no person-to-person transmission in Delhi, Bombay, Calcutta, or Madras and no plague cases were confirmed among persons traveling from India to other nations.
- Lack of diagnostic and epidemiologic capabilities led to overreporting of cases and ultimately to confusion, lack of confidence and panic.
- The outbreak itself in India cost the Indian economy in excess of 2 billion dollars. A more recent report that came out just a couple of months ago from Dr. Jacob John, an eminent infectious disease specialist in India, estimated that it was more like 3 billion US dollars.
- Other nations also suffered economic losses as a result of reduced trade, travel, surveillance costs, industry shut downs, and communication shut down within India.
- Effective surveillance, diagnosis, and control capabilities in India could have prevented this crisis.
We set up enhanced surveillance in the US and identified thirteen suspected potential imported cases. None of those thirteen were plague. The lessons learned from this epidemic are 1) that it underscored the importance of international infectious disease surveillance and cooperation; 2) the importance of prompt epidemiologic investigation; and 3) the need for adequate laboratory diagnostic capacity. It also demonstrated the global implications of local problems. What should have been a relatively unimportant local public health event, turned into a major international public health emergency and cost the global economy in excess of 4 to 5 billion in US dollars.
Dengue is a very old disease, and like plague, it has been around for
centuries. It used to
cause major pandemics that would move through the tropical regions of
the world and then disappear for periods of ten to forty years. That all
changed during World War II in the Southeast Asian region when we started
to see the emergence of Dengue Hemorrhagic Fever.
It was in the last twenty years of the 20th century where we see dengue resurging as a major epidemic disease, primarily in the tropics. What we have seen since 1980 is a dramatic geographic expansion in the distribution of both the viruses and the mosquito vectors associated with this disease. This has led to increased epidemic activity in most urban centers of the tropics. This in turn led to hyperendemicity or the cocirculation of multiple virus serotypes in the same community. It is this hyperendemicity that is most frequently associated with the emergence of dengue hemorrhagic fever, which is a severe and potentially fatal disease. It is this emergence of dengue hemorrhagic fever that is of major concern in the world today.
Dengue and yellow fever are transmitted by this mosquito, Aedes aegypti.
[SLIDE 6]
It was brought out of Africa, probably in the 1600s with the slave trade.
It basically spread around the world as the shipping industry developed
during the 18th and 19th centuries. It became a highly domesticated mosquito.
It lives in intimate association with humans, prefers to feed on humans,
and is a highly effective epidemic vector of dengue viruses. Probably
the most dramatic change in the epidemiology of dengue has been seen in
the American region.
[SLIDE 7] This slide shows the distribution in the Americas of the Aedes aegypti in the early 1930s as well as its current distribution. In the early part of the 20th century, there were major urban epidemics of yellow fever in the Americas. In 1947, the Pan American Health Organization (PAHO) initiated an eradication program for Aedes aegypti and by 1970 they had eliminated the mosquito from 23 countries in tropical America. The mosquito was still in northern South America, the Caribbean and the southern United States. This was about the same time the global malaria eradication program was changing. The public health officials at that time in their wisdom disbanded the Aedes aegypti eradication program, and combined it with the malaria eradication program, Aedes aegypti took advantage of this and began reinvading most of the tropical countries of the Americas.
The difference in 2000 from 1930 is that we have much larger urban populations in tropical America and we also have much higher mosquito densities because we have many more larval habitats for these mosquitoes. Every country that was reinvaded by this mosquito had epidemics of dengue a year or two later. All four virus serotypes were newly introduced into the American region. The region quickly became hyperendemic, and we saw the emergence of dengue hemorrhagic fever. [SLIDE 8] This shows over a thirty-year period from the 1970s, when there was no dengue hemorrhagic fever in the Americas through the 1990s including 1999 data, when it is one of the major public health problems in the Americas, especially in children. You can see it emerge in the 1980s, but in the 1990s it increased dramatically.
[SLIDE 9] There was one case in Puerto Rico in 1975. In 2000, twenty-eight countries in the American region have documented confirmed dengue hemorrhagic fever. The disease is endemic in most of those countries and many of them experience major epidemics. [SLIDE 10] On a global basis you can see the same kind of trend. The first epidemic of dengue hemorrhagic fever occurred in the wake of WWII in Southeast Asia, in the Philippines. You can see a dramatic increase in global reports of dengue hemorrhagic fever to WHO between 1955 and 1998. The last bar on the graph represents only three years, 1996-1998, but by the time we reach 2005 which will be the end of this decade, we will probably be much higher.
Dengue in the last twenty years has become one of the most important emerging tropical infectious diseases. In 2000, it has a global distribution in the tropics and over half of the world's population live in areas of risk. [SLIDE 11] Every year we see major epidemics. It is estimated that between 50 and 100 million cases of dengue fever and several hundred thousand cases of dengue hemorrhagic fever occur every year depending on the epidemic activity that occurs that particular year. In addition to its public health impact, dengue has a dramatic economic impact much as plague did in the Indian epidemic. Dr. Martin Melzer of Atlanta, a medical economist, has been working with us the last few years to try and measure the economic impact of epidemic dengue by calculating the disability adjusted life years (DALYs) for dengue. If you calculate the DALYs per million population for dengue, either in individual countries or globally as a whole, we found that the DALYs per million population for dengue are of the same order of magnitude as for many of the major tropical infectious diseases that receive hundreds of millions of dollars for prevention and control (e.g., malaria, tuberculosis, hepatitis, sexually transmitted diseases (excluding AIDS), the childhood cluster, and tropical cluster). The economic impact of this disease is just now being understood.
I want to remind you that the West Nile Virus epidemic that occurred in New York in the fall of 1999, was unprecedented in the last fifty years of the 20th century. It is epizootic because it occurred in birds and horses as well. [SLIDE 12] I want to also remind you that the West Nile belongs to the Japanese Encephalitis serocomplex of the family Flaviviridae, which has a distribution comparable to dengue. [SLIDE 13] This serocomplex has a worldwide distribution, and there are a number of viruses involved here. It was most likely an African virus that moved into India where it was discovered in the 1950s. [SLIDE 14] It caused recent epidemics/epizootics in the Middle East, Europe, and central Asia and in the United States in the summer of 1999. We do not know from where or how it was introduced into the U.S. [SLIDE 15] Shown here are the human cases that were reported in New York in 1999. This is a classic epidemic curve that you see in areas where you don't have surveillance. The epidemic is usually detected at the peak of the epidemic or at the time when it has begun to wane.
The epidemic was detected in the week of August 23. Retrospective surveillance ultimately showed that the first human case had onset on August 2, the last human case had onset on September 22. Bird infections were observed occurring before this, possibly as early as July. Most of the human cases occurred in New York, but some were in counties surrounding the cities. [SLIDE 16] Before we can fully understand the public health implications of West Nile virus introduction in the Western Hemisphere, we first need to understand the temporal and geographic spread of this virus. We have no idea where it spread in 1999. We have implemented surveillance, but we are uncertain about the geographic distribution. Every place we find this virus we are going to have to look independently at the mosquito vectors and the reservoir hosts to understand the transmission cycle and ultimately, to understand the transmission dynamics. We need to have this information before we can identify risk factors associated with human and animal infections.
So there is a lot of work that we have to do, not only in the US, but also in other areas. A program is ongoing in Canada and people in Latin American are also looking for this virus. We have spent a lot of time in the last six months developing a national surveillance plan for West Nile. We have worked very closely with state epidemiologists, state vector control people, and wildlife biologist in a number of states to try and monitor this virus. We are right now in the middle of another major episode in the US. Not unexpectedly, the virus has spread wider this year than last.
My last example is yellow fever. We do not hear a lot about yellow fever and we shouldn't because we have the cheapest, most effective, safest, live virus vaccine available to mankind. The problem is that it is not used because it is considered too expensive to immunize all the children. We have seen as part of this resurgence of vector-borne diseases in the 1980s, increased epidemic yellow fever activity, primarily in West Africa during the mid-1980s. [SLIDE 17] But also in the American region, several significant outbreaks have occurred. We have also seen the first epizootic in thirty to forty years in East Africa in 1992 and 1993, but yellow fever has not truly resurged yet.
Urban yellow fever is transmitted by the Aedes aegypti mosquito. With the reinvasion of the American tropics by Aedes aegypti, the area is at the highest risk in over fifty years for urban yellow fever epidemics. Some of us feel that it is not a matter of whether it is going to occur, but simply a matter of when it is going to occur. That is our concern in the beginning part of the 21st century. Our concern is focused on the northern regions of South America. This is the enzootic area of yellow fever in the Americas. [SLIDE 18] Shown here are cities that have populations of over 1 million people that have had yellow fever activity in the last ten years or so, the most recent in Brazil. In 1998, there was a major scare in Santa Cruz, Bolivia, where it was documented that there were two clusters of transmission in the city. Six acute cases were confirmed; five died. Three infections were likely contracted in the city. [SLIDE 19] Potentially you could get on a plane in Santa Cruz, Bolivia, and be just about anywhere in the world in 24 to 36 hours, for example the Asia Pacific area, an area that has never had yellow fever in the past. So the concern is that once we see urban transmissions starting in these South American cities, it is going to spread very rapidly. We have approximately 3 hundred million people living in urban centers in the Americas and most are susceptible to yellow fever. It will then spread very quickly to Asia and the Pacific. If nothing else, we will be able I hope, to answer that age-old question in virology--Why hasn't yellow fever ever occurred in Asia? If it should happen, it will be the next global public health emergency.
Factors Responsible for Resurgence
Let me finish up by talking about why we have seen such a dramatic resurgence of vector-borne diseases in the waning years of the 20th century. I think that it started in the 1960s with the complacency that set in following successful programs of prevention and control in the middle part of the 20th century. The complacency played a major role in policy decisions that resulted in decreased resources and deterioration of the public health infrastructure. In addition, major demographic and societal changes have influenced vector-borne diseases in the past fifty years as well.
Population growth is one of the main driving forces for most of these changes. In the last fifty years, we have seen unprecedented population growth in developing countries, and that population growth has driven a lot of changes in the world. It has resulted in massive unplanned, uncontrolled urbanization in tropical cities. This resulted in deteriorating housing, water and sewage waste management systems. This in turn creates ideal conditions for increased transmission of mosquito borne disease, rodent borne disease, water borne disease, and food borne disease. We are seeing all of them in major urban centers. Deforestation is also driven primarily by population growth and has led to increased transmission of some vector-borne diseases. Changing agricultural practices, also driven by population pressure, result in increased vector-borne disease transmission.
There have been many societal changes that have influenced vector-borne disease transmission. Life style changes, usually a concept that is associated with AIDS, is equally appropriate for vector-borne diseases. Lyme disease and plague are partially the result of people wanting to go back to nature. They want to build their houses right in the middle of an enzootic area, and they do not want anyone to disturb any of the flora and fauna. The result is that they end up with some of these diseases. All of our consumer goods are packaged in non-biodegradable plastics and tins that are discarded in the environment making good mosquito larval habitats. We have had an explosion in the number of automobiles in this world. Every automobile has four tires that are discarded after three to five years to become ideal larval habitats for mosquitoes and ideal harborage for all kinds of rodents and vermin. They are a major global problem.
Commerce is also a factor. The container shipping industry has been responsible for moving all kinds of agents such as mosquitoes and other vermin around the world. We have two mosquitoes in the US, Aedes albopictus and Aedes japonicus that are creating problems for us as a result of this type of shipping. Finally, modern transportation.
The jet airplane has revolutionized travel in the world. We have literally hundreds of millions of people moving every day between international population centers. It is the ideal mechanism to move pathogens between population centers, between regions, and between continents. A lot of the agents have incubation periods of 3-10 days, and a person that becomes infected gets on a plane and carries it to their next destination. You thus have constant movement of all kinds of pathogens between regions into areas that are permissive for transmission because we have not had effective mosquito control or other types of vector-borne disease control.
With increased transmission, there is greater chance for genetic change in these pathogens. This is probably the area that we know the least about. We do know that as you increase transmission turnover, you have increased potential for genetic change and certainly as you have increased genetic change, you have greater potential for selecting pathogens with greater epidemic potential. Vector-borne diseases are particularly vulnerable because they have to pass through two hosts, and they are extremely climate and environmentally sensitive. They are influenced by climate changes that could affect genetic change. This is an area that needs a great deal of research.
Changes in public health haven't really influenced the resurgence of disease, but it has certainly influenced the way we deal with epidemic vector-borne diseases. This relates to the change in the public health infrastructure. The complacency and policy decisions that were implemented in the 1970s, led to decreasing resources for infectious diseases in general and vector-borne diseases in particular. This resulted in a decay in the infrastructure for vector-borne diseases and shortage of trained personnel. You can go to some of the countries in Asia where vector-borne diseases are the major public health problems and you will not find a single vector biologist on the Ministry of Health staff that has been properly trained. We changed our way of dealing with these diseases in the early 1970s. We drifted away from the old prevention algorithm to one of emergency response.
Moreover, most of our medical schools have focused on curative medicine for the last thirty years. Therefore, preventive medicine has been de-emphasized, so a lot of physicians don't think about preventive medicine. The result has been a generation of people in this world who are raised to believe in quick fixes. They do not want to go to the trouble of preventing diseases. When they get sick, they go to the doctor, they get a pill, they get well, and everything is fine. It is what I call the "magic bullet syndrome" that has occurred in the last thirty years.
I put climate change with a question mark because if you read the popular press, it would lead you to believe that climate change is a major driving force for the resurgence of the many vector-borne diseases. vector-borne diseases, as we have already said, are very climate sensitive, but if you look at the data and analyze it appropriately, you will find that there is very little evidence that long-term climate changes have had anything to do with the recent resurgence of these diseases. It doesn't mean that it won't in the future, but the resurgence that has occurred can be tied most effectively to demographic and societal changes as opposed to climate change.
Reversing the Trend
What are the prospects for the future? In the 21st century, I think we are going to see continued population growth; continued unplanned, uncontrolled urbanization; continued changes in land use and movement of people; lifestyle changes and climate change. All of these changes will have a dramatic influence on transmission of vector-borne diseases, and we are going to see continued major epidemics of vector-borne diseases if we don't do something about it now.
What might we be able to do to reverse the trend of emergent/resurgent vector-borne diseases:
- We have to get control of the population growth in this world, and
we are going to have to do something about urbanization. We, as public
health officials, do not often work with urban planners and waste management
specialists. We are going to have to start working together to create
new alliances to make the urban centers of the world more livable.
- We need to control deforestation and changing agricultural practices,
which may expose people to diseases that they had not been previously
exposed to. More importantly, you create conditions that are ideal for
organisms to move in and new diseases to be transmitted.
- We are going to have to rebuild our public health infrastructure,
especially for vector-borne diseases. There is a desperate need for
young, bright people working in this field. The field is probably in
its lowest ebb in terms of well-trained people working in the field.
- We need laboratories to diagnose these diseases. You can't work on
them without good laboratory diagnosis. You need resources to implement
these kinds of training programs.
- We need new research. The research support for vector-borne diseases
began to decrease about 1970. Those of us who entered the field in the
late 1960s and early 70s remember the dry period for about thirty years
when there was very little in the way of funds for vector-borne diseases.
I think we are in a period right now where we will see a change. We
need much more research on vaccines for use in preventive programs,
drugs, diagnostics, vector control, and integrated prevention strategies.
All of these areas need a lot of work and a lot of new ideas. We need
new people coming into the field and looking at this from a different
perspective.
- We need to look critically at our public health policy if we are going
to succeed in controlling or preventing some of these diseases. To quote
Joshua Lederberg from 1997, "Today we emphasize individual rights
over community needs more than we did fifty or seventy-five years ago.
Restraining the rights of individuals is a far greater sin than allowing
the infection of others. In the triumph of individual rights, the public
health perspective has had an uphill struggle in recent pandemics."
What he is saying is that public health has always approached disease
control from a community perspective. We are now not looking at it so
much from a community perspective as we are from the individual perspective.
There has to be a middle ground somewhere that will allow public health
officials to do what they need to do to prevent disease in a community.
- Finally, we need to emphasize disease prevention. We need to go back a few years because many of these diseases, especially the vector-borne diseases, are orphan diseases. They are all preventable yet they don't receive a lot of money or a lot of attention for research on vaccines and drugs. We understand the ecology of these diseases and with proper support they can be prevented. To do this we need better surveillance, laboratory-based surveillance; we need to develop better prevention strategies, and we need to bring the public into the whole process. One of the mistakes we made in the past is that we created vertically structured programs where the government did everything. They were very effective, but they did not have sustainability. As soon as government funding dried up, the program terminated and the problem came back; usually worse than it was before. We need public outreach and education. We need to bring the public into these programs as full partners to develop prevention and control programs if we expect to reverse the trend of emerging infectious diseases in the next century.
Readings:
Gubler DJ. "Dengue and dengue hemorrhagic fever." Clinical Microbiology Reviews, 1998; 11(3): 480-496.
Gubler DJ. "Resurgent vector-borne diseases as a global health problem." Emerging Infectious Diseases, 1998; 4(3): 442-50.
Tsai TF, Popovici F, Cernescu C, Campbell GL. Nedelcu NI., for the Investigative Team. "West Nile encephalitis epidemic in southeastern Romania." Lancet, 1998; 352: 767-771, 1998.
Top | Home | Topics | Lecture Intro | Go to Lecture
©2000, University of Washington. All Rights Reserved.
Send comments to Carrie Horwitch, MD, MPH
Last updated: November 2000