Overview
"During a recent session, I reviewed 5 of my patients who are high ED utilizers and came up with strategies to reduce utilization with the help of pharmacy, mental health, and nursing colleagues. I started implementing these strategies during the session, whether that was sending a note to a patient's mental health provider or refilling medications that were expiring soon. This was more impactful for these patients than if I had spent the day just seeing them in clinic."
-Seattle VA Internal Medicine Resident
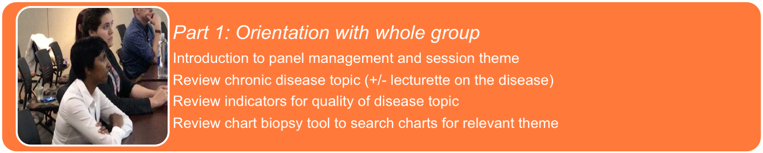
The Three Parts of Panel Management Sessions:
Why did we choose to implement panel management workshops?
Dynamic panel management didactics enable learners to:
- • Learn principles of population health at the level of individual panels in primary care as well as identify high risk patients for ambulatory care sensitive conditions.
- • Change focus of care from solely face-to-face visits to continuous between visit care.
- • Utilize time, panel data, and chart biopsy tools to actively manage their panels.
- • Review cases with trainees and faculty of different professions to facilitate inter-professional, team-based patient care.

Clinical Problems Addressed:
Interprofessional panel management session, Seattle VA.
- • Identifying panel-level measures/outcomes that are not meeting targets (e.g. HbA1c <9.0).
- • Goal to benefit individual patients.
- • Providers cannot address all care needed during in-person visits: Goal to achieve continuous between-visit care.
- • Panel management and team-based care concepts may be new or abstract. Trainees of various professions may not know how to work on panel data or how to work with team members in care of panel patients. Goal to learn population health and inter-professional care concepts.
Executive Summary
Training Objectives:
- 1. Learn about a specific clinical theme or prevention measure including rationale, targets to measure, how to access data, and how to perform a brief chart review ("Chart biopsy tool")
- 2. Seek guidance from interprofessional cadre of trainees and team members, understand the unique and complementary roles that each team member can play in care of complex patients
- 3. In session discussion of cases, construct Pareto chart of etiologies and systems factors that might be addressed via quality improvement.
- 4. Get work done! Create action plan and initiate implementation during the session (e.g. medication and/or diagnostic test orders, communication with clinical team, etc).
Rationale/Problems addressed
- • Monitoring patient clinical measures and impact of treatment strategies requires continuous between-visit care and team effort.
Competencies fulfilled:
Panel Management Curriculum fulfills several Interprofessional Education Collaborative (IPEC) competencies including:
- • IPEC RR3: Engage diverse professionals who complement one’s own professional expertise, as well as associated resources, to develop strategies to meet specific health and healthcare needs of patients and populations.
- • IPEC RR5: Use the full scope of knowledge, skills, and abilities of available health professionals and health care workers to provide care that is safe, timely, efficient, effective, and equitable.
- • IPEC RR8: Engage in continuous professional and interprofessional development to enhance team performance
- • IPEC RR9: Use unique and complementary abilities of all members of the team to optimize the quality of patient care
- • IPEC TT4: Integrate the knowledge and experience of other professions-appropriate to the specific care situation-to inform care decisions, while respecting patient and community values and priorities/preferences for care.
- • IPEC TT8: Reflect on individual and team performance for individual, as well as team, performance improvement.
Panel Management Curriculum also fulfills ACGME core competencies such as:
- • Practice-Based Learning and Improvement (PBLI)
- • Systems-Based Practice (SBP)
- • Interpersonal and communication skills
- • Professionalism
- • Milestones such as sub-competency SBP01: "Works effectively within an interprofessional team", and PROF01: "Has professional and respectful interactions with patients, caregivers and members of the interprofessional team."
Core domains covered (PI, SDM, SR, IPC)
- • Sustained relationships: The panel sessions help to facilitate needed care and further follow-up between patients and members of the care team; Sessions themselves enhance interprofessional team-work of trainees, faculty and staff.
- • Shared Decision Making: The team works together to create the treatment plan
- • Interprofessional Collaboration: Interprofessional cadre of trainees and faculty/staff work together in the sessions to trouble-shoot challenging patient issues. After case discussions, trainees may contact team members with new plans, also may have huddles with their care team members to discuss further.
Training Goals and Objectives
Description & Implementation
Implementation Requirements
Why organize a panel management session?
- • Participants can learn how to do panel management in an interprofessional setting.
- • Just giving providers data on their panel doesn't change outcomes; providers need tools and time to respond to their data.
- • Session provides dedicated time for practicing panel management on real patients and generating next steps.
Interview of trainees following Tobacco Cessation Panel Management Session, July 2017
Choose a clinical focus / topic of your workshop
A). Examples of Clinical Focus
- • Hypertension
- • Diabetes
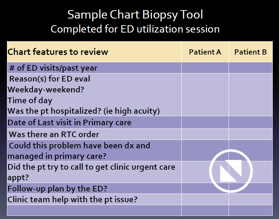
- • Emergency department utilization
- • Opioid monitoring
- • Care Assessment Need (CAN) score: a tool available to VA providers that estimates the probability of death or admission for each patient within 90 days or 1 year
B) Consider your site’s current clinical performance improvement needs via one or more of the following methods:
- • Review clinical data at your site and identify metrics that are divergent from the national average.
- • Complete focus group discussions with providers, trainees, teamlet members, clinic leadership, service line leaders, academic affiliates, other key stakeholders about areas for clinical improvement.
- • Implement a survey to ask clinic providers, trainees, etc. for their preferences.
- • Assess faculty resources and faculty development needs.
Data to Review
A). Providers will need data on their patient panels.
- • Someone may need to compile these data for each provider on a regular basis OR providers may have access to their own data.
- • Methods for accessing data will be organization-specific.
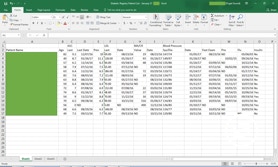
B). Examples:
- • Seattle VA trainees have access to a confidential site called the Primary Care Almanac that has data on each provider’s patient panel.
- • Data managers may compile data sets for providers to review on specific disease metrics.
- • Video Example: Using the Primary Care Almanac to generate Provider Level patient lists filtered by specific disease metric criteria
Screen shot of excel file with diabetic patient metrics for one provider’s panel. (Click to zoom)
Participants and Stakeholders
Typical sessions at Seattle VA have included:
- • Trainees: NP residents and students, MD residents, pharmacy residents, and psychology fellows.
- • Faculty: ARNPs, MDs, pharmacists, RN care managers
- • Clinical topic chosen may depend on group composition.
Nurse practitioner, internal medicine residents and pharmacy trainees participate in a panel management session on Tobacco Cessation.
Finding the time
A). When to implement?
- • If working with trainees, consider time of year, rotation, and level of experience.
- • For trainees, a panel management workshop is most helpful during an outpatient or primary care block so that participants can use these skills immediately.
- • Interprofessional training will require coordination across departments.
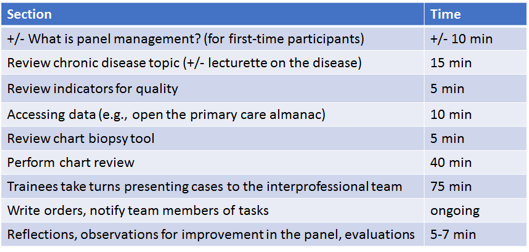
B). How long do sessions take?
- • At the Seattle VA, sessions are 3-4 hours.
C). How often are sessions completed?
- • Frequency will be dictated by clinical demands at your site.
- • At the Seattle VA, we conduct 5-6 sessions per academic year covering 4-5 topics.
D). What about after the workshop?
- • When the workshop is finished, ongoing panel management is most realistic if dedicated time is provided.



Each participant should have a computer to review patient charts and act on recommendations in real time.
Room and equipment
- • Panel management workshops are NOT didactic sessions. Active patient care occurs!
- • Workshops will require participants to review charts on real patients, engage in active discussion, and act on ideas/strategies in the moment.
- • Projector for reviewing patient charts in the EMR as a group
- • Easel to complete Pareto chart (or may construct on excel and project)
- • Each trainee must have access to a computer for chart review and for trainee presentations.
**Presentation equipment AND Computers for electronic medical record access are a must!**
Easel for group brainstorming, projector for didactic sessions and viewing patient charts.
Detailed Session Flow
1. Panel Management Introduction
- • Define panel management
- • Didactic session to large group with Faculty Presenters.

Panel Management Introduction Didactic Sample Slides
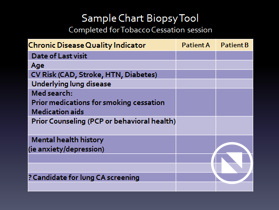
2. Review best practices for the theme of the session
- • Didactic session to large group
- • Facilitator will identify the quality metrics for the topic of choice.
- • Facilitator will also explain to participants how to access data on their panel to review these metrics.

Smoking Cessation Didactics Sample Slide
3. Review Chart Biopsy Tool
- • Large Group Didactics
- • A chart biopsy tool is a list of patient or case characteristics relevant to the specific clinical topic under review. Participants use this list of items when reviewing charts to identify patterns and barriers to quality care for each patient.
- • The chart biopsy tool will look different for different clinical topics.
- • The facilitator can start by leading a brainstorming session to generate the chart biopsy tool. Below is a sample blank chart biopsy tool from a session on ED utilization.
6. Trainee Presentations
- • Providers take turns presenting one of their patients to the group, based on their chart review.
- • Presentations should be 2-3 minutes long at most, covering the salient features identified on the chart biopsy tool.
- • Each patient's chart is opened on a large screen so the group can view it together during discussion.
- • Interprofessional participants highlight issues, offer strategies, provide suggestions to the provider to improve the care of each patient.
- • Providers should write orders, notify team members of tasks, or otherwise begin to implement the suggestions generated during the discussion of their patient.
- • Participants should be doing these tasks during the session
The goal is to complete work in-session, rather than generate more work for later!
7. Closing
- • Common themes of barriers to care identified during trainee presentations are aggregated on a Pareto chart
- • The chart is reviewed at the end of all the trainee presentations
- • A summary of action plans to address barrier to care is provided by a faculty leader
- • Trainees leave panel management session with action plans in motion and limited additional follow-up work needed.
5. Introduce Trainee Presentations
- • Didactic Session to Large Group
4. Perform Chart Review: Trainees independently review selected patients out of target measure range.
- • Each participant selects 5-6 patients who are not meeting quality metrics.
- • Participants work individually to review these patients' charts, using the framework provided by the chart biopsy tool.
- • It can be helpful to have the chart biopsy tool displayed on the projector during this time
Evaluation
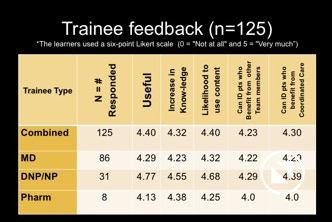
Evaluation by Trainees
- • Trainees evaluate panel management sessions following the completion of each session. These evaluations are used to tailor the curriculum of future panel management sessions.
Trainee feedback from panel management sessions. Click to enlarge.
Translation of Panel Management to Clinical Care
- • Nine out of seventeen QI projects at the Seattle VA were generated from panel management sessions.
- • Impact of QI projects in clinical domains of ED utilization, medication adherence and reducing poly-pharmacy
- • QI project metrics and PSDA cycle review allow for ongoing assessment of outcomes from panel management sessions
Sustainability & Dissemination
What makes this curriculum sustainable?
Innovations and curricular additions/changes become sustainable when they demonstrate evidence of value, benefit to patient care, and feasibility. Over time, such changes become a part of the core program and culture such that “you can’t imagine doing without it.”
Panel management significance to training and patient care:
- 1. Population health at the level of a panel of patients is important in chronic disease management and preventive health, with focus on between visit care in addition to continuous care.
- 2. Trainees in primary care are expected to learn skills in population panel management, to improve clinical outcomes.
- 3. The curriculum described is highly rated by trainees, with increased confidence in using skills learned to access data and review clinical outcomes measures over time.
- 4. Interprofessional trainee, faculty and team review of panel data for patients with out-of-target measures provides new strategies and input.
- 5. Panel management performance data helps primary care trainees to learn how they are doing and ways to work with their team to improve.
Panel Management as an impetus for patient safety/quality improvement projects:
Panel management session discussions include identification of systems issues and construction of a Pareto chart of these issues. We have identified numerous quality improvement opportunities via panel management sessions that led to projects, often resulting in significant benefit.
Examples of quality improvement projects identified from panel management sessions, and leading to improved outcomes:
- 1. Emergency Department (ED) Utilization by patients of low acuity
- 1.1. Outcomes: sustained reduction in ESI 4-5 visits to ED, multidisciplinary approach to alternative options for care and multiple PDSA cycles over 2 yrs.
- 2. Opioid monitoring, urine toxicology and state controlled substance database assessment
- 2.1. Outcomes: improved overall screening rates and identification of dual prescribers and substance use that resulted in cancelled narcotic medication plans for chronic pain
- 3. Hypertension medication adherence
- 3.1. Outcomes: Educational information for patients and staff resulted in improved medication possession ratio (MPR)
Dissemination:
Our trainees have enthusiastically encouraged continued curriculum with face to face interprofessional engagement in patient care outside of busy patient clinics. They work together as colleagues to better provide collaborative care and goals of integrated care.
Our curriculum is being disseminated to other trainees and clinic sites in our academic affiliates and other clinic teams in our own VA.
Acknowledgements
Panel Management curriculum design and implementation:
Catherine Kaminetzky, MD, MPH; Howard Mun, Pharm D, Joyce Wipf, MD
Curriculum Evaluation:
Teaching session evaluations: Anne Poppe, PhD, RN
Panel data: Jamie Davis, Data Manager; Christopher Vanderwarker, MD, MBA
Implementation Kit:
John Geyer, MD Chief Resident Clinician-Teacher Fellow
Mayuree Rao, MD R2
Anna Golob, MD, Associate Program Director CoEPCE
Joyce Wipf, MD, Director CoEPCE
References
1. Neuwirth EEB, Schmittdiel JA, Tallman K, Bellows J. Understanding panel management: a comparative study of an emerging approach to population care. The Permanente Journal. 2007;11(3):12.
2. Kaminetzky CP, Nelson KM. Editorial. In the Office and In-Between: The Role of Panel Management in Primary Care. J Gen Intern Med. 2015 Jul;30(7):876-7/
3. Kaminetzky CP, Beste LA, Poppe AP, Doan DB, Mun HK, Woods NF, Wipf JE. Implementation of a novel population panel management curriculum among interprofessional health care trainees. BMJ Medical Education. 2017 Dec 22;17(1):264.
4. Cusack CM, Knudson AD, Kronstadt JL, Singer RF, Brown AL. Practice-based population health: information technology to support transformation to proactive primary care. United States. Agency for Healthcare Research and Quality; 2010.
5. Morrow RW, Haughton J. Linking continuing professional development and practice improvement to build the primary care academic home. Academic Medicine. 2011;86(11):e11.
6. Kanter M, Martinez O, Lindsay G, Andrews K, Denver C. Proactive office encounter: a systematic approach to preventive and chronic care at every patient encounter. The Permanente Journal. 2010;14(3):38.
7. Houston TK, Wall T, Allison JJ, et al. Implementing achievable benchmarks in preventive health: a controlled trial in residency education. Academic Medicine. 2006;81(7):608-616.
8. Chen EH, Bodenheimer T. Improving population health through team-based panel management: comment on “Electronic medical record reminders and panel management to improve primary care of elderly patients”. Archives of internal medicine. 2011;171(17):1558-1559.
9. Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health affairs. 2010;29(5):835-843.
Questions / Comments