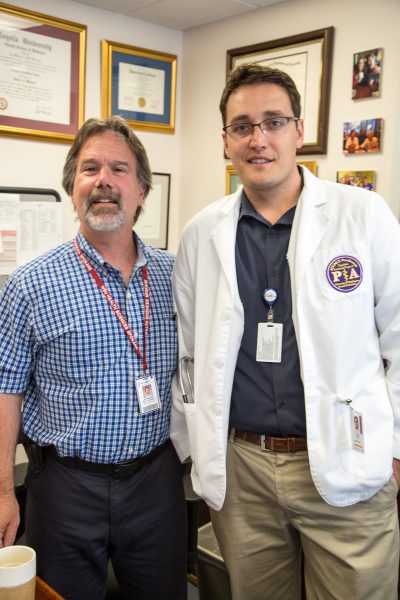
Tucker Larsen has just started his inpatient rotation at St. Luke’s Rehabilitation Institute in Spokane, WA. The facility provides inpatient and outpatient treatment for strokes, spinal cord injuries, traumatic brain injuries, orthopedic and polytrauma injuries, neuromuscular disorders, along with a host of other problems. For 30 days, Tucker is under the direction of Dr. Greg Carter, the facility’s Medical Director. This is part of Tucker’s clinical year education during his two years with the UW MEDEX Northwest physician assistant training program in Spokane. St. Luke’s is a chance for exposure to a part of medicine that may not be familiar to him.
Turns out that Tucker is not the only student under Dr. Carter’s charge. An energetic presence, Dr. Carter is responsible for yet another MEDEX student, Megan Johnson of Seattle Class 48, along with a DO student from Pacific Northwest University. With help from his own PA-Cs—MEDEX graduates Joe Gaines and Rachel Ragosta—it’s not uncommon for Dr. Carter to take on three or four students at a time. And at 102 beds and serving over 7,000 patients a year, St. Luke’s is the largest free-standing rehabilitation hospital on the West Coast, so there’s plenty for the students to do and learn. Students like Tucker spend the majority of their time on the acute in-patient medical rehabilitation service where patients can be quite medically complex and challenging.
Our visit with Tucker occurs at the very start of his rotation at St. Luke’s. By now he’s already been through five other rotations and a 5-month family medicine preceptorship at Benewah Medical Center in Plummer, Idaho. That one really stuck with him.
“The amazing thing about Benawah is that it’s not governed by Indian Health Services—it’s owned by the Coeur d’Alene tribe,” Tucker tells us. This small detail allows for a lot of freedom in the way that the clinic delivers services to its community.
Tucker further explains: “Benawah is one of very few American Indian healthcare facilities that delivers care to non-American Indians alike, and they do it successfully. And they do it without any sort of tension between all the people that come. In fact, they have tribes from all over the nation that come and walk around the facility asking, ‘How do you make this work?’ Because there’s so much historical trauma, and it’s a very sensitive topic to deal with in the Native American community. But I think that they’re doing a really great job. I lucked out to have been there.”
Time spent with Tucker Larsen reveals someone who is deeply concerned with how things work, and the health of the larger community. This is for good reason as Tucker comes to MEDEX from a social worker background.
“I gravitated towards the mental health field because I have family with mental health issues, and I have an understanding that everybody has at some point in their life struggled with mental health illness,” he says.
For three years he was a caseworker in community mental health in his hometown of Missoula, MT. “I found that the people I was working with barely had income. They were trying to get into our program and had nothing, not even a home. And so I took over the Homeless Outreach program through my mental health agency.”
Tucker would source homeless veterans, homeless women and families, and homeless men with mental illnesses. “We would do our best to find them housing, employment, insurance, and get them on the Medicaid/Medicare waiting list,” he says.
It was around that time that Tucker decided to become a physician assistant. Tucker did his undergraduate work at Boston University. But to fulfill PA school prerequisites, he moved from Montana to Oregon in order to take some post-baccalaureate classes in anatomy and physiology along with microbiology. While attending classes in Eugene, he worked at a group home, becoming one of the supervisors of a forensic psychiatric residence for adult men and women who have psychotic illness or extreme mania bipolar disorder, and had committed a violent crime.
Where most would distance themselves from those in society grappling with mental illness, Tucker’s view is just the opposite. “I think you’d be hard pressed to find anybody who says they were never anxious for a short time, or they’ve never been depressed,” he says. “And anybody who says they weren’t probably has some things to work through.”
“What I discovered is that so many people are forgotten by society because others are scared of psychosis or mania,” he says. “But mental health doesn’t correlate with intelligence, and it doesn’t correlate with what individuals can bring to the world. In my work, I’ve found some amazingly rich life stories and talented people who otherwise would have been shunned to the side.”
It’s clear that Tucker’s commitment is to bring light to the darker corners of society. “My heart lies with community health agencies,” he says. “Those are the only places I’ve ever worked. I can’t really describe why, other than when you’re paying that little drop into a bucket, you really feel like it’s significant. So I want to work in a place that has a sense of community, has a sense of teamwork and collaboration, and where patients are allowed to participate in their care. Because if they’re not inspired to make their own lives better, there’s no reason for anybody to be doing this.”
Having worked in these systems for some time, Tucker is keenly aware of the obstacles to proper care. Despite that, his attitude is altruistic. “People are constrained by policies and Medicare,” he tells us. “But really, at the end of the day, everybody who works on a healthcare team is there to do what they can to make people feel better.”
It’s this community health focus that drove Tucker towards PA training. He figures that an education with a broad disease focus will arm him with the tools to serve the homeless man who can’t afford to see a doctor, or the homeless woman that requires a routine health exam.
“I was continuously banging my head against the wall until a friend of mine and my mother in the same week told me, ‘Well, go to PA school’. And I was like, ‘But I’d have to go back to school.’ Their response was, ‘Well, you better get going.’”
With his prerequisites fulfilled, Tucker applied to the University of Washington and MEDEX Northwest. This occurred while he was coordinating all his efforts—taking classes and working as a supervisor in the lock-down forensic psychiatric residence in Eugene. He was accepted into MEDEX Spokane Class 18.
“That was my first choice because I wanted to be close to home, which is the Northwest, but specifically Missoula,” he says. “Gratefully, I got in.”
Still, a total of seven cumulative years in community mental health took its toll on Tucker. His father was a social worker in the 60’s. When he stopped to go into another field, he told his son, “Working in mental health is like painting a fence. You can’t help but get a little on you.” For Tucker, this translates as empathy. “It makes me a bit more insightful into how others think,” he says.
He was able to bring some of that kind of skill to the didactic year. “I think it’s important for people to get along and to harness each other’s gifts,” he says. “Which is one thing MEDEX does really well. It picks 30 people with very unique personalities and skill sets, and puts them into a boiler room. It worked out exceptionally well for Spokane Class 18. We’re tight as a family. That’s cool.“
Tucker recalls MEDEX Program Director Terry Scott speaking to interview candidates early in the admissions process. “He said there’s a method to who they pick, there’s a method to what they’re looking for. It’s hard to explain, but it works. I think that the faculty that selected the students knows that they need to find goal-driven people that are willing to work together. They did a really good job with that because it’s an aggressive pace of education. If you fall behind or if you start to sink, you can go fast if you don’t have support. And I never felt like anybody, at least in our crew in Spokane, struggled much. Everybody had a breakdown or two here or there, but it was the collaborative spirit that won out.”
At this point Tucker is weeks away from graduating, and the future looks good. Spokane Class 18 convenes for the last time on August 26th for its graduation ceremony. What follows is the ARC-PA board certification exams, and then employment search as a physician assistant.
Thinking back on these past two years at MEDEX, Tucker is reflective.
“It’s very humbling to get the opportunity to even go through PA school, to eventually sit through your boards, and to become a PA. I know it’s been a dream of mine for about five years, and it’s the exact same for everybody else in my program. And it’s amazing to be at the tail end of it and see this huge machine that is medicine that works well sometimes and not so well at other times. But to go into it, to be a part of it, to try and make it better, and to try and make people’s lives better—well, it’s humbling.”