ACUTE POISONING
MECHANISM OF ACUTE TOXICITY
The mechanism of acute organophosphate pesticide toxicity can be discerned from the clinical diagnostic tools and antidotes used to treat organophosphate poisonings. Namely, the determination of red blood cell and plasma pseudocholinesterase activity and treatment with 2-PAM & atropine suggests that acute organophosphate toxicity occurs through inhibition of acetylcholinesterase.
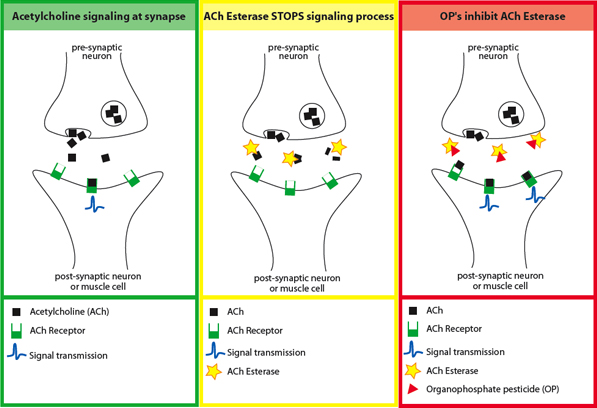
Organophosphates are anti-esterase insecticides, and exert their acute effects by causing overstimulation at cholinergic nerve terminals. This process occurs in both insects and humans. Normally, acetylcholinesterase catalyzes the degradation of the neurotransmitter acetylcholine in the synapse (yellow panel below). Organophosphate pesticides phosphorylate acetylcholine, thereby reducing the ability of the enzyme to break down the neurotransmitter (red panel below). This produces an accumulation of acetylcholine in the central and peripheral nervous systems, resulting in an acute cholinergic syndrome via continuous neurotransmission. The clinical onset of cholinergic over-stimulation can vary from almost instantaneous to several hours after exposure.
SIGNS AND SYMPTOMS
Medical students, clinical toxicologists, and emergency room physicians are often taught acronyms for the classic constellation of symptoms of cholinergic excess - copious respiratory and oral secretions, diarrhea and vomiting, sweating, altered mental status, autonomic instability, and generalized weakness that can progress to paralysis and respiratory arrest. One example is M-U-D-D-L-E-S: miosis, urination, diarrhea, diaphoresis, lacrimation, excitation of the central nervous system, and salivation. This works reasonably well in adults.
CHILDREN VS. ADULTS
Reviews of case series indicate that pediatric organophosphate poisonings often manifest with hypotonia or mental status changes such as lethargy and coma, as well as seizures, the latter being relatively rare in adult OP poisoning3.
Diagnosing pediatric OP poisoning is complicated by the fact that the non-specific symptoms of acute pesticide toxicity are easily attributed to common pediatric diagnoses such as respiratory infections, viral syndromes, gastroenteritis, atopic dermatitis or drug-related encephalopathy.
In our case study, the presentation was consistent with several commonly encountered pediatric illnesses. The lack of diagnostic support for infection coupled with the expanded exposure history allowed identification of the underlying etiology of acute pesticide poisoning.
DIAGNOSIS AND TREATMENT
Diagnosis of organophosphate poisoning is often made based on the history of significant exposure and consistent symptoms, as in the case described. If probable organophosphate poisoning is suspected, immediate treatment is recommended without waiting for laboratory confirmation. Early consultation with a poisoning specialist is recommended and is available through the Poison Control Center network if not available on site, as was done in this case. Early intervention reduces the risks of progression of the initial cholinergic crisis and of sequelae for most patients.
In suspect cases, blood samples should be drawn to measure plasma pseudocholinesterase and red blood cell (RBC) acetylcholinesterase (AChE) levels. These tests are available in most hospital laboratories. Depressions of plasma pseudocholinesterase and/or RBC AChE activities are indicative of excessive organophosphate absorption. The enzyme depression becomes apparent within a few minutes or hours after absorption of a significant amount of organophosphate. Certain organophosphates may selectively inhibit either plasma pseudocholinesterase or RBC acetylcholinesterase. Depression of the plasma enzyme generally persists for several days to a few weeks. The RBC enzyme activity may take several days to reach its minimum and usually remains depressed longer, sometimes 1-3 months, until new enzyme replaces that inactivated by organophosphate.
Cholinesterase(ChE) Depression as a Diagnostic Tool
- Remember: Individual baseline ChE levels are variable
- To confirm suspected OP poisoning:
- Compare post-exposure ChE levels to those at time of illness
- Clinically significant OP exposure:
- 20% depression of plasma pseudocholinesterase
- 15% depression of RBC ChE
Baseline levels of blood cholinesterase are variable within the population . Interpretation of ChE levels during a suspected poisoning event is difficult in the absence of the individual's pre- or post-exposure ChE levels. A pre- or post-exposure measurement that is 20% or 15% higher for the plasma and RBC enzymes, respectively, suggests clinically significant exposure has occurred.
The body hydrolizes organophosphates, creating alkyl phosphates and phenols which can be detected in the urine up to 48 hours after pesticide absorption. These analyses are sometimes useful in identifying and quantifying the actual pesticide to which a patient or research subject has been exposed. That said, there is no available data allowing interpretation of urinary metabolite concentrations for clinical outcomes. Urinary alkyl phosphate and phenol analyses can demonstrate organophosphate absorption at lower dosages than those required to depress cholinesterase activities and at much lower dosages than those required to produce signs and symptoms of toxicity. These urinary metabolites are often used to assess the presence of chronic organophosphate exposure.
Treatments for OP Poisoning
- Supportive Care
- Atropine
- 2-PAM
Treatment of acute organophosphate poisoning consists of non-specific measures of decontamination, cardiorespiratory support, and seizure control where applicable (e.g. diazepam). In addition, the specific antidotes atropine and pralidoxime (2-PAM) are employed. Atropine is a muscarinic receptor blocker, which acts to block the organophosphate-induced over stimulation of central and muscarinic cholinergic nerve terminals. Atropine reduces a subset of organophosphate poisoning symptoms: secretions, bronchoconstriction, bronchospasm, and gastrointestinal toxicity. Because it does not bind nicotinic receptors, atropine does not affect muscle weakness, including respiratory muscle weakness. Pralidoxime (2-PAM) is a cholinesterase reactivator (oxime), serving to restore respiratory and skeletal muscle strength. As 2-PAM does not cross the blood-brain barrier, the central effects are not reversed.
Isabella's RBC AChE and plasma cholinesterase were both below the normative defined by the hospital laboratory. Atropine was administered at pediatric dosages as advised by the clinical toxicologist at the poison center. Increases in cholinesterase levels measured 10 weeks later were consistent with a significant exposure to an organophosphate pesticide (greater than 20% or 15% increase in plasma or RBC enzyme levels, respectively).
