| Research | ||||||||
|
Muscular Dystrophy Research Moves Towards Gene Therapy |
||||||||
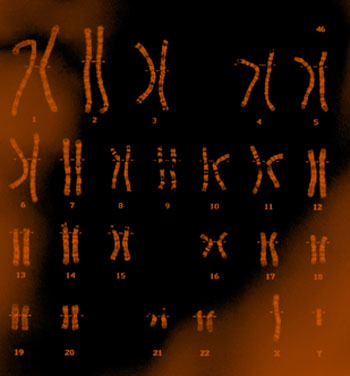
A group of muscular dystrophy specialists around Seattle is forming one of three federally funded centers for research on muscular dystrophies, a set of inherited conditions that all result in muscle weakness and wasting. The center, funded by grants from the National Institutes of Health and the Muscular Dystrophy Association, will work on creating gene therapies for both myotonic and Duchenne muscular dystrophy, as well as on perfecting ways to deliver those therapies to muscle tissue. The group, headed by Dr. Jeffrey Chamberlain, professor of neurology, medicine, and biochemistry, will include other faculty members and researchers at the Fred Hutchinson Cancer Research Center. "I think we have one of the best groups anywhere in the world for dealing with muscular dystrophy," said Chamberlain, who will serve as the center's director. "The research groups will be asking various questions in parallel, and will build the research through a collaborative effort." Having identified genes that can cause muscular dystrophy, either through malfunctioning or shutting down completely, researchers hope to take models of gene therapies shown to be successful in animals and begin applying them to humans. Chamberlain listed the challenges ahead: "What is the best way to put together a synthetic gene to work the way the normal one would? If a gene is put into the muscle will it overcome the problem? How do we deliver that gene to the muscles?" Those problems are being tackled independently, he said, with some groups working on gene therapies using tissue culture cells and mice, and other groups trying to solve the problem of delivery to the muscle tissue that contains the defective genes causing the disease. To complicate matters, the two types of muscular dystrophy they are studying have a major difference: Duchenne is a recessive inherited disease, in which the defective gene doesn't function, while myotonic is a dominant one, featuring a gene that malfunctions by disrupting other cell processes. Replacing the defective gene may be effective in treatment of Duchenne muscular dystrophy, while stopping the malfunctioning gene would be required to treat myotonic muscular dystrophy. "A good analogy of that is that Duchenne is like a car with a broken engine that won't start," Chamberlain said. "Mytonic is like a car with defective brakes, veering out of control." Though having to work on two different problems could make it difficult for researchers to perfect gene therapies for both types of the disease, solving both could help in the long run, because the many types of muscular dystrophy resemble either Duchenne or mytonic. "We're hoping that a treatment for Duchenne would be adaptable for other recessive types of muscular dystrophy, and that a treatment for myotonic would be adaptable for other dominant types," Chamberlain explained. Tackling such a complex project will be helped by the wide array of people in the Seattle research group. It includes Dr. Stephen Hauschka, professor of biochemistry; Dr. Stephen Tapscott, professor of neurology and full member at the Fred Hutchinson Cancer Research Center; Dr. Thomas Bird, professor of neurology; Dr. Stanley Froehner, professor and chair of physiology and biophysics; and Dr. Marie-Terese Little, staff scientist at the Fred Hutchinson Cancer Research Center. The center will be funded by a five-year, $6.9-million grant from the National Institutes of Health and $1.6 million in matching funds from the Muscular Dystrophy Association. |
||||||||
|
© 2003 - 2004 UW Medicine
Maintained by UW Health Sciences and Medical Affairs News and Community Relations Send questions and comments to drrpt@u.washington.edu |
||||||||