INDEX
Changing Values
High Cost System
Pressures of Global Economy
Excess Capacity
Use of Technology
Too Much, Yet Not Enough
Pluralistic Health Care System
Market Driven Reform
Market Driven Reform 2000
Pharmaceutical Industry and Drug Regulation
Health insurance premiums
Congress and State Legislation Address Issues
Medicare Going Broke
Washington State Law
Shift in Tobacco Attitude
The New Marketplace and its Effects on Infection
PROS
CONS
Questions for the future
Readings

INTRODUCTION
Changing Values: Traditional v. More Progressive
There is a shift in the United States healthcare system, from values that are more traditional to values that are more current. The traditional values are:
- Seeing the specialist and ordering anything you want whether it is cost effective or not (or pay per service)
- Technologically driven-anything at all costs if it is necessary,
- Institution based-focusing on the individual and giving that individual patient anything they want versus how to take care of society as a whole versus society based health,
- Treatment versus prevention (we do not utilize prevention to its optimum degree.)
- Individual providers versus team approach, and competition versus cooperation. How do you get all these public/private entities to work together.

US Healthcare, circa 1981
If you look at healthcare in the United States over the last 20 years, you see physicians defining the rules of the system. They bill insurance, both public and private. When there is a short fall, you collect more money, either by raising premiums or taxes or whatever your financing mechanism. The patients and physicians at this point had unlimited choice.
High Cost System [Slide]
If you look at what we spend in the US for healthcare in comparison to other industrialized countries, you can see that it is phenomenal. The US spends 14% of the Gross Domestic Product (GDP) compared to 10% for Canada and 7% for the United Kingdom. This is higher than any other country. Furthermore, they are starting with a much lower GDP than we are in the US which further reflects on the total resources being funneled into the treatment of illness.
High Cost System 1992-1994 [Slide]
Between 1992 and 1994, only one other country in the world, Germany, saw their costs go up as a proportion of their Gross Domestic Product. Why would that have occurred? The German increase is most likely due to the reunification of Germany and integrating the East Germans into the healthcare system. We do not have that as an explanation in the US.

Pressures of Global Economy
We are functioning in a global economy in this world, and business in the United States is very powerful. Anything that increases the cost of goods and services in business will come under scrutiny. Many of you know that health care insurance originally started as an employment benefit when there was a wage and price freeze after World War II. People received health insurance as a way to attract people to jobs because they could not raise the salary. That made businesses more competitive for a scarce work force in World War II. Now just the reverse phenomenon is happening when it comes to healthcare costs. Because our costs are so much higher than they are in other countries, the ability to provide healthcare insurance through business is actually decreasing businesses' competitiveness in the marketplace.
What is Fueling Change?
What is fueling these changes? The buying and selling of healthcare in the United States at 15% of the Gross Domestic Product as opposed to 12% give us a net 20% difference on a trillion dollars. The recoverry of this $200 billion per year is necessary, business claims, if the United States is going to function well in the global market.
Excess Capacity
One of the hallmarks of American healthcare is that we have excess capacity. Some of this came about because of Medicare regulations that gave incentives for building hospitals. If you look at hospital beds in 1993, in cities like New York, Chicago, Los Angeles, Philadelphia, and San Francisco, the supply is 40-50% greater than current demand. Why would that be? Reasons include the focus on costs, shortening the length of stay, not admitting people who do not need admission to the hospital, and given use of certain outpatient therapies. For example, it is not unusual for people who used to get their chemotherapy in a hospital bed to now get it in a more user-friendly outpatient setting. This is clearly a trend that is here to stay. I think what we have is basically a 40% surplus of hospital beds in the United States.

Use of Technology
It is interesting and often quoted that there are more MRI scanners in Orange County, California than in all of Canada. Now do people in Orange Country really need more MRI's than all of Canada. This phenomenon shows up in other areas as well-open heart surgery, , cardiac cathaterization, and heart transplants.
In Germany they have sickness funds, and there is an annual process that goes on between the providers of services and the administrators of the sickness funds where they set the records for these types of procedures. Likewise, because Canada has a universal system, they can impose cost controls centrally in these particular areas. In these confines the unit cost of the procedure is less, but also built into the system is that some of the risk is shifted to the providers because they do not get extra money in either of those system once they go above a particular number per year.
[Question: I thought that in the United States, we have more specialists than we have people who need specialized surgery, for instance, so people might come from Canada to have surgery here?]
One of the questions that always comes up when you compare US and Canadian healthcare is, are Canadians who are tired of the queue coming to the United States to get some of these services. The most recent surveys suggest that just a miniscule portion of Canadians come here to get these types of services. The big thing about Canada's service is that prescription coverage is not built in to the national umbrella, so province by province they decide on a plan for prescription coverage. They have special AIDS drug programs to cover their people just like we do here. These are the trade-offs. The German system does not emphasize preventive health measures compared to the United States. That has not been a value in the German system, but they do have something else that is fascinating: if you are reacting to stress and your doctor thinks you need a couple of weeks at a German spa, you get baths and massages. That is covered by their health insurance. Now why would that be? The spa industry in Germany is famous. It is world renown. They lobby their legislature. They get it covered as a health benefit. That is where a different history of a country plays out. I would much rather have a spa visit than a cardiac cath or an MRI if I have the choice.

Too Much, Yet Not Enough
In the United States, we have this paradox of too much and yet not enough. Excess supply of hospitals, laboratories and specialists in the face of 15% uninsured. Rapid availability to expensive technology long before we can pay for its application to the whole population or before we even know how to use it. Underutilized prevention.
[Question: Does that figure of 15% include people who are considered underinsured?]
It increases the figure from about 39 million who are continuously uninsured to 61 million if you look at uninsured for any period of time during that year. Then you have other issues like the definition of underinsurance. One definition I have heard is if your health expenses require more than 10% of your income and out of pocket expenditures then you may fall in the underinsured.
Pluralistic Health Care System

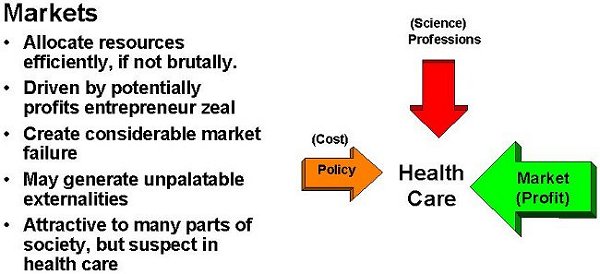
Market Driven Reform
If you look at the healthcare in the United States, what do we have now? What sort of healthcare reform do we have? It is market driven reform as opposed to regulatory reform. Regulatory reform is when the government makes laws, pays the bills, and gives incentives for the system to carry out specific duties. Market reform is when you allow business and competition to change the system in which you operate. Markets do certain things very well, and do them better than regulation in some cases. They efficiently allocate resources, they are driven by profits and zeal. It is said that if you want something done creatively, have the market do it as opposed to government. Market failure tends to sort out companies by who makes money and who does not. That is how the market answers a lot of these questions. They are attractive in many parts of society, but I think the market system is suspect in healthcare. It is one thing to be selling televisions and have a company go out of business, but it is another to have a major insurer of several million people go belly up. Then what do you do?
Reports from the Front
My favorite healthcare journal is the Wall Street Journal, there is information on all types of mergers and acquisitions. One week a company may be known one way, the next week it may have a totally different name, logo and administrative staff. Locally you have seen it with Group Health, their alliance with Virginia Mason, then their alliance with Kaiser to create a bigger product. All that is market driven.
Market Driven Reform 2000
The truth of the matter is that we have too many health insurance companies. We do not need 3,000 health insurance companies in the United States. The market is not going to support 3,000 separate administrations. They will sort themselves out by competition. By the year 2000, I think most of the healthcare in the United States is going to be managed care. I think you are going to see three or four big systems develop through mergers, acquisitions, and alliances. You will see more public insurance programs, and eventually we may get to a point where we insure everyone.
We have a lot of people in part time positions now. These have families and want a more reasonable schedule. Have any of you had a prescription filled in the last three years? Has the name of your pharmacy changed several times? Mine has gone from Payless to Rite Aid, and they have central processing where all problems get referred. Prescriptions, for the whole country, are processed to one central location. This is hard for local pharmacists. Larger companies are buying them out. The mom and pop pharmacy barely exists anymore. In this city what we see at pharmacies now are long wait lines, change in administration, and staffing. What many people hope the system will become is one of organized purchasers, some element of accountability, expectations for reduced money and capitated expenses, and an integrated network between hospitals and clinics.

Pharmaceutical Industry and Drug Regulation
Do I foresee any regulation of the pharmaceutical industry regarding their mergers and consolidations? If you look at profits last year for the pharmaceutical industry, it was a very good year. The issue of regulation of the pharmaceutical industry is almost like regulating the tobacco industry: they are large, multinational corporations. The United States can regulate a little piece of it, but if you have a US company operating in the United States whose headquarters are located in Great Britain, these issues cut across international lines. The international nature of pharmaceuticals make it a different regulatory event than an HMO, which is purely a US interest. I do not foresee any US regulation of the pharmaceutical industry that is going to dramatically change in the next couple of years.
[Question: What are your sentiments about drug regulation?]
I think if you look at drug development cost to bring a new product to the market, it is about $300 million for research and development. Even considering the advertising and the "educating" of physicians about the new medications, these pharmaceutical companies still make 20% profit. Do you believe that you should be able to make all the money you want off healthcare, or do you think there should be some restrictions placed on the industry? I personally think we are top heavy with the cost of pharmaceuticals right now, and it had the highest increase last year.
[Question: Was there something that changed to encourage the mergers and acquisitions, or is it just the market driven economy?]
The way pharmaceutical industries merge is that they will have one company that has a good infrastructure behind it but maybe not the products that are selling at the moment, and then there is a favorable picture for buyouts. This appears to be more market driven economics. If you regulate the pharmaceutical industry they will stop making new products.
[Question: Many of these companies are part of our retirement funds, so we are benefiting from their profits as well as shareholders.]

Reports from the Front [Slide]
Health insurance premiums. Many of you realize there have been changing trends in health care expenditures in the last year. In 1996 we saw the lowest amount of healthcare inflation, about 4%, in this country's history. Everybody was saying that managed care was working. However much of this is projected on decreasing insurance premiums. They were less in 1995-6 compared to 1992-4, but what else is going on now? Have any of you heard of Oxford Heath? It is a large, for profit, HMO which developed a data system to project their costs. Because of their mergers and acquisitions the company was unable to get that data system online, and they dramatically underpriced their premiums. They suffered a significant financial loss in 1997. Now the question that comes to my mind is how many other companies did this, and are these savings real, or are we going to rebound in a couple of years and be right back to where we were?
Are the Savings Real? [Slide]
Employment-based insurance is an experiment that began in the United States during World War II and will do no more for this country than it is doing right now. We are almost at full employment. We have so few people left to enter the labor force, even the unemployables are considered desirable for particular jobs. We have less than 5% unemployment in the United States. During this time period, we have seen the percent of uninsured steadily increase despite full employment. Why would that be? Certain industries do not insure their work force, and there are part time workers who do not have access to benefits. This is becoming a more common scenario. When people change jobs they risk losing their health care coverage. If an employment-based insurance system were going to solve the problem of access, 1996- 1998 are the years it should happen. It did not, the trends are in the reverse direction.
[Question: Why in the United States do we think that it is the employer who should be providing healthcare and healthcare insurance, as opposed to the government providing the insurance?]
If you look at the values in the United States, the United States has built itself on the principle that making money is a good thing. Business leaders were considered entrepreneurial. I think it is one way to drive an economy and motivate a group of people, and it works very well for certain things. Employment based insurance in the United States got started because of wage freezes in World War II. This was a way to offer a higher salary but not come under the wage freeze. In Germany, in 1888 when they started their first healthcare system, they had a popular leader who was trying to get their workers to stop striking, and their answer was to give universal healthcare coverage to their workers. But the United States has a much different history than the Europe countries. We are rugged individualists and we want to do it on our own without government involvement. The absence of universal government insurance is value driven, people are afraid of the government and their costs.

Congress and State Legislation Address Issues
I want to talk about a few issues that were really dramatic in 1997. Patient choice and the managed care backlash is very active right now all across the country. Over 28 legislatures are trying to regulate managed care, either through prohibiting drive through deliveries, drive through mastectomies, and potentially corrupt political relationships have been exposed.
Medicare Going Broke
The government finally figured out that Medicare was going broke.
We have known that worker to beneficiary ratio was declining. When the Medicare program started in 1965, there were 12 workers for every 1 beneficiary of Medicare during the first year of the program. However as the number of people receiving benefits gets greater, the worker: beneficiary ratio is declining to 2.5 to 1 beneficiary. You now have three people supporting one person as opposed to twelve people supporting one person on the system. I was just shocked when this information came out that they were shocked and suddenly had to deal with Medicare. Duh! Anyone who has looked at these population demographic figures has known this for ten years now.
Balanced Budget Act of 1997
The Balanced Budget Act of 1997 set up a commission to look at Medicare and give a report in two years. However, the Balanced Budget Act of 1997 happened this summer with many negotiations held behind closed doors. All of a sudden we now have a children's health insurance program. We were now going to extend Medicaid or a state-run Medicaid-like program to children and families under 200% of the poverty level. The Medicare Choice system was established, which creates a two tier Medicare system. The wealthy will pay extra for some conveniences that they had in Medicare. People without means are going to be forced into an HMO because fee for service is going to be proportionately more expensive. Under the Medicare Choice program people can enroll and disenroll so if you become ill you can disenroll and return to the fee for service model.

Washington State Law
In 1995, Washington State legislature mandated the inclusion of complimentary or alternative care into health care payment plans. It permits every category of healthcare provider who is licensed to provide healthcare services if they are within that provider's scope of practice. Providers have to abide by standards of utilization review and provide cost effective and clinically efficacious health services. The status of this is on appeal, because the insurance companies neither liked the interpretation of the law by the insurance commissioners office nor the vagueness of the way it was written. It validates chiropractors, naturopaths, acupuncturists and other disciplines which traditionally have not been integrated into western medicine.
Shift in Tobacco Attitude
Why do I consider this a health related event? Because tobacco smoke is one of the biggest cofactors for respiratory, middle ear infections, and chronic diseases. You could dramatically improve the health of the whole population, lower your reliance on antibiotics, by getting rid of smoking and second hand smoke.
[Question: Are they still subsidizing tobacco farmers?]
Yes, they are still subsidized. Washington State Attorney General, Christine Gregoire, is one of the key authors of the public health portion of the tobacco settlement which Congress is now fighting.
Do you all know why they want a settlement as opposed to just passing a law?
One they want to stop tobacco advertising to kids, and so the tobacco companies would have to give up their First Amendment rights. You cannot pass a law that forces someone to give up their rights. The tobacco settlement as it is currently written reduces their liability. According to Christine Gregoire, this suit is not about money it is about the tobacco industry giving up their unfair business practices of advertising to kids.
The New Marketplace and its Effects on Infection

PROS
Decreased Hospital Use
The healthier patient who does not need to be in the hospital would not be exposed to the sicker person's bacteria. This could reduce the number of hospital acquired infections and reduce the number of resistant bacteria. In the US healthcare system, it is estimated that 1-3% of healthcare expenditure if for so called "medical misadventure," nosocomial infections and iatrogenic illness.
Better Indications for High Tech Medicine
There is a current study looking at the efficacy of bone marrow transplantation in Class IV breast cancer. Part of the impetus for this study was because of the legal battle between the insurance industry and persons with this type of cancer.
Better indications for surgery.
Certain outcome studies showed that those who went to the chiropractor did just as well as those who had back surgery.
Commitment to Outcomes
The commitment to outcome measurements in the United States healthcare system is very sincere, and is one way that we are ahead of the British, the German and the Canadian systems. We have a commitment to the health employer data information set, which includes immunizations, HIV counseling, and other screening tests. The focus on quality and outcome is one of the biggest advantages in the new marketplace.

Sincere Focus on Prevention
I think the focus on prevention is sincere and is increasing in the United States. We are looking at what makes one healthy and happy: lifestyles (50%), genetics (20%), environment (20%), and the medical care system (10 to 15%). However, in the United States, we spend 97% of our dollar for medical care as opposed to spending it in other areas. The more we can integrate smoking cessation programs, preventive measures and environmental cleanup, into our overall budget, the healthier and less dependent on curative medicine our population becomes.
Controlling Costs
If healthcare costs were controlled, we might have some money left over to inspect food, improve the water supply or sanitation, and improve vaccination rates.
Integration of Complimentary Care
Integration of complimentary care could lead to more rational use of antibiotics. Overall, the individual would feel like they are doing something for themselves. There is no outcome data to suggest that alternative therapies are effective. There is outcome data which shows that antibiotics for a cold does not help.
[Question: How regulated are these herbal remedies?]
They are not well regulated. I think most of the studies have tried to standardize as best they can with a theoretical active ingredient, but that is very expensive to do. Seeing some government research dollars to look at the herbal remedies are exactly what we ought to do. We need good science and placebo controlled trials. The government can always regulate these substances. Most of the herbal remedies are not patentable because you cannot have an ownership of a natural product. It would be more a matter of brand preference and advertising than it would be the ability of one group to gain exclusive control over a compound.

Mergers and Regionalization of Health Plans
Mergers and regionalization of healthcare plans and use of central laboratories would make disease reporting and surveillance easier. It would be easier to make sure that all the E.coli 0157, tuberculosis cases, and gonorrhea cases were reported. A central lab would assist in this process.
Drug Formularies
If they are appropriately organized, you could preserve the efficacy of your newer antibiotics. Drug formularies do put a barrier on prescribing the newest and usually costliest antibiotic because they require utilization review for additional approval.
Use of Treatment Guidelines
Use of treatment guidelines for infectious disease and better information of systems could reduce error and overprescribing, if people are very clear on the guidelines and follow them. For example, how many of you know about the Oregon health plan? They passed a law to make a prioritized list of preventive and comfort related services. They approved spending of these items starting at the top of the list and moving down until the funding is depleted. Treatment of a cold, for instance, is not on that list. You can be diagnosed, but if you get an antibiotic for a cold, you would not get paid under their fee for service prioritization of benefits. This is one of the few states that has done this in an organized fashion.
The good news is that at least in Washington State, we have about 10% uninsured in this state. What would it be if you lived in Texas? Twenty five percent! In Oregon, their uninsured fell from 17% to 10% when they did this prioritized list and made Medicaid available to everybody who was below the federal poverty level.
[Question:is there is a big push for getting insurance to pay for pap smears.]
There is controversy about how often you should do a pap smear, and much of the discussion has been industry driven. It is important to recognize that what we hear about pap smear screening may not be balanced reporting even though we know it should be covered under health insurance plans. The reason pap smears are recommended annually is because most women do not abide by that and hopefully women will at least get a pap smear done every 3 years. This is probably what women need in a cost effective model.

CONS
Co-pays and Deductibles
Co-pays and deductibles are an inherent part of this market driven system. They may be a disincentive for clients to receive necessary services such as STD screening, pap smears and other preventive measures. We want clients to receive these preventive health care measures. If you charge these clients for each visit of this nature they will be less likely to comply.
Integrated Data Systems
When we talk about data systems, for example making surveillance available for reporting, it will be years before these systems actually function. Only one HMO in Washington state has an integrated disease reporting data system currently. These types of systems "scare" people. They do not like the idea of integrating an infectious disease report into a large data system.
Antibiotic Resistance Testing
Testing for antibiotic resistance is going to be less common and less attractive as cost effectiveness models come into play. For example, the newer tests for gonorrhea use DNA probes, which are cheaper than culture. However, you cannot do antibiotic resistance testing from a DNA probe. Therefore we could lose the ability to track resistance patterns for specific diseases.

Empirical Therapy
Empirical therapy is cheaper than diagnosing the infections. For example, a diagnostic chlamydia test costs $10 and the treatment (doxycycline) costs only $2, it would be cheaper just to give the treatment medication than to diagnose the condition. The problem, however, is that you also need to treat the sexual partners. Without a specific diagnosis this impairs your ability to have the appropriate people involved in the care and management of the partners in addition to the initial client.
Drug Development
Drug development could actually be inhibited if costs were truly controlled. There is a lot of room from our current situation with development costs to definitively inhibit profit in the system.
High Cost of Testing
The HIV p24 antigen test, which has a high cost, was rapidly integrated into the blood banking system. The estimated cost to prevent 10 new HIV infections using this test was approximately $100 million. On a system wide view, this rapid growth of technology may not be cost efficient or effective. We need to choose how to spend the dollars.
Public-Private Shift
One local example is the privatization of public health functions for the Tacoma-Pierce County Health Department. They contract with private providers in their community for their TB services, STD prevention and other services that operated at the health department. The structure of the private model may be substantially different from the public model. The public model screens everyone, does contact tracing, and uses on site distribution of medications. The private model usually hands out prescriptions, tells patients informally to get their partners seen and uses limited screening tools. In addition, private providers do not report as thoroughly as public providers, making it difficult to evaluate the efficacy of this change. These are the big differences. One is not right or wrong, you just have different outcomes when you look at the two models. There are no long-term evaluations of these privatization models. It would be helpful to do sentinel studies to evaluate the long-term results of this modeling.

Questions for the future
Ending the list of "con" items are several unanswered questions. For example, who will take care of the uninsured? What happens to legal immigrants denied Medicaid? Do we think the government should cover these individuals? It seems clear that our current marketplace will not pay for these groups.
Where do new and expensive treatments fit into the marketplace model? For example, protease inhibitors are expensive, costing $1000 per month. Though they may be lifesaving they will definitely increase costs. The next cost issue item will be liver transplantation for those with chronic Hepatitis C infection.
The long-term outcome of hepatitis C is liver failure and a subgroup of those infected will be transplant candidates. Currently we are limited in the number of transplants because the supply is limited. If technology advances to be able to utilize parts of liver and increase the transplant capacity, discussion about rationing will evolve.
 Readings: Mainous, A.G., et al. "Antibiotics and upper respiratory infection: Do some folks think there is a cure for the common cold?" Journal of Family Practice, Vol. 42, No.4, 1996, pp.357-361.
Return to Title PageHOME | List of Lectures |