Healing & Therapy
Studies in health care settings show a link between nature and healing. Nature contact may serve to supplement or augment medical treatment and therapy. Both passive exposure to landscapes and more active interactions with nature provide mental and physiological benefits that contribute to healing and therapy.
Fast Facts
- Hospital patients with plants in their room display less fatigue and pain, shorter hospitalization, less anxiety, and higher hospital and room satisfaction.5
- Patients with chronic musculoskeletal pain who participated in a 4-week horticultural therapy program experienced an increase in mental and physical health as well as an improved ability to cope with chronic pain.21
- A study of children with Attention Deficit Disorder who played in windowless indoor settings had significantly more severe symptoms than those who played in grassy, outdoor spaces.24
- Patients with clinical depression who participated in routine therapeutic gardening activities experienced a reduction of severity of depression, and increased attentional capacity, benefits that lasted up to three months after the program ended.32
- Gardening may be a preventative measure to help reduce the onset of dementia49; gardening on a daily basis was found to reduce risk factors for dementia by 36%.50
- Dementia patients who have access to gardens are less likely to display aggression or experience injuries41 as well as improved sleep patterns, balanced hormones, and decreased agitation.101
- Studies have shown that participating in activities and/or interacting with natural environments can ameliorate and help stave off attentional fatigue both before and after breast cancer treatment or surgery.33
- Ever more studies confirm the relationship between neighborhood open space and physical activity.94 A study calculated a $2,200 reduction in average annual healthcare charges per adult for those who had been sedentary, but became active.99
Contents:
> Nature in Hospitals * Nature in the Room * Healing Gardens and Therapeutic Horticulture > Horticulture Therapy > Mental Health, Function and Therapy * Children and Attention Deficit * Depression * Cancer Patients * Psychiatric Patients * Dementia * Elder Care > Physical Health & Therapy * Obesity and Active Living * Stress * Disabilities and Elder Care > Recovery, Resilience and Rehabilitation * Crisis Recovery and Resilience * Military Service and Stress Disorders * Prisons and Jails > Nature & the Healthcare Industry * Prescriptions for Parks & Trails * Insurance > References *cite: Wolf, K.L., S. Krueger, and K. Flora. 2014. Healing and Therapy - A Literature Review. In: Green Cities: Good Health (www.greenhealth.washington.edu). School of Environmental and Forest Resources, College of the Environment, University of Washington.
Nature in Hospitals
In Europe the first hospitals were in monastic communities, where gardens played an essential role in the healing process.1 As medical science and technologies have progressed the more indirect connections between nature and the healing process are often overlooked.1 Recent research suggests that access to natural features at a care facility aids healing and recovery from a variety of physical and mental ailments.
Nature in the Room
Exposure to plants, natural views and nature imagery plays a positive role in recovery and pain management inside care facilities. An early study by environmental psychologist Dr. Roger Ulrich revealed that gallbladder surgery patients recovered faster and used fewer strong pain medications when their room window faced a natural view rather than a brick wall.2 The patients had, on average, a one-day shorter hospitalization and fewer negative comments from nursing staff.2
A more recent study suggests views of natural surroundings may benefit male and female patients differently. Men with obstructed views of nature demonstrated a decline in mental health, while women with obstructed views appeared to have a greater decline in physical health.3
Regardless of the view, windows in hospital rooms also allow for the potential benefits of natural sunlight. Spinal surgery patients exposed to bright, naturally-sunlit hospital rooms experienced significantly less stress, and used less pain-killing medication (thus reducing costs of care) compared to similar patients who were not exposed to intense sunlight.4
Why might simply viewing nature ease pain and encourage healing? New insights from neuroscience suggest that nature experiences are positive distractions that help a person to refocus their attention. Increased focus on other inputs increases pain thresholds and tolerance, leading to improved coping and healing strategies.10,11,12
Healing Gardens and Therapeutic Horticulture
Acting on research findings, healthcare facilities such as hospitals, nursing homes, and rehabilitation centers have begun to install healing gardens for patients, visitors and staff. In addition to contributing to the healing and therapy process, gardens are intended to help address the mental stress, information overload, and emotional distress that visitors may experience when assisting a loved one in a healthcare facility.13,14 Gardens may also serve as restorative environments for healthcare employees.15,16
Studies inform garden design by evaluating how specific pathways, plantings, and other features influence levels of interaction with the garden, duration of stay, and therapeutic benefits. Hospitals and care facilities may design healing gardens for a target population and purpose, such as Alzheimer's patients or children with physical disabilities.16 Observations of patients undergoing treatment for stress-related diseases suggests that gardens are most beneficial when they provide distinct areas for passive reflection and emotional recovery, as well as social interaction, physical activity, and sensory stimulation.17
A survey of visitors to four hospital gardens found that respondents most commonly mentioned multiple nature elements of gardens - trees, greenery, flowers, and water - as having positive benefits on their moods.18 A study of a pediatric hospital’s healing gardens demonstrated that having play features, pathways, and shading encouraged higher levels of physical activity for visitors and children. Meanwhile staff preferred garden areas that provided visual and auditory privacy.15 Other studies support the need for distinct garden spaces for staff - spaces where they can enjoy breaks without encountering visitors and patients.14
Horticulture Therapy
Providing gardens and other natural settings for the general purpose of facilitating healing and wellbeing is known as therapeutic horticulture, including the examples provided above. Horticultural therapy is the use of prescribed nature activity or experience by a trained professional to aid recovery from specific mental or physical ailments. Therapeutic treatment can take place in healthcare facilities or in community settings. Horticultural therapists engage their patients in gardening activities as individuals or in group settings. They guide activities that provide physical exercise or therapy, social interaction, or cognitive development to meet clinically defined goals.19
A systematic review of over 240 scientific studies found reliable evidence to support horticultural therapy as an intervention for a variety of conditions, from cerebral palsy to schizophrenia.20 In one study patients with chronic musculoskeletal pain who participated in a 4-week horticultural therapy program experienced an increase in mental and physical health, as well as an improved ability to cope with chronic pain.21
After just one horticultural therapy session, patients recovering from cardiac surgery experienced marked improvement in their mood, and stress reduction.22 Beyond treating acute health conditions, research shows that horticultural therapy can also benefit individuals trying to overcome emotional or physical trauma. In one study adults with diagnosed depression participated in a therapeutic horticulture program and showed significant beneficial change in mental health aspects of anxiety, mood, and depression.23
Mental Health, Function, and Therapy
Children and Attention Deficit
Over 2 million children in the U.S. have been diagnosed with attention-deficit/hyperactivity disorders (ADHD). Such a child has reduced attention capacity, which can have detrimental effects on social, cognitive, and psychological growth. Studies at the University of Illinois have tested nature-based activity and ADHD outcomes. In the first study parents judged that attention deficit symptoms were more manageable after doing activities in green settings than after activities in other settings (Table 1). Also, the greener a child's play area, the less severe his or her attention deficit symptoms; children who played in windowless indoor settings had significantly more severe symptoms than those who played in grassy, outdoor spaces (with or without trees). Though the greenness of a child’s home was unrelated to their ADD severity, more green in their play setting was related to better outcomes.24
In a follow up study green outdoor activities reduced symptoms significantly more than did either built outdoor activities or indoor activities.25 A third study found that children with ADHD concentrated better after a walk in the park than after a downtown walk or a neighborhood walk. Exposure to ordinary natural settings in the course of common after-school and weekend activities may be widely effective in reducing attention deficit symptoms in children. “Green time” may be an important supplement to traditional medicinal and behavioral treatments.26
Depression
Depression, like stress, occurs at any age and can be ameliorated through improving social connections (to decrease the feeling of isolation) and exercise,27both of which are encouraged by the presence of nearby green outdoor spaces. A multi-study review found that those who exercise in natural environments reported greater enjoyment and satisfaction and declared a greater intent to repeat the activity at a later date. Compared to being indoors, exercising in natural environments was associated with more positive mental states, such as greater feelings of revitalization and positive engagement, decreases in tension, confusion, anger, and depression, and increased energy.28
Exposure to natural light, in particular morning light, appears to be effective in treating patients with seasonal affective disorder (SAD).31 Outdoor walks are one way to access natural lighting.
Studies investigating major depression disorder (MDD) have shown that an exercise program can be just as effective as antidepressants in reducing depression among patients,29 and that a 50-minute walk in a natural area (compared to a built setting) may increase memory span and elevate moods.30 Patients with clinical depression who participated in therapeutic gardening activities for 3 months experienced a reduction in severity of depression and increased attentional capacity that lasted up to three months after the conclusion of the program.32
Mental Stress and Cancer Patients
Clinical reports note a loss of concentration and increased distractibility in patients undergoing cancer treatment, including those with breast cancer.33 There is a correlation between cognitive function and cancer diagnosis. A decreased ability to direct attention may begin before treatment actually starts. Treatment planning following diagnosis can be mentally demanding and stressful, leading to attentional fatigue.33
Participating in activities and/or interacting with natural environments have been found to ameliorate and help stave off the attentional fatigue both before and after breast cancer treatment or surgery.33 A qualitative study compared the meaning of gardening in daily life for those with and without cancer and found that - though dependent on past gardening experiences, individual interests, and current circumstances - gardening can be used as a potential coping strategy for stressful life experiences.34
Further, nature may have a preventative effect on cancer generation and development. Studies of people doing 'forest bathing' trips in Japan show an increase in natural killer cell activity, the number of beneficial cells, and the release of anticancer proteins.35
Psychiatric Patients
Studies investigating the effects of nature and gardening on psychiatric patients display a range of results, from general mood improvement to specific illness. For example, horticultural therapy was effective in decreasing the levels of anxiety, depression, and stress among participants diagnosed with psychiatric illness.36 In another study placing flowering plants in a ward increased socializing and food consumption in severely withdrawn schizophrenic patients.37
The smells, colors, and handling of soil by patients during horticulture activities may be particularly important and can improve life satisfaction, well-being, and self-concept in mentally ill patients.38
Finally, when comparing intensive therapy patients in rooms with translucent windows to ones without windows, those patients with windows had less sleep disturbance, improved memory and orientation, as well as fewer hallucinations and delusions, providing more normalcy and connection to the outside world.39
Dementia
Dementia patients experience multiple disorders, including memory impairment, intellectual decline, temporal and spatial disorientation, impaired ability to communicate and make logical decisions, and decreased tolerance to high and moderate levels of stimulation. Dementia care poses a financial burden on society on par with cancer and heart disease, with the total annual cost of care in the U.S. estimated to be $157 to $215 billion (in 2010).40
Recent studies report that, in both adult day settings and nursing homes for those with dementia, there are positive correlations of well-being and enhanced competence following passive and active interaction with nature. Dementia patients are sensitive to environments and natural surroundings can provide prosthetic support to compensate for limited cognitive capabilities.41 Studies note decreased aggression, improved socialization, and increased social competencies, as the natural environment provides cues of what is comfortably familiar due to reminiscence and nostalgia.42 Additionally, outdoor nature-based activity contributes to improved sleep patterns, balanced hormones, and decreased agitation in dementia patients (Figure 1).43,44
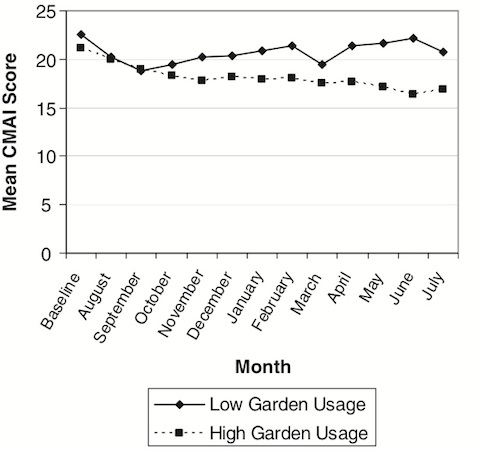
Figure 1: Garden usage is associated with reduced agitation in dementia patients (CMAI is a measure of agitation)
Overall quality of life measures for dementia patients, their family members, and staff appear to improve at long-term care facilities with therapeutic gardens.45 Access to gardens has been shown to reduce incidents of dangerous behavior and aggression for dementia patients (Figure 2).41 Gardens can also evoke memories that reconnect patients to the real world.46 Additionally, residents with high use of wander gardens have a decreased use of high-dosage anti-psychotic medications.47 Gardening activities may help improve mobility and dexterity, confidence and social skills in dementia and stroke patients.48 Finally, gardening can be used as a preventative measure to help reduce the onset of dementia49; gardening on a daily basis was found to reduce risk factors for dementia by 36%.50
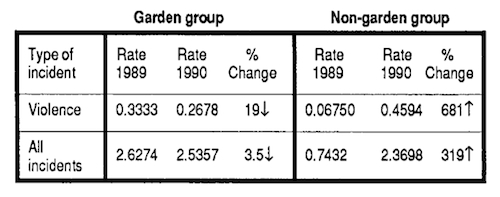
Figure 2: Comparison of behavioral incidents with dementia patients in institutions based on garden access (over a one year period)
Design for dementia care is important; there is a distinct association between measures of health and how spaces are designed.51 A space needs to promote functionality and well-being, but also be safely open and free.52,51 Recommended design features for outdoor spaces for dementia patients include: looped pathways; tree groves or sites to act as landmarks for orientation; non-toxic plants; even, well-lit paths with handrails; seating areas with the illusion of privacy; and low key fragrances and color to soothe, rather than negatively stimulate.41
Elder Care
Some of the earliest research about nearby nature and human benefits focused on benefits to the elderly. Studies continue as most industrialized nations have aging populations, and face increased need for providing care as people get older. The University of Helsinki summarized the potential mental, emotional, and social benefits experienced when the elderly participate in gardening and horticulture (Table 2).48
Physical Health & Therapy
Obesity and Active Living
The CDC reports that more than one-third of U.S. adults (35.7%) are obese, and the estimated annual medical cost of obesity in the U.S. was $147 billion in 2008 U.S. dollars. Obesity leads to increased risk of chronic diseases, such as asthma, Type II diabetes, cardiovascular disease, some cancers, osteoarthritis, and can effect body image, social stigmatization and discrimination, which can lead to depression.53
One lifestyle change that can help with weight control is routine physical activity, sometimes termed active living. Studies found that the creation or improvement of a park or open space was shown to lead to a 25.6% increase in nearby residents exercising three or more days a week54 and a 48.4% increase in frequency of physical activity.55 Also, park access increases aerobic capacity by 5.1%, reduces body fat, improves flexibility, and increases perceived energy.55 Aerobic exercise in a natural environment may lead to greater gains in lowering blood pressure, stress, and depression compared with exercise in non-green urban settings.56,57
Stress
People experience stress at all ages, however it is especially prominent later in life due to physical, psychological, and social changes that include chronic disease, disability, loss of loved ones, and fixed incomes.58 Stress can affect people’s perceptions of their well-being, causing them to have diminished mental health.58 Physical activity has also been linked to improved mental health and stress coping.59 Studies have connected park use to decreased stress levels and improved moods. In one study participants showed fewer stress symptoms the longer they stayed in the park.60
Simply viewing nature can help. Following a stressful activity, young adults sitting in a room with a views of trees showed reduced blood pressure and feelings of stress compared to those in a viewless room.61 Lab and clinical investigations have found that within five minutes of viewing a nature setting positive changes in blood pressure, heart activity, muscle tension, and brain electrical activity occur.62,63
A study of brain activity, using alpha rhythms as a measure, showed that participants were most awake and relaxed while looking at plants with flowers, rather than empty pots.64 In a companion study EEG (electrical brain activity) indicated more relaxation when viewing greenery compared to looking at a concrete structure.65
Disabilities and Elder Care
Horticultural therapy can increase self-esteem, making people with learning disabilities consider themselves more desirable and confident than before.66 Much of the research of green effects on mobility, dexterity, and disabilities focuses on the elderly. Preliminary studies have reported the benefits of horticultural therapy and garden settings in reduction of pain, improvement in attention, lessening of stress, modulation of agitation, lowering of as needed medications, antipsychotics and reduction of falls.67
Outdoors gardening or activities improves exposure to sunlight, which can increase bone density, due to increased vitamin D absorption,68 as well as improves circadian rhythms and sleep cycles.69 Gardening activity can also help increase bone mineral density70 as well as improve musculoskeletal function.71
Recovery, Resilience, and Rehabilitation
Crisis Recovery and Resilience
Efforts to recover and rebuild often follow soon after a major disaster or crisis, at both personal and community levels. Nature can have a rehabilitating effect on individuals. A study of people recovering from significant personal crises found that experiences in nature had a powerful positive influence on recovery.72 Individuals place positive symbolic value on trees and natural landscapes after a catastrophe;73 familiar, green, restorative places can ease trauma and discomfort.74
Historically, gardening was an expression of the will to be “resistant and resilient” during World War I, as gardens were created by soldiers in battle trenches. The book, Defiant Gardens,75 describes how people created gardens within the extreme conditions of World War II: Jews in Warsaw ghettos, prisoners of war, and Japanese-Americans in internment camps.
The act of working together as a community to build something and help it grow can improve attitudes and social ties, heal and create new memories, and provide an outlet for grief.76 The Sunflower Project in New York City, an interim, living memorial before the official 9/11 memorial could be constructed, was a movement to memorialize the loss of loved ones through planting and nurturing new life.77
Community greening can encourage diversity and facilitate reconciliation between ethnic and social groups, such as programs where Jews and Palestinians plant trees together in Israel.78 Additionally, community greening can address economic and environmental damage following events like tsunamis and hurricanes, by providing food and restoring the landscape.78 Gardening can also aid in the resettlement process as it has been shown to help asylum seekers and refugee families cope with the trauma of relocating and acclimating to a new environment,79 especially as gardening can provide the opportunity to restore cultural traditions and familiar foods.
Military Service and Stress Disorders
Those that have been or are in the military may experience emotional and psychological trauma in addition to physical injuries. While little conclusive research that has been done to date, nature shows promise as a therapy and treatment.
A study of veterans who participated in multi-day, group-based outdoor recreation outings with the Sierra Club reported significant increases in well-being, social functioning and life outlook, particularly for those veterans who had reported severe on-going health problems.80 Veterans suffering from chronic post-traumatic stress disorder who participated in a 12-month weekly sailing program experienced a reduction in symptoms and improvements in daily functioning, hope, and perceived control over their illness.81 Veterans who participated in an Outward Bound recreation program, compared to more traditional therapy sessions, had inconclusive quantitative results, but showed increased enthusiasm for the program, trust of the treatment staff, and improved feelings of self-control of behavior and depression as well as physical abilities.82
While most nature therapy programs for veterans are conducted in places outside cities, nearby nature may also provide benefit. A study of veterans participating in a community gardening program reported that they gained a sense of purpose; had something to look forward to; felt relaxed, secure and safe; learned new skills; and were able to share new knowledge and skills with others.83
Prisons and Jails
Drawing from a small set of studies about gardening projects within prisons, nature may be a tool for rehabilitation. Inmates have shown enhanced self-esteem and sense of accomplishment,84as well as decreased hostility and a feeling of experiencing success.85 Female inmates who participated in a Master Gardener program reported higher self-esteem and life satisfaction, particularly those who previously abused drugs or alcohol.86
The benefits of these programs may extend to life after release. Participants in the GreenHouse Program, a horticulture program at Rikers Island Prison (New York), had a recidivism rate (number of released criminals that commit another offense and return to prison) of 25%, compared to the overall recidivism rate of 65%.87 The Sustainable Prisons Project (based in Washington State) facilitates conservation science research within prisons. Offenders raise endangered frogs and butterflies, propagate native plants for prairie restoration, assist with beekeeping to learn about bee colony collapse, and participate in research. While the program’s benefits have not been empirically assessed, informal evaluations of the program suggest that inmates become motivated learners.88
Studies of youth offenders offer hope for behavioral improvements. Studies show that youth offenders involved in horticulture training learn about responsibility, social skills, problem solving, and better decision-making.89 Researchers concluded that such a program can be a tool to improve social bonding, and be effective in causing attitude changes and increasing perceptions of self-image, pride, and ability to succeed.90 Similarly, a study of a gardening program at a juvenile detention facility found improved social skills, increased self-esteem, anxiety reduction, increased patience, and an improved ability to delay gratification.91
Nature & the Healthcare Industry
Prescriptions for Parks & Trails
Ever more studies confirm the relationship between neighborhood open space and physical activity.92 Even short doses of outdoor exercise in natural settings are shown to improve mental health.93 Researchers have yet to define exact dosages and frequencies for outdoor activity to address specific ailments. Yet, organizations and health care providers now recognize the benefits of nature activity and some are working to develop goal-oriented “prescriptions” for individual use of parks and trails.
For example, New Mexico’s Prescription Trails program equips health care providers with tools for motivating patients to use trails for walking and wheelchair use. Patients receive individualized recommendations for duration and frequency of trail use based on their physical condition.94 The Golden Gate Parks Foundation launched a similar program, encouraging health care providers to issue “park prescriptions” to establish and monitor goals for outdoor activity as a preventative health measure for patients.95
Insurance
Traditionally, insurance reimbursements are spent on treatment of symptoms rather than exercise or lifestyle interventions that could prevent the cause of disease. Not long ago fewer than 14% of primary care providers regularly give any form of counseling on exercise.96 A 2003 study calculated a $2,200 annual reduction in average annual healthcare charges per person for individuals who had been sedentary, but became physically active (exercising three or more days a week).97
Insurance companies are recognizing the value of connecting customers to the benefits of active lifestyles. SeeChange Health Insurance, for instance, reimburses state parks fees for customers who visit parks in California and Colorado.98 Empirical analysis of such programs are still forthcoming, but insurance companies may find that incentivizing outdoor activity pays off for customers, communities, and insurers.99
Project support was provided by 1) the national Urban and Community Forestry program of the USDA Forest Service, State and Private Forestry, and 2) the Pacific Northwest Research Station, USDA Forest Service. Summary completed August 1, 2014.
References
1. Grinde, B., and G.G. Patil. 2009. Biophilia: Does Visual Contact with Nature Impact on Health and Well-being? International Journal of Environmental Research and Public Health 6:2332-343.
2. Ulrich, R.S. 1984. View Through A Window May Influence Recovery From Surgery. Science 224:420-421.
3. Raanaas, R.K., G.G. Patil, and T. Hartig. 2012. Health Benefits of a View of Nature Through the Window: A Quasi-experimental Study of Patients in a Residential Rehabilitation Center. Clinical Rehabilitation 26, 1:21-32.
4. Walch, J.M., B.S. Rabin, R. Day, J.N. Williams, K. Choi, and J.D. Kang. 2005. The Effect of Sunlight on Postoperative Analgesic Medication Use: A Prospective Study of Patients Undergoing Spinal Surgery. Psychosomatic Medicine. 67:156-153.
5. Park, S.H., and R.H. Mattson. 2009. Ornamental Indoor Plants in Hospital Rooms Enhanced Health Outcomes of Patients Recovering From Surgery. Journal of Alternative and Complementary Medicine 15, 9:975-980.
6. Park, S.H., and R.H. Mattson. 2009. Therapeutic Influences of Plants in Hospital Rooms on Surgical Recovery. HortScience 44, 1:102-05.
7. Diette, G.B., N. Lechtzin, E. Haponik, A. Devroates, and H.R. Rubin. 2003. Distraction Therapy with Nature Sights and Sounds Reduces Pain During Flexible Bronchoscopy. Chest 123:941-949.
8. Maas, J., R.A. Verheij, P.P. Groenewegen, S. de Vries, and P. Tse, M., J.F.K. Ng, J.W.F. Chung, and T.K.S. Wong, 2002. The Effect of Visual Stimuli on Pain Threshold and Tolerance. Journal of Epidemiology and Community Health 60:587–592.
9. Suminski, R.R., W.S. Carlos Poston, R.L. Petosa, E. Stevens, and L.M. Katzenmoyer. 2005. Features of the Neighborhood Environment and Walking by U.S. Adults. Journal of Clinical Nursing 11:462-469.
10. Varni, J.W., M.A. Rapoff, S.A. Waldron, R.A. Gragg, B.H. Bernstein, M.D. Newcomb, and C.B. Lindsley. 1996. Development of the Waldron/Varni Pediatric Pain Coping Inventory. Pain 67:141-150.
11. Tilt, J.H., T.M. Unfried, and B. Roca. 2007. Using Objective and Subjective Measures of Neighborhood Greenness and Accessible Destinations for Understanding Walking Trips and BMI in Seattle, Washington. American Journal of Health Promotion 21, 4:371-379.
12. Sprenger, C., F. Eippert, J. Finsterbusch, U. Bingel, M. Rose, and C. Büchel. 2012. Attention Modulates Spinal Cord Responses to Pain. Current Biology 22, 11:1019-1022.
13. Kaplan, R., and S. Kaplan. 1983. Cognition and Environment: Functioning in an Uncertain World. New York, Praeger, 287 pp.
14. Sherman, S. A., J.W. Varni, R.S. Ulrich, and V.L. Malcarne. 2005. Post-Occupancy Evaluation of Healing Gardens in a Pediatric Cancer Center. Landscape and Urban Planning 73:167-183.
15. Pasha, S., and M.M. Shepley. 2013. Research Note: Physical Activity in Pediatric Healing Gardens. Landscape and Urban Planning 118:53-58.
16. Marcus, C.C., and N.A. Sachs. 2013. Therapeutic Landscapes: An Evidence-Based Approach to Designing Healing Gardens and Restorative Outdoor Spaces. John Wiley & Sons, 336 pp.
17. Ivarsson, C.T., and P. Grahn. 2012. Differently Designed Parts of a Garden Support Different Types of Recreational Walks: Evaluating a Healing Garden by Participatory Observation. Landscape Research 37, 5:519-537.
18. Cooper-Marcus, C., and M. Barnes. 1995. Gardens in Healthcare Facilities: Uses, Therapeutic Benefits, and Design Recommendations. Martinez, CA, The Center for Health Design, 610 pp.
19. Stigsdotter, U.K., A.M. Palsdottir, and A. Burls, et al. 2011. Nature-Based Therapeutic Interventions. In: K. Nilsson, M. Sangster, and C. Gallis, et al. (Eds.) Forests, Trees and Human Health. Springer, pp. 309-342.
20. Annerstedt, M., and P. Währborg. 2011. Nature-Assisted Therapy: Systematic Review of Controlled and Observational Studies. Scandinavian Journal of Public Health 39, 4:371-388.
21. Verra, M.L., F. Angst, and T. Beck, et al. 2012. Horticultural Therapy for Patients with Chronic Musculoskeletal Pain: Results of a Pilot Study. Alternative Therapies in Health and Medicine 18, 2:44-50.
22. Wichrowski, M., J. Whiteson, F. Hass, A. Mola and M.J. Rey. 2005. Effects of Horticultural Therapy on Mood and Heart Rate in Patients Participating in an Inpatient Cardiopulmonary Rehabilitation Program. Journal of Cardiopulmonary Rehabilitation and Prevention 25, 5:270-4.
23. Gonzalez, M.T., T. Hartig, G.G. Patil, E.W. Martinsen, and M. Kirkevold. 2011. A Prospective Study of Group Cohesiveness in Therapeutic Horticulture for Clinical Depression. International Journal of Mental Health Nursing 20, 2:119-129.
24. Taylor, A.F., F.E. Kuo, and W.C. Sullivan. 2001. Coping with ADD: The Surprising Connection to Green Play Settings. Environment and Behavior 33:54-77.
25. Kuo, F. E., and A.F. Taylor. 2004. A Potential Natural Treatment for Attention-Deficit/Hyperactivity Disorder: Evidence from a National Study. American Journal of Public Health 94:1580-6.
26. Faber Taylor, A., and F.E. Kuo. 2009. Children with Attention Deficits Concentrate Better After Walk in the Park. Journal of Attention Disorders 12, 5:402-09.
27. Josefsson, T., M. Lindwall, and T. Archer. 2013. Physical Exercise Intervention in Depressive Disorders: Meta-Analysis and Systematic Review. Scandinavian Journal of Medicine & Science in Sports 14, 3:340-347.
28. Coon, J.T., K. Boddy, K. Stein, R. Whear, J. Barton, and M.H. Depledge. 2011. Does Participating in Physical Activity in Outdoor Natural Environments Have a Greater Effect on Physical and Mental Wellbeing Than Physical Activity Indoors? A Systematic Review. Environmental Science & Technology45, 5:1761-772.
29. Blumenthal, J. A., M.A. Babyak, and K.A. Moore, et al. 1999. Effects of Exercise Training on Older Patients with Major Depression. Archives of Internal Medicine 159:2349-356.
30. Berman, M.G., E. Kross, and K.M. Krpan, et al. 2012. Interacting with Nature Improves Cognition and Affect for Individuals with Depression. Journal of Affective Disorders 140, 3:300-05.
31. Lewy, A.J., V.K. Bauer, and N.L. Cutler, et al. 1998. Morning vs. Evening Light Treatment of Patients with Winter Depression. Archives of General Psychiatry 55, 10:890-896.
32. Gonzalez, M.T. 2010. Therapeutic Horticulture in Clinical Depression: a Prospective Study of Active Components. Journal of Advanced Nursing 66, 9:2002-13.
33. Cimprich, B., and D.L. Ronis. 2003. An Environmental Intervention to Restore Attention in Women With Newly Diagnosed Breast Cancer. Cancer Nursing 26:284-293.
34. Unruh, A., and S. Hutchinson. 2011. Embedded Spirituality: Gardening in Daily Life and Stressful Life Experiences. Scandinavian Journal of Caring Sciences 25, 3:567-574.
35. Li, Q., K. Morimoto, and M. Kobayashi, et al. 2008. Visiting a Forest, But Not a City, Increases Human Natural Killer Activity and Expression of Anti-Cancer Proteins. International Journal Immunopathology Pharmacology 21:117-28.
36. Kam, M.C.Y., and A.M.H. Siu. 2010. Evaluation of a Horticultural Activity Programme for Persons with Psychiatric Illness. Hong Kong Journal of Occupational Therapy 20, 2:80-86
37. Talbot, J., D. Stern, J. Ross, and C. Gillen. 1976. Flowering Plants as a Therapeutic Environmental Agent in a Psychiatric Hospital. Hortscience 11:365-366.
38. Perrins-Margalis, N.M., J. Rugletic, N.M. Schepis, H. Stepanski, and M. Walsh. 2000. The Immediate Effects of a Group-Based Horticulture Experience on the Quality of Life of Persons with Chronic Mental Illness. Occupational Therapy in Mental Health 16, 1:15-32.
39. Keep, P., J. James, and M. Inman. 1980. Windows in the Intensive Therapy Unit. Anaesthesia 35:257-262.
40. Hurd, M.D., P. Martorell, A. Delavande, K.J. Mullen, and K.M. Langa. 2013. Monetary Costs of Dementia in the United States. The New England Journal of Medicine 368, 14:1326-34.
41. Mooney, P., and P.L. Nicell. 1992. The Importance of Exterior Environment for Alzheimer Residents: Effective Care and Risk Management. Healthcare Management Forum 5:23-29.
42. Rappe, E., and P. Topo. 2007. Contact with Outdoor Greenery Can Support Competence among People with Dementia. Journal of Housing for the Elderly 21:229-248.
43. Detweiler, M.B., P.F. Murphy, L.C. Myers, and K.Y. Kim. 2008. Does a Wander Garden Influence Inappropriate Behaviors In Dementia Residents? American Journal of Alzheimer’s Disease and Other Dementias 23:31-45.
44. Chalfont , G.E., and S. Rodiek. 2005. Building Edge: An Ecological Approach to Research and Design of Environments for People with Dementia. Alzheimer's Care Today 6:341-8.
45. Edwards, C.A., C. McDonnell, and H. Merl. 2012. An Evaluation of a Therapeutic Garden’s Influence on the Quality of Life of Aged Care Residents with Dementia. Dementia 12, 4:494-510.
46. Rauma, P. 2003. What Makes a Healing Garden? A Tour Of Three Facilities’ Gardens That Nurture Residents’ Well-Being. Nursing Homes 52:50-55.
47. Detweiler, M.B., P.F. Murphy, K.Y. Kim, L.C. Myers, & A. Ashiai. 2009. Scheduled Medications and Falls in Dementia Patients Utilizing A Wander Garden. American Journal of Alzheimer’s Disease and Other Dementias 24:322-332.
48. Rappe, E. 2005. The Influence of a Green Environment and Horticultural Activities on the Subjective Well-Being of the Elderly Living in Long Term Care. Publication No. 24. Finland, University of Helsinki, Department of Applied Biology.
49. Fabrigoule, C., L. Letenneur, and J.F. Dartigues, et al. 1995. Social and Leisure Activities and Risk of Dementia: A Prospective Longitudinal Study. Journal of the American Geriatrics Society 43, 5:485-490.
50. Simons, L.A., J. Simons, J. McCallum, and Y. Friedlander. 2006. Lifestyle Factors and Risk of Dementia: Dubbo Study of the Elderly. Medical Journal of Australia 184:68-70.
51. Zeisel, J., N.M. Silverstein, J. Hyde, S. Levkoff, M.P. Lawton, and W. Holmes. 2003. Environmental Correlates to Behavioral Health Outcomes in Alzheimer’s Special Care Units. The Gerontologist 43:697-711.
52. Zeisel, J. 2005. Environment, neuroscience and Alzheimer’s disease. Alzheimer’s Care Quarterly 6:273-279.
53. Center for Disease Control. 2012. Obesity Health Consequences. www.cdc.gov/nccdphp/dnpa/obesity/consequences.htm.
54. Center for Disease Control. 2001. Increasing Physical Activity: A Report on Recommendations of the Task Force on Community Preventive Services. www.cdc.gov/mmwr/preview/mmwrhtml/rr5018al.htm.
55. Kahn, E.B., L.T. Ramsey, and R.C. Brownson, et al. 2002. The Effectiveness of Interventions to Increase Physical Activity. American Journal of Preventive Medicine 22, 4S:87-88.
56. Pretty, J., J. Peacock, M. Sellens, and M. Griffin. 2005. The Mental and Physical Health Outcomes of Green Exercise. International Journal of Environmental Health Research 15:319-337.
57. Mackay, G.J., and J.T. Neill. 2010. The Effect of "Green Exercise" on State Anxiety and the Role of Exercise Duration, Intensity, and Greenness: A Quasi-Experimental Study. Psychology of Sport and Exercise 11:238-245.
58. Orsega-Smith, E., A.J. Mowen, L.L. Payne, and G. Godbey. 2004. The Interaction of Stress and Park Use on Psycho-Physiological Health in Older Adults. Journal of Leisure Research 36:232-257.
59. U.S. Department of Health & Human Services. 1996. Physical Activity and Health: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Atlanta, GA.
60. Hull, R.B., and S.E. Michael. 1995. Nature-Based Recreation, Mood Change, and Stress Restoration. Leisure Sciences 17:1-14.
61. Hartig, T., G.W. Evans, L.D. Jamner, D.S. Davis, and T. Gärling. 2003. Tracking Restoration in Natural and Urban Field Settings. Journal of Environmental Psychology 23:109-123.
62. Ulrich, R.S., R.F. Simons, B.D. Losito, E. Fiorito, M.A. Miles, and M. Zelson. 1991. Stress Recovery During Exposure to Natural and Urban Environments. Journal of Environmental Psychology 11:201-230.
63. Ulrich, R.S. 1981. Natural Versus Urban Scenes: Some Psychophysiological Effects. Environment and Behavior 13:523-556.
64. Nakamura, R., and E. Fujii. 1990. Studies of the Characteristics of the Electroencephalogram When Observing Potted Plants: Pelargonium Hortorum "Sprinter Red" and Begonia Evansiana. Technical Bulletin of the Faculty of Horticulture of Chiba University 43:177-183.
65. Nakamura, R., and E. Fujii. 1992. A Comparative Study of the Characteristics of the Electroencephalogram When Observing a Hedge and a Concrete Block Fence. Journal of the Japanese Institute of Landscape Architects 55:139-144.
66. Smith, V.D., and D.E. Aldous. 1994. Effect of Therapeutic Horticulture on the Self-Concept of the Mildly Intellectually Disabled Student. In: M. Francis, M., P. Lindsey, and J.C. Rice, (Eds.) The Healing Dimensions of People-Plant Relations. University of California, Davis, Center for Design Research.
67. Detweiler, M.B., T. Sharma, and J.G. Detweiler, et al. 2012. What Is the Evidence to Support the Use of Therapeutic Gardens for the Elderly? Psychiatry Investigation 9, 2:100-110.
68. Glerup, H., K. Mikkelsen L. Poulsen, E. Hass, S. Overbeck, J. Thomsen, P. Charles, and E.F. Eriksen. 2000. Commonly Recommended Daily Intake of Vitamin D is Not Sufficient if Sunlight Exposure is Limited. Journal of Internal Medicine 247, 2:260-268.
69. Gammack, J.K. 2008. Light Therapy for Insomnia in Older Adults. Clinics in Geriatric Medicine 24, 1:139-149.
70. Coupland, C.A., S.J. Cliffe, E.J. Bassey, M.J. Grainge, D.J. Hosking, and C.E. Chilvers. 1999. Habitual Physical Activity and Bone Mineral Density in Post-Menopausal Women in England. International Journal of Epidemiology 28:241-246.
71. Galloway, M.T. and P. Jokl. 2000. Aging Successfully: The Importance of Physical Activity in Maintaining Health and Function. Journal of the American Academy of Orthopaedic Surgeons 8:37-44.
72. Ottosson, J., and P. Grahn. 2008. The Role of Natural Settings in Crisis Rehabilitation: How Does the Level of Crisis Influence the Response to Experiences of Nature with Regard to Measures of Rehabilitation? Landscape Research 33, 1:51-70.
73. Hull, R.B. 1992. How the Public Values Urban Forests. Journal of Arboriculture 18, 2:98-101.
74. Kaplan, S., and C. Peterson. 1993. Health and Environment: A Psychological Analysis. Landscape and Urban Planning 26:17-23.
75. Helphand, K.I. 2006. Defiant Gardens: Making Gardens in Wartime. San Antonio, TX, Trinity University Press, 303 pp.
76. Vale, L.J., and T. J. Campanella (Eds). 2005. The Resilient City: How Modern Cities Recover from Disaster. Oxford University Press, USA.
77. Tidball, K.G., M. Krasny, E. Svendsen, L. Campbell, and K. Helphand. 2010. Stewardship, Learning, and Memory in Disaster Resilience. Environmental Education Research 16, 5-6:591-609.
78. Tidball, K.G., and M.E. Krasny. 2007. From Risk to Resilience: What Role for Community Greening and Civic Ecology in Cities? In A.E. Wals (Ed.) Social Learning Towards a More Sustainable World. Netherlands, Waageningen Academic Publishers.
79. Hodge, S. 2003. Research into Practice. Community Care 1503:45-48.
80. Duvall, J., and R. Kaplan. 2013. Exploring the Benefits of Outdoor Experiences on Veterans. Report Prepared for Sierra Club Military Families and Veterans Initiative. Report prepared for the Sierra Club Military Families and Veterans Initiative.
81. Gelkopf, M., I. Hasson-Ohayon, M, Bikman, and S. Kravetz. 2013. Nature Adventure Rehabilitation for Combat-Related Posttraumatic Chronic Stress Disorder: A Randomized Control Trial. Psychiatry Research 209:485-493.
82. Hyer, L., S. Boyd, R. Scurfield, D. Smith, and J. Burkel. 1996. Effects of Outward Bound Experience as an Adjunct to Inpatient PTSD Treatment of War Veterans. Journal of Clinical Psychology 52, 3:263-278.
83. Atkinson, J. 2009. An Evaluation of the Gardening Leave Project for Ex-Military Personnel with PTSD and Other Combat Related Mental Health Problems. Glasgow, The Pears Foundation.
84. Kaplan, R., and S. Kaplan. 1989. The Experience of Nature: A Psychological Perspective. New York, Cambridge University Press.
85. Rice, J.S., and L.L. Remy. 1998. Impact of Horticultural Therapy on Psychosocial Functioning Among Urban Jail Inmates. Journal of Offender Rehabilitation 26, 3-4:169-191.
86. Migura, M.M., L.A. Whittlesey and J.M. Zajicek. 1997.Effects of a Vocational Horticulture Program on the Self-Development of Female Inmates. HortTechnology 7, 3:299-304.
87. Jiler, J. 2009. Restoring Lives, Transforming Landscapes: The GreenHouse Program at Rikers Island Jail. In: L. Campell and A. Wiesen (Eds.) Restorative Commons: Creating Health and Well-Being Through Urban Landscapes. U.S. Department of Agriculture, Forest Service, Northern Research Station.
88. Nadkarni, N.M., and D.J. Pacholke. 2013. Bringing Sustainability and Science to the Incarderated. In: J. Appleton (Ed.) Values in Sustainable Development. London, Routledge, pp. 235-243.
89. Flagler, J. 1995. The Role of Horticulture in Training Correctional Youth. HortTechnology 5, 2:185-187.
90. McGuinn, C., and P.D. Relf. 2001. A Profile of Juvenile Offenders in a Vocational Horticulture Curriculum. HortTechnology 11, 3:427-433.
91. Sandel, M.H. 2004. Therapeutic Gardening in a Long-Term Detention Setting. Journal for Juvenile Justice Services 19, 1&2:123-131.
92. Lachowycz, K., and A.P. Jones. 2013. Towards a Better Understanding of the Relationship Between Greenspace and Health: Development of a Theoretical Framework. Landscape and Urban Planning 118: 62-69.
93. Barton, J., and J. Pretty. 2010. What is the Best Dose of Nature and Green Exercise for Improving Mental Health? A Multi-Study Analysis. Environmental Science and Technology 44, 10:3947-55.
94. Prescription Trails Program. 2011. New Mexico Health Care Takes on Diabetes Prescription Trails Fact Sheet. http://prescriptiontrails.org/about-us/2011factsheet_final.pdf
95. Institute at Golden Gate. 2013. Healthy Parks Healthy People. http://instituteatgoldengate.org/resources.
96. Walsh, J.M.E., D.M. Swangard, T. Davis, and S.J. McPhee. 1999. Exercise Counseling by Primary Care Physicians in the Era of Managed Care. American Journal of Preventive Medicine 16:307-313.
97. Martinson, B.C., A.L. Crain, N.P. Pronk, P.J. O'Connor, and M.V. Maciosek. 2003. Changes in Physical Activity and Short-Term Changes in Health Care Charges: A Prospective Cohort Study of Older Adults. Preventive Medicine 37:319-326.
98. SeeChangeHealth. 2013. CA/CO State Park Fee Reimbursement. SeeChange Health Blog, http://blogs.seechangehealth.com/partners/ca-parks.
99. Cohen-Mansfield, J., and P. Werner. 1998. Visits to an Outdoor Garden: Impact on Behavior and Mood of Nursing Home Residents Who Pace. In: B. Vellas, J. Fitten, and G. Frisoni (Eds.) Research and Practice in Alzheimer’s Disease. Paris, Serd, pp. 419-436.

a substantial amount of research shows that access to nature and gardens aids healing and recovery from a variety of physical and mental ailments
 hospital patients having plants in their room may display less fatigue and pain, shorter hospitalization, less anxiety, and higher hospital and room satisfaction
hospital patients having plants in their room may display less fatigue and pain, shorter hospitalization, less anxiety, and higher hospital and room satisfaction

 horticulture therapy has helped patients with chronic musculoskeletal pain to improve their mental and physical health, as well as help them to cope with chronic pain
horticulture therapy has helped patients with chronic musculoskeletal pain to improve their mental and physical health, as well as help them to cope with chronic pain
 gardening may help reduce the onset of dementia; gardening on a daily basis was found to reduce risk factors for dementia by 36%
gardening may help reduce the onset of dementia; gardening on a daily basis was found to reduce risk factors for dementia by 36%

 dementia patients having access to gardens show less aggression, fewer injuries, improved sleep patterns, and decreased agitation
dementia patients having access to gardens show less aggression, fewer injuries, improved sleep patterns, and decreased agitation
nearby nature can have positive effects on mental health, wellness, and can be applied in treatment or therapy
 children with Attention Deficit Disorder who played in grassy outdoor spaces had less severe symptoms than those playing in windowless indoor settings
children with Attention Deficit Disorder who played in grassy outdoor spaces had less severe symptoms than those playing in windowless indoor settings
 gardening activities or interacting with natural environments can reduce the mental fatigue of cancer treatment or surgery
gardening activities or interacting with natural environments can reduce the mental fatigue of cancer treatment or surgery
 depression patients who participated in routine gardening activities experienced a reduction in depression severity, and increased attentional capacity benefits lasting 3 months or more
depression patients who participated in routine gardening activities experienced a reduction in depression severity, and increased attentional capacity benefits lasting 3 months or more

it is estimated that there is a $2,200 reduction in average annual health care charges for an adult who has been sedentary, but then becomes more active; some studies suggest a connection between neighborhood open space and physical activity
 GreenHouse Program participants at Rikers Island Prison (New York) had a recidivism rate of 25%, compared to the overall rate of 65%
GreenHouse Program participants at Rikers Island Prison (New York) had a recidivism rate of 25%, compared to the overall rate of 65%