Epidemiology of Antimicrobial Resistant Gonococcal Infection (ARGC) in King County, Washington
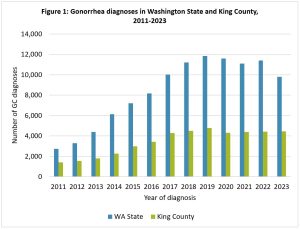
Figure 1: Gonorrhea diagnoses increased steadily in Washington State and in King County from 2011 to 2019. In 2020, the number of diagnosed cases decreased slightly, although it’s unclear whether this was due to a change in STD testing practices caused by the COVID-19 pandemic or a true decrease in incidence. There were 9,797 gonorrhea diagnoses in Washington State and 4,434 gonorrhea diagnoses in King County in 2023.
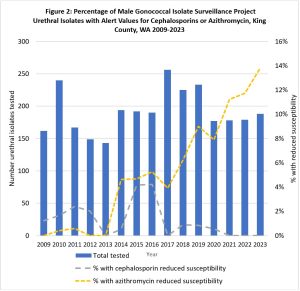
Figure 2: CDC’s Gonococcal Isolate Surveillance Project (GISP) monitors antimicrobial resistance in urethral gonococcal isolates from STD clinics around the U.S. In King County, azithromycin reduced susceptibility was low between 2009 and 2013 (0-1%), increased sharply in 2014 to 5%, then has increased steadily through 2023 to a high of 14%. Cephalosporin reduced susceptibility was low between 2009 and 2013 (0-1%), increased to 4% during 2015-2016, then decreased again during 2017-2023 (0-1%).
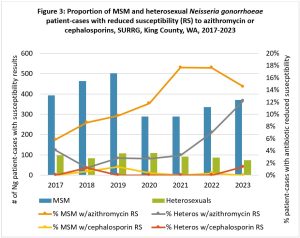
Figure 3: CDC’s Strengthening the U.S. Response to Resistant Gonorrhea (SURRG) monitors ARGC in patients of all genders with Neisseria gonorrhoeae (Ng) and at any infected anatomic site. Differences in ARGC are observed when comparing men who have sex with men (MSM) vs. heterosexual men and women. Reduced susceptibility to azithromycin steadily increased in MSM between 2017 and 2021, from 6% to 17%, and slightly decreased in 2023 to 15%. Reduced susceptibility to azithromycin in heterosexuals ranged from 1% to 4% through 2021, then increased through 2023 to 12%. Reduced susceptibility to cephalosporins (ceftriaxone and cefixime) has been low, 0-1% between 2017 and 2023, and has been detected in both MSM and heterosexuals.
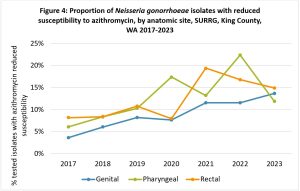
Figure 4: The proportion of gonococcal isolates with reduced susceptibility to azithromycin increased for all anatomic sites between 2017 and 2023. Genital isolates tended to have a lower prevalence of azithromycin reduced susceptibility compared to rectal and pharyngeal isolates except in 2023 (pharyngeal 12%, genital 14%, rectal 15%).
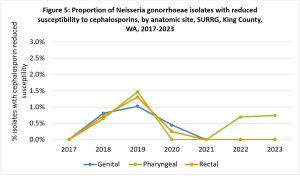
Figure 5: The proportion of gonococcal isolates with reduced susceptibility to cephalosporins (ceftriaxone and cefixime) increased among all anatomic sites from 2017 (0%) to 2019 (1.5% at the pharynx, 1.3% at the rectum, and 1.0% at the genitals) and decreased back to 0% in 2021. In 2022 and 2023, 0.7% of pharyngeal isolates had reduced susceptibility to cephalosporins, while genital and rectal isolates remained at 0%.
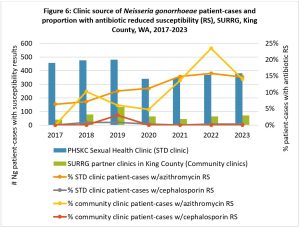
Figure 6: Public Health – Seattle & King County partners with several healthcare clinics in King County to collect gonococcal isolates from patients beyond the traditional STD clinic setting for monitoring ARGC. About 15% of SURRG patient-cases in King County were diagnosed at community clinics. Azithromycin reduced susceptibility increased in both STD clinic gonorrhea patient-cases (6-16%) and in community clinic patient-cases (0-23%) between 2017 and 2023. Although low, cephalosporin reduced susceptibility was identified in patients obtaining care both at the STD clinic (0-1%) and at community clinics (0-3%).