The majority of the focus of microbiological research in CF and other chronic lung infections has been on specific bacteria, such as Pseudomonas aeruginosa and Staphylococcus aureus. However, recent work by many laboratories reveals that many chronic lung infections are polymicrobial, involving very diverse collections of microbes infecting together. In CF, the use of culture-independent, next-generation sequencing methods shows that respiratory specimens for which cultures identify only one or two bacterial species can actually contain dozens of bacterial species. These results raise difficult questions about which of these organisms, if any, contributes to lung disease, and how these microbes respond to treatment with antibiotics and other medicines. Answering these questions may allow us to more rationally treat CF and other chronic infections.
We use next-generation sequencing methods to study the microbes infecting children with CF and other chronic lung infections. We recently showed that children with these diseases can have significant disease symptoms, and even advanced lung damage, despite having microbes very similar to those found in children with mild disease or even no lung disease, suggesting that the microbes were not responsible for initiating these diseases. Using these methods, we are studying how the microbes infecting children with chronic lung infections change as their disease progresses, and with treatments that improve their symptoms. In addition to suggesting better treatments, we use these data to inform our multispecies microbial models described in the previous web page on polymicrobial interactions.
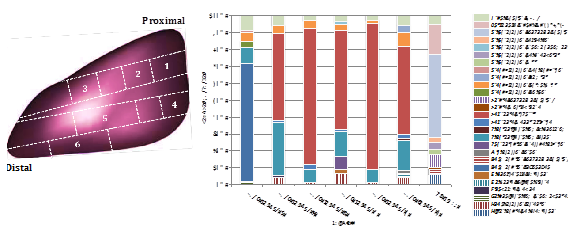
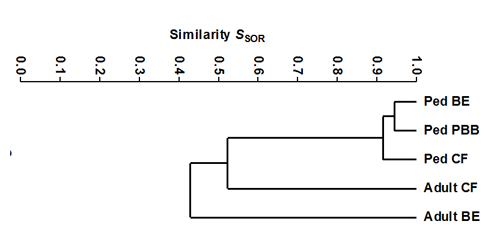
Figure legend: Top, sequencing-based microbiota analysis of samples from a diseased lung lobe from a young child with CF demonstrates anatomically heterogeneous, diverse microbiota that do not have abundant “traditional pathogens” and are poorly reflected by cultures (which yielded only S. aureus) or an oropharyngeal swab (right). Bottom, the most abundant and common microbiota from respiratory specimens from children with CF (Ped CF) are >90% similar to those from children with two other respiratory diseases—non-CF bronchiectasis (Ped BE) and protracted bacterial bronchitis (Ped PBB). However, adults with the two of these diseases that persist long-term—CF and BE—have respiratory sample microbiota that diverge from the childrens’ in disease-specific ways. It is not yet clear whether these changes are the cause of different disease outcomes, are caused by the different underlying diseases, or are driven by the different medicines these patients receive.


