While Pseudomonas aeruginosa has been relatively well-studied with respect to cystic fibrosis (CF) lung infection pathogenesis, the gram-positive bacterium Staphylococcus aureus has received relatively less attention, despite that fact that S. aureus is now the bacterium most commonly cultured from respiratory samples from all people with CF.
We found that slow-growing, antibiotic-resistant variants of S. aureus known as small-colony variants (SCVs) were very common among our local children with CF. Concerningly, detection of SCVs was associated with much worse lung disease outcomes compared with children who did not have SCVs detected. SCVs grow too slowly to be identified by most clinical laboratories, or to be tested for their responses to antibiotics using usual laboratory methods. Therefore, SCVs may be important CF pathogens that are rarely detected or reported, and little is known about how to treat them.
We are currently working to identify new laboratory methods for growing and testing S. aureus SCVs to improve detection and identify useful treatments. We are also working to understand the reasons why SCVs emerge over time among people with CF and many other chronic infections with S. aureus, including the selective forces within infected patients, as well as the molecular mechanisms of this adaptive change, in an effort to find ways to prevent their emergence.
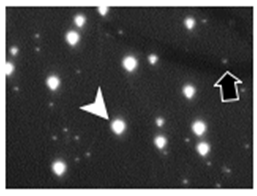
Figure legend: S. aureus small-colony variants (black arrow) compared with normal-colony, wild-type S. aureus (white arrow).


