| Research | ||||||||
|
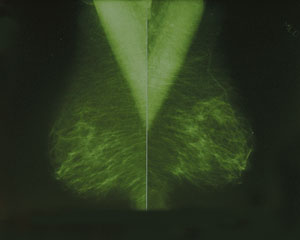
False-positive Mammograms Associated with Radiologist Inexperience |
||||||||
|
Mammograms may be the best tools for detecting breast cancer, but a UW study suggests a physician's experience interpreting results can affect a patient's treatment plan. In the Sept. 18, 2002 issue of the Journal of the National Cancer Institute, UW researchers reported that younger, more recently trained radiologists had two to four times the number of false-positive mammogram readings than radiologists who graduated more than 15 years prior to the study.
In 1998 Elmore and colleagues at the UW and Harvard University published a study in the New England Journal of Medicine reporting that at least one woman in two will receive a false-positive result after having annual screening mammograms for a decade, and almost 20 percent of women will undergo a biopsy. "If possible, women undergoing screening mammography should go to the same facility or ensure that prior films are available for comparison, because this can reduce unnecessary recalls," recommended Elmore. "Timing the mammography during the first and second week of a menstrual cycle may improve accuracy. Women taking hormone replacement therapy should be aware of possible increases in breast density that could reduce the accuracy of the mammography and result in the need for additional imaging or breast ultrasound. These women might want to reconsider the possible benefits of hormone replacement therapy in light of this and other possible risks." Elmore's editorial on steps women can take to obtain more accurate mammogram results is in the Journal of the National Cancer Institute, Vol. 95, 2003, pages 250-251. Development Note
Breast cancer in women and men is an area of intense focus for UW Medicine. The Breast Cancer Research Foundation has supported UW research projects for many years. Its contributions, along with those of other supporters, have funded studies on breast cancer vaccines, dose-density chemotherapy, cancer detection, and other aspects of breast cancer screening and treatment. |
||||||||
|
© 2003 - 2004 UW Medicine
Maintained by UW Health Sciences and Medical Affairs News and Community Relations Send questions and comments to drrpt@u.washington.edu |
||||||||