-
Home
We enhance prosthetics for people with limb loss through ground breaking research. Our philosophy is to be at the cutting edge of the interface between technology and clinical care. Though an academic research lab, we have a corporate culture of advancing quickly in our research and being highly productive in terms of immediately benefiting clinical care. Our research is centered around the improvement of care for transtibial amputees and designed to be immediately relevant to clinical practice. Our strong partnerships with prosthetists across the country ensures that we remain focused on the most pressing issues facing amputees. As a research lab within the University of Washington, education is at the core of what we do. The students and research engineers in our lab have diverse backgrounds, allowing students to gain a set of broadly applicable skills, while obtaining expertise in our core areas of research. 
-
Current Research
One of the biggest issues impacting limb health in transtibial amputees is the variability of fluid volume in their residual limb thoughout the course of the day. We are developing a socket whose volume can be adjusted, via a smartphone app, to ensure a proper fit. Prosethesis users frequently use socks, measured in "ply", to adjust the fit of their socket. Unfortunately, ply is not a well defined and so users cannot be sure how much they are adjusting their sockets. The problem is exacerbated when the sock is stretched over their limb. The CSG is means to measure the thickness of these socks while the user is wearing them. Bioimpedance has long been used to measure overall body composition. We are applying this technology to measure the fluid volume of amputees' residual limbs before and after their prosthetist does a modification on their socket. The goal is to help clinicians produce better outcomes and more quickly home in on the most beneficial modification. Determining the utility of new prosthetic practices and devices is a critical testing component. Initial tests conducted in a lab setting are useful, but they do not replace data collected from patients as they go about their daily routines. This work is intended to design tools to quantify changes in prosthetic fit and usage. Prosthetic liners are made out of a variety of polymers and even within liners from the same class of polymer there is substantial variation in material properties. Unfortunately, there has been no systematic survey done of these materials and clinicians have had to rely on anecdotal evidence for liner selection. We are creating a database of liner properties so that clinicians will have better information upon which to recommend liners to their patients. Prosthesis users can suffer skin damage from socket overuse or poorly fitting sockets. Skin can also adapt to become more resistant to mechanically-induced damage. Our goal in this research is to better understand the processes of skin breakdown and adaptation and to create tools to help clinicians better evaluate tissue health. 
-
Previous Research
-
Advancing Industry
-
Volunteer
-
Join Us
-
Contact Us
Current Research

Adjustable Sockets
- JE Sanders, TL Hartley, RH Phillips, MA Ciol, BJ Hafner, KJ Allyn, DS Harrison, "Does temporary socket removal affect residual limb fluid volume of trans-tibial amputees?", Prosthetics and Prosthetics International, vol. 40, no. 3, pp. 320-328, 2016
- JE Sanders, JC Cagle, KJ Allyn, DS Harrison, MC Ciol, "How do walking, standing, and resting influence transtibial amputee residual limb fluid volume?", Journal of Rehabilitation Research & Development, vol. 51, no. 2, pp. 201-212, 2014 PMID 24933719
- JE Sanders, "Commentary on Troedsson's 1964 Article "Stump Arterial Circulation at its Relationship to the Prescription of a Prosthesis for the Geriatric Patient"", Journal of Rehabilitation Research and Development, vol. 50, no. 5, pp. 9-9, 2013 PMID 26306335
- JE Sanders, JC Cagle, DS Harrison, KJ Allyn, "How does adding and removing liquid from socket bladders affect residual limb fluid volume?", Journal of Rehabilitation Research and Development, vol. 50, no. 6, pp. 845-860, 2013 PMID 24203546
- DL Swartzendruber, MT Redfield, JE Sanders, "A novel measurement device for volume management in lower limb amputees: A technical note", Medical Measurements and Applications Proceedings (MeMeA), 2013 IEEE International Symposium, 2013
- JE Sanders, KJ Allyn, DS Harrison, TR Myers, MA Ciol, EC Tsai, "Preliminary investigation of residual-limb fluid volume changes within one day", Journal of Rehabilitation Research and Development, vol. 49, no. 10, pp. 1467-1478, 2012 PMID 4423818
- JE Sanders, DS Harrison, JC Cagle TR Myers, MA Ciol, KJ Allyn, "Post-doffing residual limb fluid volume change in people with trans-tibial amputation", Prosthetics and Orthotics International, vol. 36, no. 4, pp. 443-449, 2012
- JE Sanders, DS Harrison, KJ Allyn, TR Myers, MA Ciol, EC Tsai, "How do sock ply changes affect residual limb fluid volume in people with trans-tibial amputation?", Journal of Rehabilitation Research and Development, vol. 49, no. 2, pp. 241-256, 2012 PMID 4431546
- JE Sanders, DS Harrison, TR Myers, KJ Allyn, "Effects of elevated vacuum on in-socket residual limb fluid volume: Case study results using bioimpedance analysis", Journal of Rehabilitation Research and Development, vol. 48, no. 10, pp. 1231-1248, 2011 PMID 4440224
- JE Sanders, S Fatone, "Residual limb volume change: Systematic review of measurement and management", Journal of Rehabilitation Research and Development, vol. 48, no. 8, pp. 949-986, 2011 PMID 4423813
- JE Sanders, DS Harrison, KJ Allyn, TR Meyers, "Clinical utility of in-socket residual limb volume change measurement: Case study results", Prosthetics and Orthotics International, vol. 33, no. 4, pp. 378-390, 2009 PMID 4435543
- JE Sanders, GS Lee, "A means to accommodate residual limb movement during optical scanning: A technical note", IEEE Transactions on Neural Systems and Rehabilitation Engineering, vol. 16, no. 5, pp. 505-509, 2008
- JE Sanders, EL Rogers, DC Abrahamson, "Assessment of residual-limb volume change using bioimpedence", Journal of Rehabilitation Research and Development, vol. 44, no. 4, pp. 525-535, 2007
- JE Sanders, EL Rogers, DC Abrahamson, "Assessment of residual-limb volume change using bioimpedence", Journal of Rehabilitation Research and Development, vol. 44, no. 4, pp. 525-536, 2007 PMID 18247249
- JE Sanders, A Karchin, JR Fergason, EA Sorenson, "A noncontact sensor for measurement of distal residual-limb position during walking", Journal of Rehabilitation Research and Development, vol. 43, no. 4, pp. 509-516, 2006 PMID 17123190
- JE Sanders, AK Jacobsen, R Fergason, "Effects of fluid insert volume changes on socket pressures and shear stresses: Case studies from two trans-tibial amputee subjects", Prosthetics and Orthotics International, vol. 30, no. 3, pp. 257-269, 2006
- JE Sanders, SG Zachariah, AK Jacobsen, JR Fergason, "Changes in interface pressures and shear stresses over time on trans-tibial amputee subjects ambulating with prosthetic limbs: comparison of diurnal and six-month differences", Journal of Biomechanics, vol. 38, no. 8, pp. 1566-1573, 2005
- JE Sanders, JR Fergason, SG Zachariah, AK Jacobsen, "Interface pressure and shear stress changes with amputee weight loss: case studies from two trans-tibial amputee subjects", Prosthetics and Orthotics International, vol. 26, no. 3, pp. 243-250, 2002
- R Saxena, SG Zachariah, JE Sanders, "Processing computer tomography bone data for prosthetic finite element modeling: A technical note", Journal of Rehabilitation Research and Development, vol. 39, no. 5, pp. 609-614, 2002 PMID 17642025
- JE Sanders, DW Cassisi, "Mechanical performance of inflatable inserts used in limb prosthetics", Journal of Rehabilitation Research and Development, vol. 38, no. 4, pp. 365-374, 2001 PMID 11563488
- SG Zachariah, JE Sanders, "Standing interface stresses as a predictor of walking interface stresses in the trans?tibial prosthesis", Prosthetics and Orthotics International, vol. 25, no. 1, 2001
- JE Sanders, SG Zachariah, AB Baker, JM Greve, C Clinton, "Effects of changes in cadence, prosthetic componentry, and time on interface pressures and shear stresses of three trans-tibial amputees", Clinical Biomechanics, vol. 15, no. 9, pp. 684-694, 2000
- SG Zachariah, JE Sanders, "Finite element estimates of interface stress in the trans-tibial prosthesis using gap elements are different from those using automated contact", Journal of Biomechanics, vol. 33, no. 7, pp. 895-899, 2000
- SG Zachariah, JE Sanders, "Pre-stresses due to trans-tibial socket donning: A nonlinear finite element analysis with contact", BMES/EMBS Conference, 1999, 1999
- JE Sanders, DM Bell, RM Okumura, AJ Dralle, "Effects of alignment changes on stance phase pressures and shear stresses on transtibial amputees: measurements from 13 transducer sites", IEEE Transactions on Rehabilitation Engineering, vol. 6, no. 1, pp. 21-31, 1998
- BJ Hafner, SG Zachariah, JE Sanders, "Automated alignment of contour pairs: A hybrid approach with applications to prosthetics", Proc. 1998 RESNA Annual Conference, pp. 283-285, 1998
- JE Sanders, D Lam, AJ Dralle, R Okumura, "Interface pressures and shear stresses at thirteen socket sites on two persons with transtibial amputation", Journal of Rehabilitation Research and Development, vol. 34, no. 1, pp. 19-43, 1997 PMID 9021623
- SG Zachariah, JE Sanders, "Finite Element Modeling of Contact Stresses Between the Below-Knee Residual Limb and Prosthetic Socket", ASME, 1997
- SG Zachariah, JE Sanders, "Interface mechanics in lower-limb external prosthetics: A review of finite element models", IEEE Transactions on Rehabilitation Engineering, vol. 4, no. 4, pp. 288-302, 1996
- SG Zachariah, JE Sanders, GM Turkiyyah, "Automated hexahedral mesh generation from biomedical image data: applications in limb prosthetics", IEEE Transactions on Rehabilitation Engineering, vol. 4, no. 2, pp. 91-102, 1996
- RE Schreiner, JE Sanders, "A silhouetting shape sensor for the residual limb of a below-knee amputee", IEEE Transactions on Rehabilitation Engineering, vol. 3, no. 3, pp. 242-253, 1995
- JE Sanders, LM Smith, FA Spelman, DJ Warren, "A portable measurement system for prosthetic triaxial force transducers", IEEE Transactions on Rehabilitation Engineering, vol. 3, no. 4, pp. 366-372, 1995
- JE Sanders, AJ Dralle, R Okumura, G Turkiyyah, HD Jang, D Lam, D Berglund, R Reed, G Hwaung, R Miller, " Interface Mechanics In Prosthetics: A System For Analysis", RESNA 95, pp. 242-244, 1995
- RE Schreiner, JE Sanders, "A geometric shape sensor for the residual limb of below-knee amputees", Engineering in Medicine and Biology Society, 1993. Proceedings of the 15th Annual International Conference of the IEEE, pp. 1290-1291, 1993
- LM Smith, JE Sanders, FA Spelman, "A portable signal conditioning and data acquisition system for prosthetic triaxial force transducers", Engineering in Medicine and Biology Society, 1993. Proceedings of the 15th Annual International Conference of the IEEE, 1993
- JE Sanders, CH Daly, "Normal and shear stresses on a residual limb in a prosthetic socket during ambulation: comparison of finite element results with experimental measurements", Journal of Rehabilitation Research and Development, vol. 30, no. 2, pp. 191-204, 1993 PMID 8035348
- JE Sanders, CH Daly, EM Burgess, "Interface shear stresses during ambulation with a below-knee prosthetic limb", Journal of Rehabilitation Research and Development, vol. 29, no. 4, pp. 1-8, 1992 PMID 4433005
- JE Sanders, DA Boone, CH Daly, "The residual limb/prosthetic socket interface normal stress and shear stress", Proceedings of the 13th Annual RESNA Conference, 1990
- JE Sanders, CH Daly, "Normal and shear interface stresses in lower-limb prosthetics", Engineering in Medicine and Biology Society, 1989. Proceedings of the 15th Annual International Conference of the IEEE, pp. 1443-1444, 1989
Funded by the Department of Defense.
The purpose of this project is to develop a prosthetic socket for trans-tibial prosthesis users that automatically adjusts its size so as to maintain prosthetic fit and minimize residual limb fluid volume loss.
The socket is potentially useful for active users who cannot be distracted to continually sense and adjust their socket size.
The objective is to allow prosthesis users to continuously wear their prosthesis pain-free and distraction-free and operate at high levels of function.
A first step in the development of the automatically adjusting socket was to make a socket where the volume could be controlled and monitored. We developed a motor-driven, cabled-panel, adjustable-socket system.
The motor is mounted beneath the socket and connects to the cable through tubes within the socket wall.
Upon commands from a micro-controller, the motor moves in discrete steps (in either direction), which causes the three socket panels (anterior lateral, anterior medial, posterior midline) to displace radially.
By keeping careful track of cable length, we are able to track socket volume changes induced by the radial movement of the panels.
The automatically-adjusting system operates using a collection of sensors in the prosthetic socket that monitors socket fit.
When an unfavorable change in fit is detected by the sensors, the system adjusts socket size accordingly until fit is once again favorable.
The sensors used are a collection of custom sensors developed in our lab.
To develop the automatic system, we created adjustable sockets for 12 participants and investigated how limb fluid volume changed when socket size was changed.
Results showed that, on average, users tolerated a socket size increase 2.2% larger than their normal socket volume and tolerated a socket size decrease 3.0% smaller than their normal socket volume.
User’s optimal size was, on average, 0.7% smaller in volume than their normal socket.
Fluid volume monitoring using bioimpedance analysis demonstrated that near the user’s optimal socket size, limb fluid volume changed in proportion to socket volume change.
At larger socket volumes, however, limb fluid volume did not further increase, and the socket became unstable and uncomfortable.

Diagnostic Tool
- JE Sanders, TL Hartley, RH Phillips, MA Ciol, BJ Hafner, KJ Allyn, DS Harrison, "Does temporary socket removal affect residual limb fluid volume of trans-tibial amputees?", Prosthetics and Prosthetics International, vol. 40, no. 3, pp. 320-328, 2016
- JE Sanders, JC Cagle, KJ Allyn, DS Harrison, MC Ciol, "How do walking, standing, and resting influence transtibial amputee residual limb fluid volume?", Journal of Rehabilitation Research & Development, vol. 51, no. 2, pp. 201-212, 2014 PMID 24933719
- JE Sanders, "Commentary on Troedsson's 1964 Article "Stump Arterial Circulation at its Relationship to the Prescription of a Prosthesis for the Geriatric Patient"", Journal of Rehabilitation Research and Development, vol. 50, no. 5, pp. 9-9, 2013 PMID 26306335
- JE Sanders, JC Cagle, DS Harrison, KJ Allyn, "How does adding and removing liquid from socket bladders affect residual limb fluid volume?", Journal of Rehabilitation Research and Development, vol. 50, no. 6, pp. 845-860, 2013 PMID 24203546
- DL Swartzendruber, MT Redfield, JE Sanders, "A novel measurement device for volume management in lower limb amputees: A technical note", Medical Measurements and Applications Proceedings (MeMeA), 2013 IEEE International Symposium, 2013
- JE Sanders, KJ Allyn, DS Harrison, TR Myers, MA Ciol, EC Tsai, "Preliminary investigation of residual-limb fluid volume changes within one day", Journal of Rehabilitation Research and Development, vol. 49, no. 10, pp. 1467-1478, 2012 PMID 4423818
- JE Sanders, DS Harrison, JC Cagle TR Myers, MA Ciol, KJ Allyn, "Post-doffing residual limb fluid volume change in people with trans-tibial amputation", Prosthetics and Orthotics International, vol. 36, no. 4, pp. 443-449, 2012
- JE Sanders, DS Harrison, KJ Allyn, TR Myers, MA Ciol, EC Tsai, "How do sock ply changes affect residual limb fluid volume in people with trans-tibial amputation?", Journal of Rehabilitation Research and Development, vol. 49, no. 2, pp. 241-256, 2012 PMID 4431546
- JE Sanders, DS Harrison, TR Myers, KJ Allyn, "Effects of elevated vacuum on in-socket residual limb fluid volume: Case study results using bioimpedance analysis", Journal of Rehabilitation Research and Development, vol. 48, no. 10, pp. 1231-1248, 2011 PMID 4440224
- JE Sanders, S Fatone, "Residual limb volume change: Systematic review of measurement and management", Journal of Rehabilitation Research and Development, vol. 48, no. 8, pp. 949-986, 2011 PMID 4423813
- JE Sanders, DS Harrison, KJ Allyn, TR Meyers, "Clinical utility of in-socket residual limb volume change measurement: Case study results", Prosthetics and Orthotics International, vol. 33, no. 4, pp. 378-390, 2009 PMID 4435543
- JE Sanders, GS Lee, "A means to accommodate residual limb movement during optical scanning: A technical note", IEEE Transactions on Neural Systems and Rehabilitation Engineering, vol. 16, no. 5, pp. 505-509, 2008
- JE Sanders, EL Rogers, DC Abrahamson, "Assessment of residual-limb volume change using bioimpedence", Journal of Rehabilitation Research and Development, vol. 44, no. 4, pp. 525-535, 2007
- JE Sanders, EL Rogers, DC Abrahamson, "Assessment of residual-limb volume change using bioimpedence", Journal of Rehabilitation Research and Development, vol. 44, no. 4, pp. 525-536, 2007 PMID 18247249
- JE Sanders, A Karchin, JR Fergason, EA Sorenson, "A noncontact sensor for measurement of distal residual-limb position during walking", Journal of Rehabilitation Research and Development, vol. 43, no. 4, pp. 509-516, 2006 PMID 17123190
- JE Sanders, DW Cassisi, "Mechanical performance of inflatable inserts used in limb prosthetics", Journal of Rehabilitation Research and Development, vol. 38, no. 4, pp. 365-374, 2001 PMID 11563488
- RE Schreiner, JE Sanders, "A silhouetting shape sensor for the residual limb of a below-knee amputee", IEEE Transactions on Rehabilitation Engineering, vol. 3, no. 3, pp. 242-253, 1995
- RE Schreiner, JE Sanders, "A geometric shape sensor for the residual limb of below-knee amputees", Engineering in Medicine and Biology Society, 1993. Proceedings of the 15th Annual International Conference of the IEEE, pp. 1290-1291, 1993
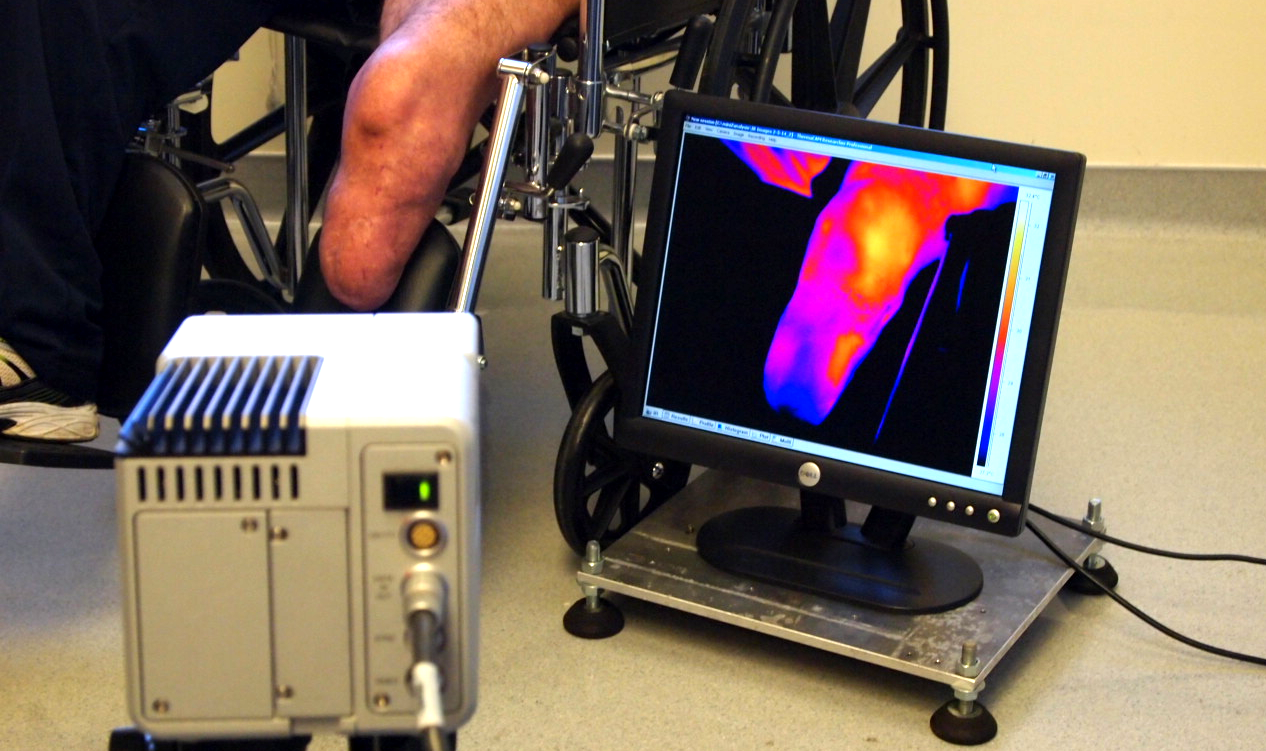
Changes in residual limb volume adversely affect the prosthetic fit of people with limb loss.
When volume change occurs, prosthetic fit can rapidly deteriorate from good to poor and put the user’s limb at risk of injury, precluding use of the prosthesis.
Though there are a variety of clinical techniques available to try to accommodate residual limb volume fluctuations, practitioners face difficulties selecting an appropriate accommodation strategy for an individual prosthesis user because residual limb volume change patterns are quite variable and can be difficult for some users to detect prior to the onset of limb health issues.
This study seeks to overcome this challenge in clinical care by presenting to the practitioner the fluid volume fluctuations their patient is experiencing, including where and when they occur and predicting how different accommodation treatments will affect each patient.
The objective is the translation of our portable bioimpedance analysis device created as part of a prior project into a meaningful and useful clinical diagnostic tool that facilitates diagnosis of limb fluid volume fluctuation and aids in selecting and fitting clinically-appropriate accommodation strategies to people with limb loss.
Our bioimpedance analysis device allows us to quantify extracellular and intracellular fluid within living tissue (i.e., a prosthesis user’s residual limb) while an individual is wearing their prosthetic socket (see Residual Limb Volume Fluctuation and Accommodation in the Previous Research tab).
We anticipate that the clinical research studies conducted here will provide key experience and knowledge towards a subsequent large-scale clinical trial.

Field Monitoring
- EC Swanson, JB McLean, KJ Allyn, CB Redd, JE Sanders, "Instrumented socket inserts for sensing interaction at the limb-socket interface", Medical Engineering & Physics, vol. 51, pp. 111-118, 2018
- DW Gardner, CB Redd, JC Cagle, BJ Hafner, JE Sanders, "Monitoring Prosthesis User Activity and Doffing Using an Activity Monitor and Proximity Sensors", Journal of Prosthetics and Orthotics, vol. 28, no. 2, pp. 68-77, 2016
- JE Sanders, JB McLean, JC Cagle, DW Gardener, KJ Allyn, "Technical note: Computer-manufactured inserts for prosthetic sockets", Medical Engineering and Physics, vol. 38, pp. 801-806, 2016
- BJ Hafner, JE Sanders, "Considerations for development of sensing and monitoring tools to facilitate treatment and care of persons with lower limb loss", Journal of Rehabilitation Research & Development, vol. 51, no. 1, pp. 1-14, 2014 PMID 4435686
- JE Sanders, MR Severance, D Swartzendruber, KJ Allyn, MA Ciol, "Influence of prior activity on residual limb volume and shape measured using plaster casting: results from individuals with trans-tibial limb loss", Journal of Rehabilitation Research and Development, vol. 50, no. 7, pp. 1007-1016, 2013 PMID 4435802
- MT Redfield, JC Cagle, BJ Hafner, JE Sanders, "Classifying Prosthetic Use via accelerometry in persons with trans-tibial amputations", Journal of Rehabilitation Research and Development, vol. 50, no. 9, pp. 1201-1212, 2013
- JE Sanders, MR Severance, KJ Allyn, "Computer-socket manufacturing error: How much before it is clinically apparent?", Journal of Rehabilitation Research and Development, vol. 49, no. 4, pp. 567-582, 2012 PMID 22773260
- JE Sanders, MR Severance, TR Myers MA Ciol, "Central fabrication: carved positive assessment", Prosthetics and Orthotics International, vol. 35, no. 1, pp. 81-89, 2011
- JE Sanders, MR Severance, "Measuring foam model shapes with a contact digitizer", Prosthetics and Orthotics International, vol. 35, no. 2, pp. 243-245, 2011
- JE Sanders, EL Rogers, EA Sorenson, GS Lee, DC Abrahamson, "CAD/CAM transtibial prosthetic sockets from central fabrication facilities: How accurate are they?", Journal of Rehabilitation Research and Development, vol. 44, no. 3, pp. 395-405, 2007 PMID 18247236
- JE Sanders, SB Mitchell, SG Zachariah, K Wu, "A digitizer with exceptional accuracy for use in prosthetics research: a technical note", Journal of Rehabilitation Research and Development, vol. 40, no. 2, pp. 191-196, 2003 PMID 15077643
- BJ Hafner, JE Sanders, JM Czerniecki, J Fergason, "Transtibial energy-storage-and-return prosthetic devices: A review of energy concepts and a proposed nomenclature", Journal of Rehabilitation Research and Development, vol. 39, no. 1, pp. 1-11, 2002 PMID 11926321
- JE Sanders, RA Miller, "A modular six-directional force sensor for prosthetice assessment: A technical note", Journal of Rehabilitation Research and Development, vol. 34, no. 2, pp. 195-203, 1997 PMID 9108346
- JE Sanders, RD Reed, RJ Marks, "Computer-aided prosthetic alignment for lower-limb amputees", Engineering in Medicine and Biology Society, Proceedings of the 15th Annual International Conference of the IEEE, pp. 1282-1283, 1993
- JE Sanders, CH Daly, DA Boone, TF Donaldson, "Technical note an angular alignment measurement device for prosthetic fitting", Prosthetics and Orthotics International, vol. 14, no. 1, pp. 143-144, 1990
We are developing a multitude of prosthetic monitoring devices that have a wide range of applications.
Our ultimate goal is to develop instrumentation to be worn on the prosthesis with little notice by the user that will provide practitioners with valuable insights, enabling them to provide better care to their patients.
Additionally, we develop devices for use as research tools, such as those that can be used to evaluate the effectiveness of different prosthetic components or new prosthetic technologies that we are developing.
In this work we develop devices to collect various biological signals of interest using sensors that we develop in our lab or existing sensors that we adapt for use in a prosthesis.
We also develop methods for automatically analyzing the collected data to extract important clinical insights and then to visualize the information in manner that is clinically relevant and easy to understand.
We have developed or are currently developing methods to monitor variables including: socket fit, limb movement, interface pressures, activity tracking, daily socket use, and patient behavioral compliance.

Optimizing Liner Selection
- JC Cagle, PG Reinhall, BJ Hafner, JE Sanders, "Development of Standardized Material Testing Protocols for Prosthetic Liners", Journal of Biomechanical Engineering, vol. 139, no. 4, pp. 1-12, 2017
- BJ Hafner, JC Cagle, KJ Allyn, JE Sanders, "Elastomeric Liners for People with Trantibial Amputation: Survey of Prosthetists' Clinical Practices", Prosthetics and Orthotics International, vol. 41, no. 2, pp. 149-156, 2016 PMID 27613589
- JE Sanders, BS Nicholson, SG Zachariah, DV Cassisi, AK Karchin, JR Fergason, "Testing of elastomeric liners used in limb prosthetics: classification of 15 products by mechanical performance", Journal of Rehabilitation Research and Development, vol. 41, no. 2, pp. 175-186, 2004 PMID 15558371
- JE Sanders, CH Daly, "How does vacuum forming affect Pelite mechanical properties?", Prosthetics and Orthotics International, vol. 18, pp. 43-48, 1994
A critical component in most prosthetic limb systems is the material used at the interface between the prosthetic socket and the residual limb.
This material acts as a cushion between the socket and the limb and often helps create a mechanical connection.
In lower-limb systems, this material comes in the form of an elastomeric prosthetic liner.
Selecting the appropriate liner is an important decision; however, prior to this project, information quantifying liner material properties was lacking.
The findings of this project are intended to enhance the practitioner's toolbox by providing information about how liners interact with residual limb soft tissues and how liners mechanically differ from one other.
This information should help practitioners select appropriate liners for their patients.
In this work, we have created a suite of standardized mechanical tests to be performed on prosthetic liners.
We have characterized several existing and emerging interface liner materials and have published our findings in a searchable tool on the website:
http://www.linerassist.org/.

Sock Thickness and Use
- JC Cagle, KJ D'Silva, BJ Hafner, DS Harrison, JE Sanders, "Amputee socks: Sock thickness changes with normal use", Prosthetics and Orthotics International, vol. 40, no. 3, pp. 329-335, 2016
- JC Cagle, AJ Yu, MA Ciol, JE Sanders, "Amputee socks: Thickness of multiple socks", Prosthetics and orthotics International, vol. 38, no. 5, pp. 405-412, 2014
- K D'Silva, BJ Hafner, KJ Ally, JE Sanders, "Self-reported prosthetic sock use among persons with transtibial amputation", Prosthetics and Orthotics International, vol. 38, no. 4, pp. 321-331, 2014
- JE Sanders, JC Cagle, DS Harrison, A Karchin, "Amputee socks: how does sock ply relate to sock thickness?", Prosthetics and Orthotics International, vol. 36, no. 1, pp. 77-86, 2012
Daily changes in the shape and size of the residual limb affect prosthetic socket fit. Prosthetic socks are often added or removed to manage changes in limb volume. The number and thickness of prosthetic socks required to maintain fit are highly variable. Manufacturers of prosthetic socks usually characterize the thickness of their products by a metric called sock “ply;” however, differences in materials, strain, and age of socks make the meaning of amputee sock ply confusing for both prosthesis users and prosthetists.
Using a custom research instrument, compressive stresses were applied to socks while sock thickness was measured, to reflect strain and loads experienced within the socket. We aimed to facilitate understanding of the meaning of sock ply towards clinical fit. An additional goal was to characterize how sock thickness changed under loading conditions experienced while a person with limb amputation walked in a prosthesis. Results from this investigation led us to propose a new nomenclature for sock thickness that may be more intuitive to practitioners and to the industry. We have also sought to better understand how persons with transtibial amputation use socks to manage diurnal changes in volume and comfort with a customized, self-report questionnaire. This work led to current projects involving the development of field monitoring devices to record sock changes and sock thickness during normal prosthesis use.
Adding and removing prosthetic socks is currently the most-used method for maintaining good socket fit when limb volume changes occur. Previous studies regarding sock thickness and sock use have shown that the volume accommodation provided cannot be reliably predicted by sock ply or age. Direct measurement of total sock thickness may provide more meaningful insight to quantify prosthetic users' socket fit and guide volume accommodation recommendations. We have developed a clinical tool for proper measurement of sock thickness in a clinical setting. We are designing it to be handheld and easy to use while providing accurate sock thickness measurements.
Tissue Health
- U Baran, EC Swanson, JE Sanders, RK Wang, "OCT-based microangiography for reactive hyperaemia assessment within residual limb skin of people with lower limb loss", Skin Research and Technology, vol. 24, no. 1, pp. 152-155, 2018
- YN Wang, J Sanders, "Chapter 15 - Skin Model Studies", Pressure Ulcer Research: Current and Future Perspectives; D. Bader, C. Bouten, D. Colin, C. Oomens Editors, pp. 263-285, 2005 PMID Springer
- MM Sullivan, TH Barker, SE Funk, A Karchin, NS Seo, M Hook, J Sanders, B Starcher, TN Wight, P Puolakkainen, EH Sage, "Matricellular Hevin Regulates Decorin Production and Collagen Assembly", The Journal of Biological Chemistry, vol. 281, no. 37, pp. 27621-27632, 2005
- YN Wang, JE Sanders, "How does skin adapt to repetitive mechanical stress to become load tolerant?", Medical hypotheses, vol. 61, no. 1, pp. 29-35, 2003
- JE Sanders, SB Mitchell, YN Wang, K Wu, "An explant model for the investigation of skin adaptation to mechanical stress", IEEE transactions on Biomedical Engineering, vol. 49, no. 12, pp. 1626-1631, 2002
- JE Sanders, BS Goldstein, "Collagen fibril diameters increase and fibril densities decrease in skin subjected to repetitive compressive and shear stresses", Journal of Biomechanics, vol. 34, pp. 1581-1587, 2001 PMID 11716860
- JE Sanders, "Thermal response of skin to cyclic pressure and pressure with shear: a technical note", Journal of Rehabilitation Research and Development, vol. 37, no. 5, pp. 511-515, 2000 PMID 11322149
- B Goldstein, J Sanders, "Skin Response to Repetitive Mechanical Stress: A New Experimental Model in Pig", Archives of Physical Medicine and Rehabilitation, vol. 79, pp. 265-272, 1998 PMID 9523777
- B Goldstein, JE Sanders, E Benson, "Pressure Ulcers in SCI: Does Tension Stimulate Would Healing?", American Journal of Physical Medicine & Rehabilitation, vol. 75, pp. 130-133, 1996 PMID 8630193
- JE Sanders, B Goldstein, "Skin Adaptation to Repetitive Mechanical Stress: Structural Remodeling and Bioprocess Changes", Whitaker International Program, 1996
- JE Sanders, BS Goldstein, DF Leotta, "Skin response to mechanical stress: adaptation rather than breakdown--a review of the literature", Journal of Rehabilitation and Research and Development, vol. 32, no. 3, pp. 214-227, 1995 PMID 8592293
- JE Sanders, RA Roy, BS Goldstein, "High-Frequency Acoustic Imaging for Early Detection of Skin Breakdown", ARPA/ONR Medical Ultrasonic Imaging Technology Workshop, 1995
- DF Leota, JE Sanders, "Non-invasive assessment of Structural Adaptation in Mechanically-Stressed Skin", Engineering in Medicine and Biology Society, 1993. Proceedings of the 15th Annual International Conference of the IEEE, vol. , no. , pp. 1286-1287, 1993
- DF Leotta, JE Sanders, "Non-Invasive Assessment of Structural Adaptation in Mechanically-Stressed Skin", IEEE Engineering in Medicine and Biology Conference, 1993
A common problem among prosthesis users is skin breakdown caused by the repetitive mechanical stresses acting on the limb within the prosthesis.
Skin breakdown (e.g. abrasions, skin tears, and pressure ulcers) can be painful and often results in decreased mobility for an individual.
Fortunately, skin is also able to adapt to mechanical stress to enhance the tissue’s ability to bear the stress without suffering breakdown.
The goal of this work is to develop techniques to prevent skin breakdown and to promote skin adaptation.
Previously we have investigated the phenomena of skin breakdown and adaptation through both animal and explant models, largely using histological techniques.
Currently we are developing non-invasive imaging techniques to investigate the physiology of skin breakdown and adaptation in humans and to predict skin breakdown before it is visibly evident.
Findings from this work could have broad-reaching applications from prosthetics to other areas where skin breakdown is a concern such as users of assistive devices and bedridden individuals.