-
Home
We enhance prosthetics for people with limb loss through ground breaking research. Our philosophy is to be at the cutting edge of the interface between technology and clinical care. Though an academic research lab, we have a corporate culture of advancing quickly in our research and being highly productive in terms of immediately benefiting clinical care. Our research is centered around the improvement of care for transtibial amputees and designed to be immediately relevant to clinical practice. Our strong partnerships with prosthetists across the country ensures that we remain focused on the most pressing issues facing amputees. As a research lab within the University of Washington, education is at the core of what we do. The students and research engineers in our lab have diverse backgrounds, allowing students to gain a set of broadly applicable skills, while obtaining expertise in our core areas of research. 
-
Current Research
One of the biggest issues impacting limb health in transtibial amputees is the variability of fluid volume in their residual limb thoughout the course of the day. We are developing a socket whose volume can be adjusted, via a smartphone app, to ensure a proper fit. Prosethesis users frequently use socks, measured in "ply", to adjust the fit of their socket. Unfortunately, ply is not a well defined and so users cannot be sure how much they are adjusting their sockets. The problem is exacerbated when the sock is stretched over their limb. The CSG is means to measure the thickness of these socks while the user is wearing them. Bioimpedance has long been used to measure overall body composition. We are applying this technology to measure the fluid volume of amputees' residual limbs before and after their prosthetist does a modification on their socket. The goal is to help clinicians produce better outcomes and more quickly home in on the most beneficial modification. Determining the utility of new prosthetic practices and devices is a critical testing component. Initial tests conducted in a lab setting are useful, but they do not replace data collected from patients as they go about their daily routines. This work is intended to design tools to quantify changes in prosthetic fit and usage. Prosthetic liners are made out of a variety of polymers and even within liners from the same class of polymer there is substantial variation in material properties. Unfortunately, there has been no systematic survey done of these materials and clinicians have had to rely on anecdotal evidence for liner selection. We are creating a database of liner properties so that clinicians will have better information upon which to recommend liners to their patients. Prosthesis users can suffer skin damage from socket overuse or poorly fitting sockets. Skin can also adapt to become more resistant to mechanically-induced damage. Our goal in this research is to better understand the processes of skin breakdown and adaptation and to create tools to help clinicians better evaluate tissue health. 
-
Previous Research
-
Advancing Industry
-
Volunteer
-
Join Us
-
Contact Us
Previous Research
|
Advancing Computer Manufactured Sockets
Biomaterials and Tissue Engineering
Interface Pressure and Shear Stress Management
Residual Limb Volume Fluctuation and Accommodation
Sock Thickness and Use
|
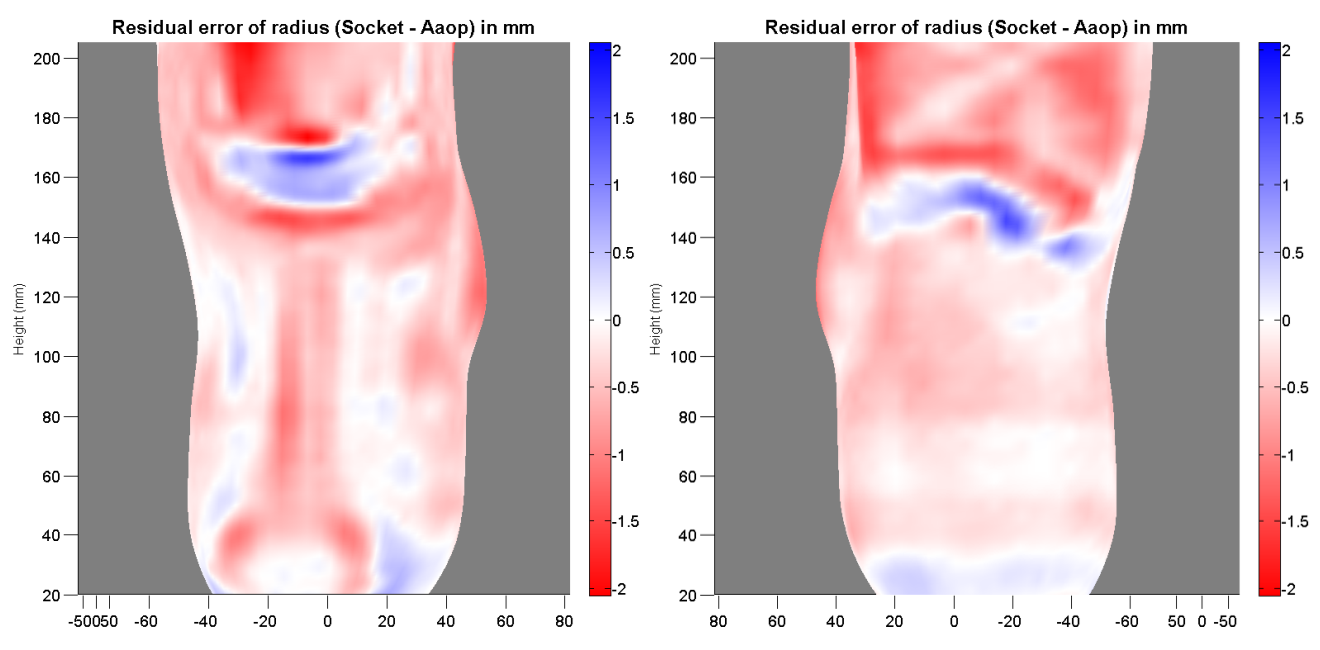
Advancing Computer Manufactured Sockets
The purpose of this project was to assess fabrication quality of computer-manufactured prosthetic sockets and positive models, and to determine socket size errors that negatively impact the health and quality of life of lower limb prosthesis users.
We found considerable variability in the quality of computer-manufactured sockets and models made by the central fabrication industry in prosthetics.
Some central fabrication facilities (~40%) consistently demonstrated very low manufacturing error while others were less consistent.
These findings led us to publish an evaluation strategy for central fabrication facilities to test their equipment.
The strategy may also be useful to companies who manufacture fabrication equipment as well as clinics who construct sockets in house.
We also investigated size and shaping error that caused clinically detectable changes in prosthetic fit. Our findings indicated that sockets oversized as little as 1.0% were clinically distinguishable from properly-sized sockets. Other studies indicated potential metrics for early detection of deterioration in socket fit that may be useful towards creating outcome assessment criteria for clinical care. Publications

Biomaterials and Tissue Engineering
In this work, we developed and tested novel materials for use in a variety of tissue engineering applications.
One area we focused on was improving the biocompatibility of implantable materials with the ultimate goal being long-term improvements in tissue health.
We focused on finely tuning the material properties of implants to more closely match those of the host tissue, more specifically by tuning fiber diameters in fibro-porous implants so that they were not encapsulated by host tissue.
We also focused on tissue engineering methods to enhance vascularity to promote blood flow through a porous implant material.
Enhancing blood flow through implantable materials is a key strategy to improve their integration into host tissue and to increase the likelihood of long-term tissue health.
Publications
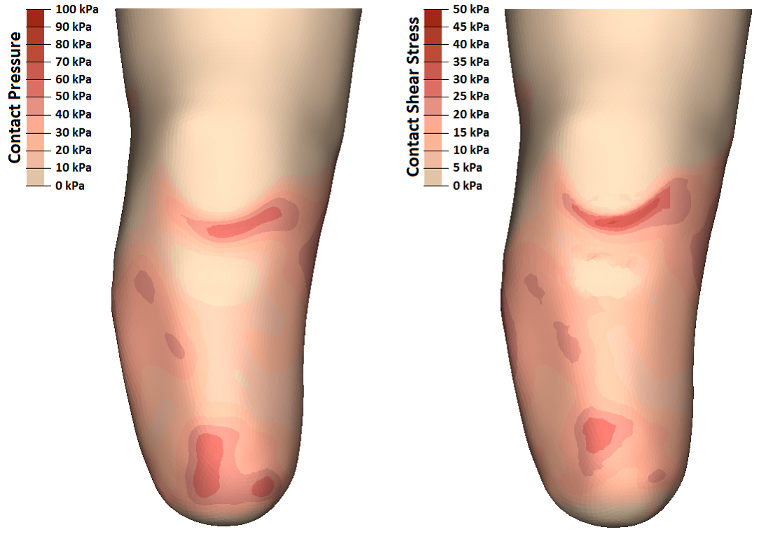
Interface Pressure and Shear Stress Management
In prosthetics, it is important to attain an appropriate distribution of pressure and shear stress at the limb-socket interface to maximize stability without overloading the soft tissues of the residual limb.
In the lower-limb prosthesis these mechanical stresses can be very large and potentially dangerous, as the soft tissues of the residual limb are often expected to bear multiple times full body weight such as during walking or jogging.
Obtaining reliable measurements of pressure and shear stress at the limb-socket interface is challenging due to space constraints and the need to leave the inside surface of the socket unaltered so as not to affect the distribution of pressure and shear. Prior to this project, knowledge of interface pressure and shear was limited by a lack of reliable measurements. In this work, we developed specialized transducers that were installed onto prosthetic sockets to measure both pressure and shear stresses at the socket wall. We performed a series of studies and obtained pressure and shear measurements at several locations on multiple study participants. This work has informed several of the other projects in our research group by providing a better understanding of the mechanical stresses that are to be expected at various locations within a prosthetic socket. Publications

Residual Limb Volume Fluctuation and Accommodation
We have developed a novel bioimpedance analysis instrument and use it regularly in studies to measure limb volume.
Thin electrodes are placed on the skin with very small wires exiting at the brim and extending to a data storage unit.
The instrumentation is worn by subject participants for many hours while they participate in a variety of activities.
The instrument has been used to better understand how design features of the prosthesis and the activity of a prosthesis user affect changes in size of a person's residual limb over the day.
Through various studies we have provided key insight to patients and practitioners treating volume management challenges.
We have also worked to develop novel volume management systems to overcome the detrimental effects of limb volume change on prosthetic fit and patient quality of life.
Publications

Sock Thickness and Use
Daily changes in the shape and size of the residual limb affect prosthetic socket fit. Prosthetic socks are often added or removed to manage changes in limb volume. The number and thickness of prosthetic socks required to maintain fit are highly variable. Manufacturers of prosthetic socks usually characterize the thickness of their products by a metric called sock “ply;” however, differences in materials, strain, and age of socks make the meaning of amputee sock ply confusing for both prosthesis users and prosthetists.
Using a custom research instrument, compressive stresses were applied to socks while sock thickness was measured, to reflect strain and loads experienced within the socket. We aimed to facilitate understanding of the meaning of sock ply towards clinical fit. An additional goal was to characterize how sock thickness changed under loading conditions experienced while a person with limb amputation walked in a prosthesis. Results from this investigation led us to propose a new nomenclature for sock thickness that may be more intuitive to practitioners and to the industry. We have also sought to better understand how persons with transtibial amputation use socks to manage diurnal changes in volume and comfort with a customized, self-report questionnaire. This work led to current projects involving the development of field monitoring devices to record sock changes and sock thickness during normal prosthesis use. Adding and removing prosthetic socks is currently the most-used method for maintaining good socket fit when limb volume changes occur. Previous studies regarding sock thickness and sock use have shown that the volume accommodation provided cannot be reliably predicted by sock ply or age. Direct measurement of total sock thickness may provide more meaningful insight to quantify prosthetic users' socket fit and guide volume accommodation recommendations. We have developed a clinical tool for proper measurement of sock thickness in a clinical setting. We are designing it to be handheld and easy to use while providing accurate sock thickness measurements. Publications
|