|
|
|
An Evolutionary War: Microbes and Immune System Disorders
|
|
 |
|
|
|
In the 20th century, improvements in hygiene and the introduction of immunizations and antibiotics gave humans an edge against microbes. This advantage has greatly reduced the prevalence of many infectious diseases. However, success may have its price. Researchers suspect the downside may be the growing incidence of immune system disorders, including certain autoimmune diseases.
The “Hygiene Hypothesis” suggests that the relative sterility of the developed world can, in genetically susceptible individuals, disturb the fine-tuning of their immune systems, which evolved over millennia to protect against a much dirtier environment.
Immune systems must strike a balance between protecting against infection, yet not reacting so strongly as to injure the body. Autoimmune disease happens when the system attacks the body’s own cells. At the UW, researchers investigate complex autoimmune disorders, specifically type 1 diabetes, multiple sclerosis, and lupus. They are seeking to discover the mechanisms that trigger the autoimmune response and to illuminate the complementary roles of genetic factors and environmental adaptations. Other work on the lifelong lung infection that kills cystic fibrosis patients has revealed that the condition worsens when the immune system reacts too aggressively to a microbial adaptation.
“We’ve changed the relationship between microbes and humans. Microbes have responded through rapid genetic adaptation,” said Dr. Chris Wilson, chair of immunology. “In this evolutionary war, the human immune system cannot adapt nearly as quickly.”
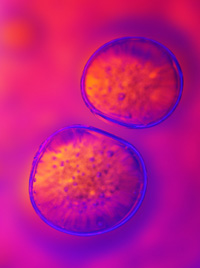
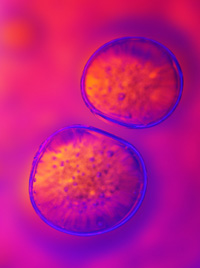
Research on type 1 diabetes in rats suggests a genetic basis for this autoimmune disease, in which T cells, the white blood cells that help fight off infection, attack the insulin-producing cells in the pancreas. Dr. Ake Lernmark, professor of medicine, has identified a gene, a mutation of which disrupts development of T cells. The mutation deletes a protein in the thymus, the gland where immature T cells develop and T cells that might harm the body are eliminated.
Multiple sclerosis, though not well understood, is thought to be an autoimmune disease that develops when T cells erroneously attack the myelin sheath surrounding nerve cells. Fluid taken from inflamed regions of the brains of multiple sclerosis patients contains two major types of T cells. Research on an animal disease similar to multiple sclerosis has focused on one type of T cell. However, another type of T cell is not activated in this model and its role has been mysterious. Dr. Joan Goverman, associate professor of immunology, has developed a promising animal model in which these myelin-specific T cells are also activated. The disease observed in this experimental model exhibits diverse pathology and a range of neurological signs consistent with the highly variable clinical signs of multiple sclerosis.
Researchers studying systemic lupus suspect that it may be related to imperfect clearance of dying cells by the immune system. Clearance of billions of such cells is an everyday bodily routine. Dr. Keith Elkon, professor of medicine, has established that this clearance is more efficient when the dying cells are coated with proteins from blood serum. Individuals with genetic deficiencies of these proteins are at risk for lupus. Another factor may be the release of cellular constituents, including DNA from dying cells. As a cell dies, this material undergoes biochemical changes. The immune system receptors that sense foreign pathogens fail to recognize the released cellular contents as the body’s own. This misidentification triggers an immune response.
Immunological research also suggests that, in the course of an infectious disease, a bacterial genetic adaptation may set off a damaging immune response. Pseudomonas aeruginosa is a deadly infectious agent in the lungs of patients with cystic fibrosis. A team led by Dr. Samuel Miller, professor of microbiology and of medicine, had earlier shown that Pseudomonas adapts to people with cystic fibrosis by changing the structure of a molecule in its membrane coat. A collaborative study by Miller’s team and a group led by Wilson found that certain immune system receptors recognize the molecular signature of this adaptation and trigger a more intense inflammatory response. In a healthy person, this would help eliminate the bacteria. In cystic fibrosis patients, the inflammation destroys the lungs.
“There’s a delicate immune system balance between reacting defensively to foreign pathogens and reacting too aggressively so as to endanger one’s own cells,” said Elkon, the lupus researcher. “It’s difficult for the system to maintain that balance while engaged in an arms race against microbes.”
|