Culture of Inquiry and Innovation
UWMC Professional Practice Structure | Our Shared Leadership

Relationship Based Care is our model of nursing. This model emphasizes the relationship with self, coworkers, and the patient/family, based on work by Mary Koloroutis, MSN, RN
Jump to section:
The Professional Practice Council (PPC), Local Practice Councils (LPCs) and Unit Practice Councils (UPCs) are the central structures by which nurses come together from within and across the medical center campuses to define and guide professional nursing practice. These councils are an example of shared leadership, where bedside nurses and leaders collaborate to improve care. The PPC reports to the Nursing Executive Council (NEC). Information flows between these levels of councils in both directions.
- UPC – Focuses on improvement projects for one unit.
- LPC – Focuses on improvement projects for a specialty area in nursing (ICU, Med-Surg, OR, etc.) and support the UPCs.
- PPC – House wide committee (both campuses) that oversees nursing policies and supports the councils. Made up of LPC co-chairs and more.
- NEC – Oversight council for nursing quality & practice with bedside RNs and nursing leaders.
Northwest campus LPCs
- Critical Care/ED
- Med-Surg
- Periop
- Procedural
- Infusion
- CBC
Montlake campus LPCs
- ICU
- Med-Surg
- Perianesthesia
- OR
- Procedural
- Oncology
- MIC
- NICU
Joint Councils
- Education
- Advanced Practice
- Clinical Informatics
- PPC
National Contributions to Research, Evidence-Based Practice and Sharing of Innovation
Nurses play a critical role in disseminating evidence, influencing national best practice guidelines, sharing innovation, and supporting and inspiring nurses across the country. The University of Washington Medical Center nurses make an incredible contribution on a national level in a multitude of ways. Some examples include:
Elizabeth Bridges, PhD, RN, CCNS, FCCM, FAAN
- National organization leadership position: Immediate Past-President of the American Association of Critical Care Nurses (AACN)
Nancy Colobong-Smith
- Author: Smith, N.C. (2022). An Innovative Approach to Integrating Nephrology Nursing into Acute and Critical Care. Nephrology Nursing Journal, 49(5) 397-403.
- Author: Jonsdottir, A.A., Lazo, G.R., Kessler, L.G., Smith, N.C., & Kim, J-E. (2022). Nephrology nurses’ perspectives for designs of mobile hemodialysis devices: A human factors engineering approach. Nephrology Nursing Journal, 49(6), 481-493.
- Book chapter author: Smith, N.C. (2022). Wearable Artificial Kidney. In S.M. Bodin (Ed.), Contemporary Nephrology Nursing. (4th ed., pp 1137-1149). Pitman, NJ: American Nephrology Nurses Association
- National organization leadership position: End Stage Renal Disease Network 16 Board of Directors, Chairperson (regional position – WA, OR, ID, MT, AK)
- National organization leadership position: American Nephrology Nurses Association, National President-Elect 2023-2024 Nephrology Nursing Journal Editorial Board
- National organization leadership position: End Stage Renal Disease Network 16 Medical Review Board
Cheri Constantino-Shor, MSN, RN, CRNI, CMSRN
- Author: Constantino-Shor, C. (2022). Authenticity is integral to effective leadership, Journal for Nurses in Professional Development, 38 (4), 231-32.
- Speaker: Infusion Nurses Society Annual Conference, Orlando, FLA, Keynote Address: Rebuilding Strong Healthcare Teams: Connecting as a Pathway Forward, June 2022
- Speaker: Emergency Nurses Association, WA Chapter, Seattle, WA, Keynote Address: Rebuilding Strong Teams: Shifting Away from the “I’m Fine” Culture in Healthcare, August 2022
Charity Holmes, RN, MSN, MBA, CNML, PMH-BC, NEA-BC
- National organization leadership position: President, Washington chapter of the American Psychiatric Nurses Association
Sydne Mead-Smith, MSN, RN, OCN
- Speaker: 47th Annual Oncology Nurses Society Congress, Anaheim, CA, Invited Panel Presenter: Deciphering the Specialty of Oncology Radiation, April, 2022
Tao Zheng, MN, RN, CCRN-CSC-CMC, CHFN, PCCN
- Speaker: University of Washington Continuing Nursing Education: Assessing Sleep in Patients with Cardiovascular Disease using Peripheral Arterial Tone Technology, October 2022
- Author: Zheng T. (2022). Sleep and heart failure: What do we know and what else do we need to know? American Association of Critical-Care Nurses Blog. Retrieved from: https://www.aacn.org/blog/sleep-and-heart-failure
- Award: Hester McLaws Dissertation Grant, University of Washington School of Nursing, 2022

Welle Rollout
We were excited to launch the new workplace violence prevention program called Welle in 2022. Welle is a program that supports assessment and de-escalation training for all patient-facing staff. Several hundred employees have successfully completed the training so far. It has been great to see our organization shift to a more trauma-informed, relationship-based care model that gives our staff practical skills to manage challenging situations and help decrease assaults. Our primary focus was getting staff in the high-risk (see below) tiers through first, then medium and finally low risk.
What are the tiers of training?
We divided the organization into three tiers of risk, High (ED, STAT/Resource, Public Safety, MSE, and APU), Medium (Acute care units), and Low (All other departments). This is based on potential risk for encountering challenging or violent behaviors.
How much training does everyone get?

Workplace safety is a top priority for UW Medical Center, and our Welle training program is a big part of that. We also had a thorough security assessment in 2022 by our public safety experts, and interventions in our environment and equipment were made based on that as well.
BERT
Workplace violence in our community and healthcare settings has been on the rise and continues to pose a significant occupational hazard to our staff, providers, and patients. As the climate of workplace safety changes, the standard for workplace violence prevention strategies must evolve with it. One of the multimodal solutions initiated by UWMC has included the Behavioral Emergency Response Team (BERT), a consult service modeled off the rapid response team to assist caregivers with proactively deescalating behaviors that could pose a safety risk to inpatient areas and the ED. The foundational principles of the BERT operate from a trauma-informed lens that centers addressing the patient’s individual needs, and ultimately developing therapeutic alliance through empowerment and skill development.
The team consists of one psychiatrically trained Registered Nurse from the Adult Psychiatric Unit, one STAT Registered Nurse, and one Public Safety Officer lead. Each responder team had received extensive training involving workplace violence prevention strategies, verbal de-escalation, BERT workflow, and “mock” BERT consults in which BERT responders could practice skills in real time through live simulation.
The BERT consult service has been live campus-wide at UWMC – Northwest since March 7, 2023, following a pilot period that occurred on the 5th floor between January 30th-March 6th, 2023. We are thrilled to have collected both anecdotal and statistical evidence of its success in supporting staff with identifying patient-centered solutions and preventing behavioral crises on medical units. Following the pilot period alone, the 5th floor saw a 22% decrease in SPM utilization, 66% decrease in WPV incidents, and 4.3% decrease in Code Gray events between January-March 2023, compared to January-March 2022 data. We have also received feedback from staff across the hospital that BERT has enhanced their sense of safety and support in their work setting, see below for more details.
We are excited to witness the long-term impacts of the BERT on workplace safety and an overall cultural change towards a trauma-informed, patient-centered approach when addressing the behavioral health needs of our patients.
Feedback from post-BERT response surveys:
- “[BERT] plan included validation of nursing tasks that were safe or unsafe given pt's AMS, delirium, dementia and assaultive behavior. Plan also included environmental modification, readjusting restraints for comfort and safety, and assisting primary RN to assess if other factors were contributing to agitation.”
- Special Care Unit RN - “It was very helpful having the psych RN here to help deescalate the situation with the patient.”
– Acute Care RN
CARE4U Wellbeing and Support Program
CARE4U Wellbeing and Support, has continued to grow through 2022. This program continues to strive to impact and inspire a robust culture of wellbeing at UWMC including: reducing the stigma of behavioral health and mental health impacts for allied health professionals, reducing barriers to access of support resources, offering a diverse menu of options for you, incorporating practical solutions and strategies that can be easily embedded into our workflows, and to adapt and stay flexible to meet you where you are and get the support and resources that you need - when you need them!
Here are some highlights from 2022:
Trauma Informed Workplaces
In 2022, UWMC and CARE4U began to embrace two foundational guiding frameworks more intentionally. The first is moving toward a truly Trauma Informed Workplace, from Substance Abuse and mental health Services Administration (SAMHSA). When a workplace is trauma informed, this means that the organization:
- Realizes the widespread impact of trauma and understands potential paths for recovery.
- Recognizes the signs and symptoms of trauma in patients, families, staff, and all other members of the system.
- Responds by fully integrating knowledge about trauma into policies, procedures, and practices and seeks to actively Resist Re-Traumatization
To do this, we are working to influence the prioritization of the Six Key Principles of a Trauma Informed Workplace:
- Safety: ensuring physical and emotional safety.
- Trustworthiness/Transparency: decisions are made with transparency with a goal of building and maintaining trust for all.
- Peer Support: Utilizing their stories and lived experience to promote healing.
- Collaboration/Mutuality: Everyone has a role to play in the healing process.
- Empowerment, Voice, & Choice: Individuals' strengths are recognized, built on, and validated.
- Cultural, Historical, and Gender Issues: Actively moving past stereotypes and biases, offering inclusive services.
Stress First Aid / National Center for Post Traumatic Stress Disorder
The second guiding foundational framework that we have adopted and began to implement into workflows in our hospitals and clinics is Stress First Aid from the National Center for PTSD.
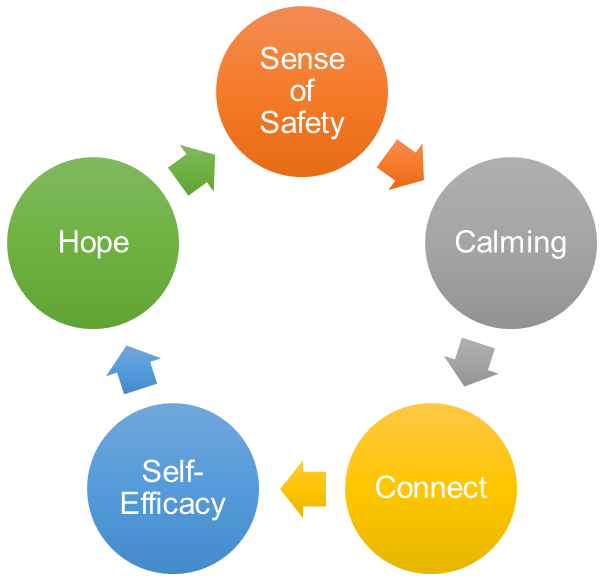
Stress First Aid (SFA) is a framework to improve recovery from stress reactions, both in oneself and in coworkers. The model aims to support and validate good friendship, mentorship and leadership actions through core actions that help to identify and address early signs of stress reactions in an ongoing way (not just after "critical incidents"). The goal of SFA is to identify stress reactions in self and others along a continuum and to help reduce the likelihood that stress outcomes develop into more severe or long-term problems.
Two of the main tools that you may have seen or be familiar with include the Five Factors that help us to move through stress and adversity, and The Stress Continuum Model.
Stop & Paws Staff Pet Therapy
The staff pet therapy program was expanded to include eight new pet therapy teams! With the support of these amazing volunteer teams and guides we were able to expand the program to reach both hospital sites and all shifts. The program was recently transitioned back into our Volunteer Services Program.
UW Medicine Peer to Peer Program
The UW Medicine Peer to Peer Program continues to see amazing utilization. Over 2022, we were able to support 267 referrals. The majority of these referrals consistently come from UWMC, which demonstrates a healthy culture of recognizing in ourselves or others a need for peer support and successfully linking to the program. Thank you for prioritizing self and mutual care at UWMC!
The top themes for peer support in 2022 were:
- Stress and Anxiety (27%)
- Death of a Patient (17%)
- Patient Adverse Event (17%)
- Emotional Distress (14%)
- Disruptive Patient or Family (12%)
- Burnout (10%)
Community of Support (Got Burnout? Sessions)
Community of Support or Got Burnout? sessions continue to be very popular and are now going on their 3rd consecutive year of sessions. These sessions continue to draw 20-60 people to each session and are a wonderful and caring space for everyone to touch in with each other – to get support for the hard things at work and in life, and to celebrate healing and other successes (even the little ones). We talk about preventing, managing, and recovering from the experience of burnout, but we also often dive into discussions about cognitive load, decision fatigue, self-compassion, empathy fatigue, acute and chronic stress, trauma exposures, conflict, transitioning into a new practice or specialty, world events that impact us, and much more.
Anyone is welcome to join and share or just listen – whatever feels good to you that day. We also end each session with exposure to a wellbeing practice, article, strategy, or intervention. We fully embrace that not one thing works for all of us and not one thing works for each situation, so we use this time to critically evaluate different evidence-based tools and talk about if they speak to us or not.
Looking Forward In 2023
- Implementation of a wellbeing grant program – Let us help fund the fantastic grass roots work you are doing in the wellbeing space!
- Launching “Get to Know CARE4U Sessions” – drop in informational and brainstorming sessions.
- Further embedding Peer Support referrals into high-risk workflows and experiences.
- Onboarding a new employee assistance program.
- Developing and implementing a formalized suicide prevention, intervention, and survivor support program for employees including launching a completely anonymous platform for proactive risk screening and connection to resources.
- Further development of a healthy debrief culture at UWMC including launching a Critical Incident Response Team and Group Debriefing process.
Tiered Skills Acquisition Model (TSAM)
Brittany Bergquist, MSN, RN and Kara Gardner, MN, RN, CMSRN – Nursing Professional Development


UW Medical Center is passionate about supporting RN preceptors and newly licensed nurses (NLN) during role transitions. In response to the national experience-complexity gap, UWMC started piloting the Tiered Skills Acquisition Model (TSAM) in 2022. TSAM is a competency-based model that offers a structured approach to unit orientation. Focused on the acquisition of skills, orientees assume more responsibility of their assignment with their preceptor by progressing through five defined tiers. The model increases new nurse competence, time management, and prioritization.
Originally created by the Mayo Clinic, TSAM was customized for UWMC in collaboration with preceptors, unit practice councils, committees, and leadership teams. Implementation of this model included preceptor training, creation of an online resource library, and partnership with leadership teams.
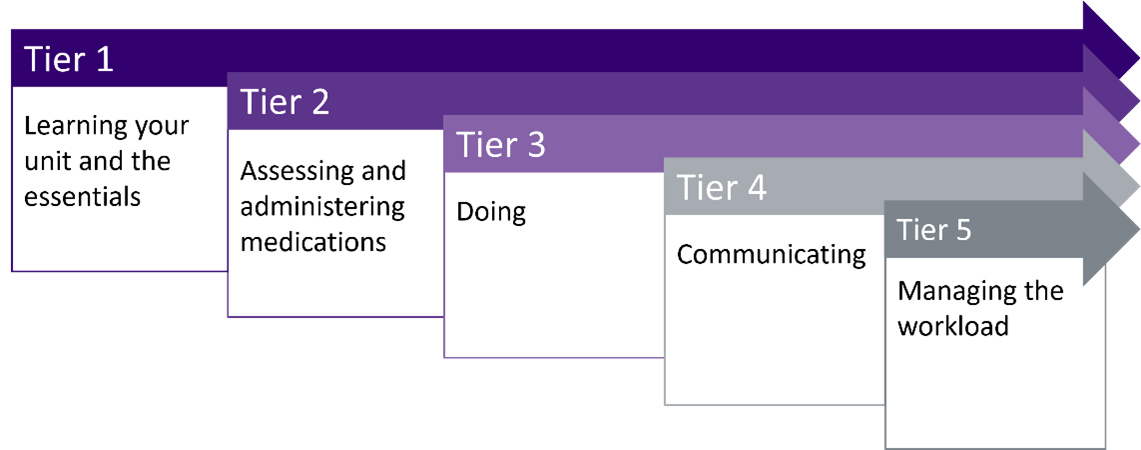
TSAM helps preceptors feel more supported, provided them with the knowledge and materials to precept, and clarified preceptor role expectations. Preceptors also felt their orientees were better prepared to transition into independent practice.
Here’s what preceptors are saying:
- “[TSAM] provides preceptors a tool to guide a preceptee’s journey and breaks down the teaching process into smaller bits.”
- “Orientees feel supported throughout the whole orientation”
NLNs report feeling less overwhelmed during orientation and better prepared to practice independently.
Supporting nursing staff is a top priority for UWMC and we are looking forward to bringing this model to more units next year.