Smoking has created a worldwide epidemic of death and disease.
- Smoking is the Number One cause of preventable death in the world. It currently causes about 8 million deaths per year (https://www.who.int/news-room/fact-sheets/detail/tobacco).
- The chemicals from cigarette smoke are inhaled into your lungs and do serious damage over time. They cause breathing problems, smoker’s cough, emphysema and lung cancer among many other illnesses.
- Cigarette smoke contains 250 cancer-causing chemicals, but there are 2 primary ones that do the most damage—tobacco-specific nitrosamines (TSNAs) and polycyclic aromatic hydrocarbons (PAHs). TSNAs are found in tobacco and are especially present in American produced tobacco leaves due to the curing process used in the US. PAHs are found in smoke generally (e.g, cigarette smoke, the charred parts of your steak, forest fires).
- Red blood cells get oxygen from the lungs and then distribute it throughout your body. When you inhale smoke, carbon monoxide (like car exhaust), TSNAs and PAHs are deposited on your red blood cells, too, and are then carried throughout your body. They thus affect not only your lungs, but your other organs, tissues and cells. This is why smokers are prone to various types of cancer—not just lung cancer.
Nicotine is addictive, but it won’t kill you.
- Nicotine is the primary drug in cigarettes that gets people hooked. It is highly addictive.
- Nicotine is like hopped up caffeine—it revs up the nervous system. Some people feel it helps them concentrate, gives them energy. But it’s also a more complex drug—it can work the opposite way to help people relax.
- Nicotine is not highly dangerous or deadly for adults. For most, it is relatively harmless outside of its addictive properties, so the gold standard treatment for smoking for years has been to replace the nicotine in cigarettes with safer forms of nicotine: nicotine lozenges, gums, patches, etc.
- Unlike with many drugs, you CANNOT overdose on nicotine as it is consumed in marketed products (cigarettes, ecigarettes, chew, snus, patches, gums). Withdrawal is not fun but it’s not life-threatening or physically harmful.
- In large amounts, however, nicotine can affect kids’ brains. It can rewire the brain and affect concentration and impulse control. It can lead to lifelong addiction to nicotine, which can lead to smoking unless they are using safer nicotine delivery systems. As far as drugs go, however, it’s not as risky for kids as most others out there.
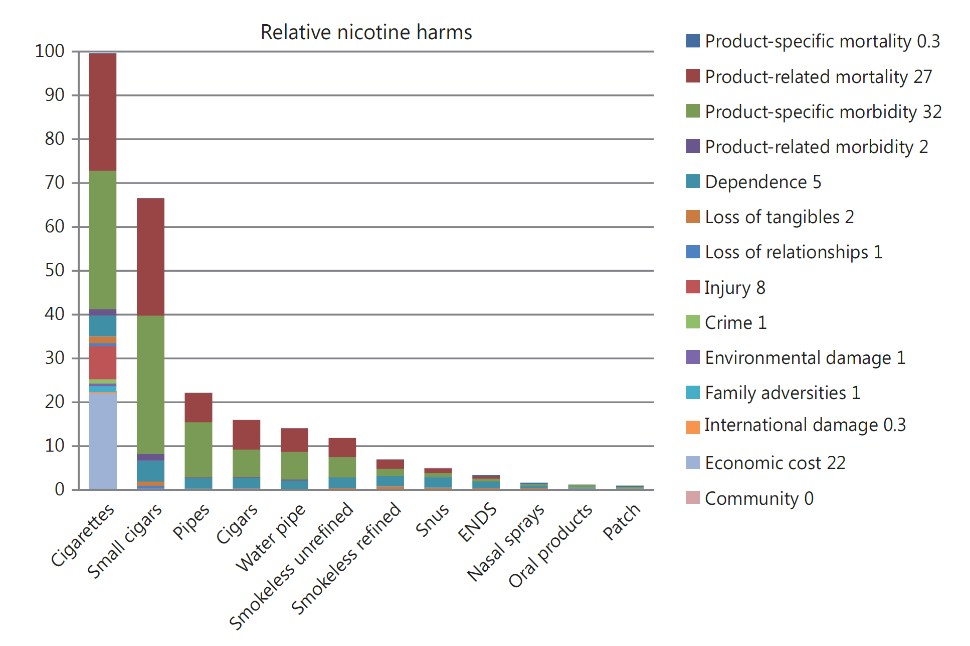
Getting nicotine in other ways than smoking reduces risk by at least 85%.1
- Again, the way adults typically use it, nicotine
is not highly dangerous in and of itself. So, getting nicotine in a safer way
than smoking will substantially reduce smoking related harm. One international study
found:
- Chewing tobacco is 85% safer than smoking.
- E-cigarettes/vapes, are 95% safer than smoking.
- Nicotine replacement therapy is 98% safer than smoking.
- So, while we want to prevent nicotine use among kids, e-cigs are a safer choice than smoking.
- The more factual information kids and the general public have about the relative risks of different drugs, the more they can make scientifically informed choices. We need to provide kids with the truth about nicotine, smoking and e-cigarettes. Otherwise, research has shown they will get and value more the information their peers give them.2
- We know information from peers is often inaccurate and thus potentially harmful, so we are best served combatting it through correct yet thoughtful information about health and safety.3
Completely switching to e-cigs is 95% safer than smoking and can promote harm-reduction among heavy smokers
- In their 2018 comprehensive, systematic review, the National Academies of Sciences, Engineering and Medicine concluded ecig use is safer than smoking.4 They even included a chapter on harm reduction involving e-cigarettes.
- The concentration of TSNAs is 97% lower in ecig users than smokers.5
- A study of smokers who switched to ecigs for 2 weeks showed toxin exposure was substantially reduced.6
- E-cigarette vapor does not contain the cancer-causing toxins in cigarette smoke that kill people (i.e., TSNAs or PAHs). Vaping does not entail other toxins that anyone can link to specific serious harm or health conditions.
- While we don’t know the long-term effects of vaping, the most cutting-edge science indicates that “the adoption of ENDs rather than cigarette smoking might result in an overall benefit for public health.”7
- Some smokers– esp those who are marginalized and from Communities of Color–often prefer e-cigs to other stop-smoking aids. This makes ecigs a more viable choice as a stop-smoking aid than nicotine replacement therapy or other pharmaceuticals for communities who have been most seriously impacted by the effects of smoking.8
How can we protect kids AND leverage e-cigarettes as a support to reduce harm in heavy smokers?
- We need to continue to do research on ecigs. We do not yet know the long-term health effects.
- We must warn the public to purchase ecigs from reputable sources only. The recent wave of lung disease in youth was caused by vaping cannabis that was illegally produced. It contained an additive that is not used in mainstream ecigs or vapes. It was NOT caused by mainstream vaping or ecig use (e.g., Juul).
- In the meantime, tightly regulating all nicotine products is key. This can be accomplished by setting a high legal age to purchase, regulating advertising and how it is pitched to youth, limiting venues where these can be purchased, having consequences for stores and individuals who make nicotine products available to minors.9,10
- The FDA’s plan is to start regulating the ecig industry, reduce nicotine content in cigarettes, which will essentially drive existing smokers to safer forms of nicotine use. And it will keep kids and others safer if there is better regulation of the purity of these products and laws against selling products to minors.
- Prohibition has—historically and notably– been associated with unintended negative consequences. In this case, banning industry-grade ecigs and flavoring means people obtain lower quality and illegally produced products or go back to smoking, which would undo positive strides we have made in keeping people—including kids—away from smoking. It could lead to the same kind of public-health-induced crisis we saw with opioids.
What are we doing to understand ecigarettes and health and safety in Seattle?
- Our long-standing science partnership between the University of Washington and Downtown Emergency Service Center (DESC) showed that providing health counseling, which included the above information paired with the provision of e-cigarettes, was an effective combination for heavy smokers experiencing homelessness, a very vulnerable, high-utilizing, high-cost, heavy-smoking population.8
- Participants rated the acceptability and effectiveness of this approach as “totally acceptable/effective” (10 out of 10 possible points).
- For each 1 week in the study, participants experienced an 18% increase in their odds of reporting 7-day, biochemically validated, point-prevalence smoking abstinence. The 6 participants who achieved abstinence reported using ENDS, not nicotine replacement therapy (even though we offered them NRT as well).
- Participants also showed reductions in self-reported cigarette dependence (-45%), smoking frequency (-29%), and smoking intensity (-78%; all ps<.05), the latter of which are associated with increased likelihood of future quit attempts.
- More important, participants who reported using ENDS during the study experienced a 44% reduction in smoking intensity and a 1.2-point reduction in dependence on cigarettes compared to participants who did not use ENDS.
- Our pilot findings echo the balance of the literature which has shown ENDS may help promote smoking reduction and cessation, even among smokers who do not intend to quit.4
- We are currently conducting a randomized controlled trial of this counseling + ecig approach compared to the current gold standard treatment for smoking in WA State (i.e., brief advice to quit + quitlilne referral). We plan to finish this study in 2021.
- We do not endorse or receive any funding from the ecigarette, tobacco or pharmaceutical industries.
References
1. Nutt DJ, Phillips LD, Balfour D, et al. Estimating the Harms of Nicotine-Containing Products Using the MCDA Approach. European Addiction Research. 2014;20(5):218-225.
2. Liu J, Zhao S, Chen X, Falk E, Albarracín D. The influence of peer behavior as a function of social and cultural closeness: A meta-analysis of normative influence on adolescent smoking initiation and continuation. Psychological Bulletin. 2017;143(10):1082-1115.
3. Romer D, Jamieson PE, Jamieson KH, Jones C, Sherr S. Counteracting the Influence of Peer Smoking on YouTube. J Health Commun. 2017;22(4):337-345.
4. National Academies of Sciences Engineering and Medicine. Public health consequences of e-cigarettes. Washington DC: The National Academies Press; 2018.
5. Shahab L, Goniewicz ML, Blount BC, et al. Nicotine, carcinogen, and toxin exposure in long-term e-cigarette and nicotine replacement therapy users: A cross-sectional study. Annals of Internal Medicine. 2017;166(6):390-400.
6. Goniewicz ML, Gawron M, Smith DM, Peng M, Jacob P, 3rd, Benowitz NL. Exposure to Nicotine and Selected Toxicants in Cigarette Smokers Who Switched to Electronic Cigarettes: A Longitudinal Within-Subjects Observational Study. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2017;19(2):160-167.
7. Benowitz NL, Fraiman JB. Cardiovascular effects of electronic cigarettes. Nature Reviews Cardiology. 2017;14:447.
8. Begh R, Lindson-Hawley N, Aveyard P. Does reduced smoking if you can’t stop make any difference? BMC Medicine. 2015;13:257.
9. Hardesty J, Awopegba A, Cohen J. Tobacco 21 Policy in Maryland: State of the Evidence. Available at: https://globaltobaccocontrol.org/resources/tobacco-21-reportsummary. 2019.
10. Stockings E, Hall WD, Lynskey M, et al. Prevention, early intervention, harm reduction, and treatment of substance use in young people. The Lancet Psychiatry. 2016;3(3):280-296.
Created by:
Susan E. Collins, PhD
Professor in the Department of Psychology at Washington State University
Affiliate Professor in the Department of Psychiatry and Behavioral Sciences at the University of Washington
Codirector of the Harm Reduction Research and Treatment (HaRRT) Center