April 2018 Spotlight-ED VTE Pathway

ED VTE Treatment & Disposition Pathway led by Dr. M. Kennedy Hall
The treatment of venous thromboembolism (VTE) in the emergency department is a prime example of the benefits of value-based care. A decade ago, the majority of pulmonary embolism (PE) and deep vein thrombosis (DVT) cases required admission for anticoagulation and bridging therapy with heparin. However, an emerging standard for outpatient management of DVT and low-risk PE could reduce admissions to 50% of newly diagnosed cases. Harborview Medical Center (HMC) and UW Medical Center each see approximately 800 cases a year. A CPI project, led by ER physician Kennedy Hall, sought to apply this approach within UW Medicine’s system.
“The opportunity for patients with pulmonary embolism to avoid admission will allow otherwise healthy patients to go about their lives with minimal interruptions.” — M. Kennedy Hall, MD MHS
Hall assembled a multi-disciplinary team (comprised of EM, inpatient IM, outpatient medicine, anticoagulation, pharmacy, IT, and nursing) to develop a new outpatient management approach to VTE. The team implemented this new pathway at HMC in March, which includes a sPESI (simplified pulmonary embolism severity index) and DVT assessment.
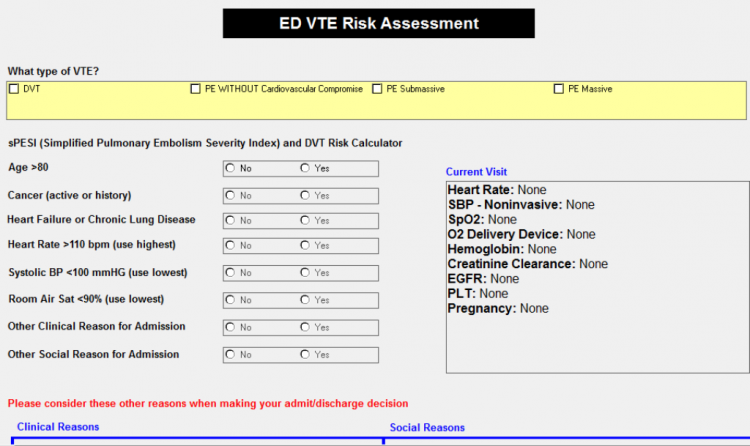
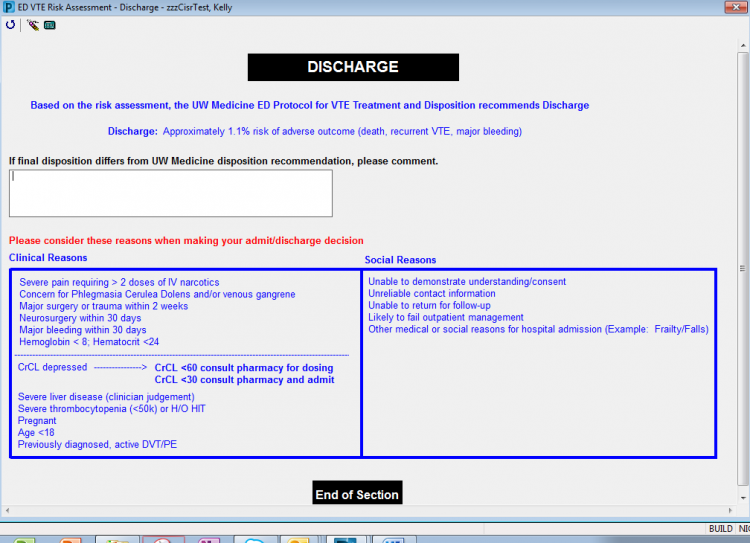
The pathway details explicit criteria, determined by a patient’s clinical and social situation, with electronic health record-based clinical decision support for patient disposition. This allows an improved ability to risk stratify: massive (causing circulatory shock), submassive (causing right ventricular failure), and small (radiographic only). The sPESI enables providers to interact with the tool and receive decision support at the time of care in the emergency department. Once all fields are populated, a recommendation for admission or discharge is displayed.
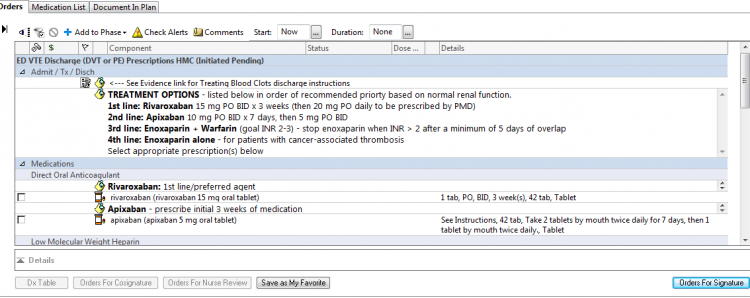
The pathway also includes a prescription PowerPlan, which assists providers in prescribing correct dosages of anticoagulation medications. Improvements in anticoagulation medications through DOACs confer multiple benefits: patients can now take a daily DOAC pill to thin the blood, preventing the need for monitoring of anticoagulation through painful blood testing. Another benefit of DOACs is that they may result in significantly fewer medication side effects from excessive unintended bleeding.
This approach to managing ED patients diagnosed with PE is complex and has not been without controversy. Even those physicians who have embraced outpatient management have been reticent to take this approach due to difficulties with risk stratification, lack of assurance of follow-up, challenges related to prescribing and obtaining the needed medications for these patients, and the extensive amount of time that this approach entails (a significant consideration in a busy ED).
“By collaborating with an inter-disciplinary team from pathway design to implementation, we were able to effectively engage stakeholders and troubleshoot perceived and real barriers to outpatient VTE management,” said Hall. “As highlighted by this CPI project, with system-wide partnerships, emergency medicine clinicians and their patients can benefit from building similar pathways for related conditions that traditionally required hospital admission.”
The inpatient hospital and pharmacy teams were also supportive. For example, at HMC, Pharmacy agreed on alternative payment models if a patient had no insurance. Valley Medical Center is also expected to go live with the pathway in April, with other entities following suit.
“The opportunity for patients with pulmonary embolism to avoid admission will allow otherwise healthy patients to go about their lives with minimal interruptions,” added Hall. “This approach also has considerable potential for high quality at lower cost, can help keep inpatients beds available for patients who need them most, and represents an excellent opportunity to provide value-based care.”