September 26, 2018
September 2018 Newsletter

Carlos A. Pellegrini, MD, FACS Chief Medical Officer, UW Medicine and Vice President for Medical Affairs
September is Sepsis Awareness Month and this issue of our newsletter focuses on some of the transformative and quality improvement work that’s been done to treat this life-threatening episode. It’s this type of critical care that is crucial for us to continue in our mission to improve the health of the public. Of course, we cannot even come close to achieving this mission if we are failing at getting patients into our system. Access shouldn’t be a barrier when patients are burdened by illness. But, as a system, we are not performing at our optimum best in this area, both in hospitalization and ambulatory settings. We need your help to fix this complex problem, so that we can get patients to see the right provider and receive appropriate care in a timely way. Follow standardized pathways and best practices. Proactively plan and schedule available hours. Participate in our service-by-service financial transformation process. Find out more about how you can help by watching this recent video discussion with Chief Health System Officer Lisa Brandenburg and me. Send any thoughts to uwmedway@uw.edu or projfit@uw.edu. Thanks for all you do for UW Medicine to help us fulfill our mission of improving the health of the public.
Code Sepsis: Systematic Response Saves Lives

More than 1.5 million people develop sepsis each year, making it one of the most common reasons for hospitalization. It’s also one of the most deadly — with 1 in 3 hospital deaths related to sepsis. With the introduction of CMS quality measures around sepsis in October 2015, there’s been increased effort to identify and rapidly treat sepsis. Sepsis is one area where standardization has been proven to be beneficial from the perspectives of mortality, length of stay and cost. Public reporting of hospital performance is set to begin this month (available on the Hospital Compare site).
All hospitals across the UW Medicine system have been working on improving the care of patients with sepsis. At Northwest Hospital, a Clinical Practice Innovator initiative, led by Laura Quinnan MD and Mary Jo Kelly MN ARNP-CNS, is starting to make a big difference in outcomes. Building on work by the NWH Sepsis Committee, this includes a “Code Sepsis” protocol with goals of early identification in the ED and ICU, antibiotics delivery within an hour of identification, alignment with ED anti-microbial order sets for in-patient, and decreased time to an ICU bed.
Use of flowsheets and nurse-initiated order sets (see below) was particularly key. “Improved nurse awareness of sepsis quality measures has a lot more people thinking about it,” said Quinnan. “Everyone is pleased this is being done.”

A video created by ED Operations Manager Liza Skelton and ED Director Christin Gordanier helps nurses evaluate vital signs and get labs and IVs started immediately while alerting the doctor. This work bridged the transition to the ICU and integrated other members across the care team, including phlebotomists, ICU charge, pharmacy and hospitalists.
The team is currently working on data collection for outcomes like mortality and length of stay, but there have been great improvements in process measures – from levels as low as 50% to all-time high of 88% in March.
According to Kelly, “Nurses providing feedback on use of the checklist has been critical to our success.” Future plans are to roll out the protocol to Acute Care early next year.
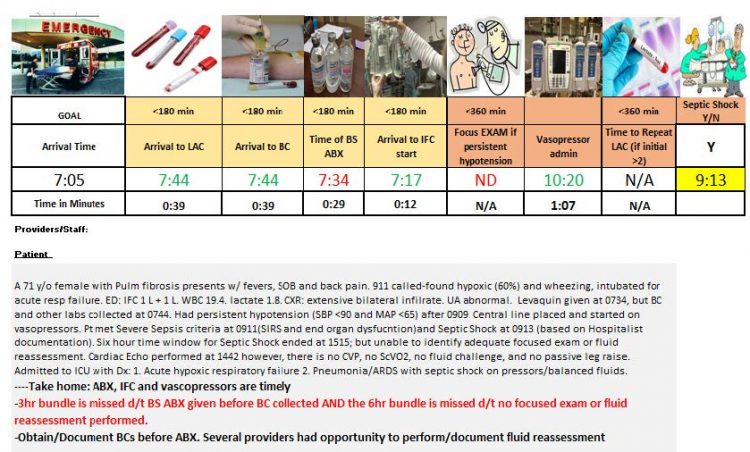
Valley Medical Center has also been achieving improved rates of sepsis QI measures that are above the national average. ED Director Cameron Buck, MD and Sepsis PI Team Champion/QI Specialist Jennifer Carney, MSN RN, developed performance feedback which reflects adherence to sepsis bundles via a pictogram (see below). This analytical tool helps communicate successes and improvement opportunities to the entire care team. Additionally, the CNS/educators provide “at-the-elbow” support through rounding and real-time coaching in early recognition and intervention. The CNS’ also provide formal communication and staff education.
Over at Harborview, Sepsis Medical Director David Carlbom, MD and Sepsis Coordinator Rosemary Grant BSN RN CPHQ, led a team that went through an intensive Rapid Improvement Process Workshop in 2016. The multidisciplinary group built on the existing sepsis screening system that had been in place at the hospital since 2011. This system showed more rapid delivery in acute care and a decrease in O/E mortality from 1.24 in 2011 to .95 in 2015, but was felt to be too sensitive in identifying sepsis patients — leading to alert fatigue and user dissatisfaction. Through an automated screening algorithm, nurse triage, standardized provider responses, and the creation of a Sepsis Order Set (SOS), improvements were made to workflow and downstream communications, leading to faster delivery of sepsis care and reduced mortality. Continued enhancements will work to further improve timely antibiotic delivery in the acute care setting and the creation of a screening system to be piloted in the MCICU in September, with roll out to other ICUs in 2019.
At UWMC, the multidisciplinary sepsis committee led by Rags Durvasula, MD MHA and Greta Anaman, MS RN CCRN, along with new PMO Director Esmeralda Pulido, MPH, have been working on iterations put into place after consultation with Vizient last year to develop a process improvement project plan. From this collaboration, UWMC launched a streamlined sepsis PowerPlan for improved safety and compliance with CMS guidelines, initiated an inpatient nursing sepsis alert system for medicine, cardiac and oncology units, and created dashboards using an innovative “time zero” methodology. Focus this year will include efforts to increase utilization based on provider feedback and boosting the inpatient response structure. Sepsis remains a major priority at UWMC and has been incorporated into three top 2018 Leader Evaluation Manager goals, including time to antibiotics in the ED, nurse response to alerts and reducing O/E mortality.
Briefly
- Improving care in the transition from inpatient to post-acute care (PAC) has been a joint initiative between the Chief Medical Officer and Chief Health System Officer’s office over the past two years. The cross-functional workteam has also strived to further evolve communication during these transitions of care to reduce the risk of post- hospital discharge adverse events and potentially preventable readmissions to the hospital. A Discharge Documentation Improvement Workgroup was tasked with identifying and addressing the existing gaps in discharge communication, including the discharge summary. Through literature reviews, stakeholder interviews, focus groups and surveys, an updated discharge summary template was developed, which includes formatting updates and additional sections to highlight care coordination. It also features improved functionality, including pulling in existing documentation from other tools/areas of the chart, such as Discharge Readiness and CORES. The new discharge summary template is scheduled to be released in late October 2018. For questions, please contact UWM Post-Acute Care at hmtran@uw.edu.