August 9, 2018
August 2018 Newsletter

Carlos A. Pellegrini, MD, FACS Chief Medical Officer, UW Medicine and Vice President for Medical Affairs
As we begin the new fiscal year, I wanted to take this opportunity to look forward to our goals in FY19 and to also recognize the great work you all helped accomplish last year. Dr. Paul Ramsey, CEO of UW Medicine, has identified two key FY19 priorities: our Financial Improvement Transformation (FIT) and Healthcare Equity. Our work in population health management, particularly at the primary care level, is integral to these goals in order to deliver the best care to all our populations of patients, while reducing disparities. Thanks to your work and leadership, we’ve made significant improvements — from Annual Wellness Visits to launching pathways for hypertension, depression and colorectal screening — and payers are taking notice. Through more accurately capturing risk scores, and bettering the cost and quality of care, UW Medicine is viewed as a high-performing health care system — resulting in more satisfied patients, better contracts and bonus payments. Moving forward this year, we’ll be expanding in new areas of transitional care management (TCM) and chronic care management (CCM) and have brought on an Associate Medical Director for Population Health, Leah Marcotte, MD, to help us in these efforts. Previously with Iora Health, Leah brings expertise on the team-based model approach to improving health of populations. This month, we’re highlighting a new care transformation pilot that further expands this breadth of care and helping keep chronic conditions at bay. Keep up the good work and thanks for all you do for UW Medicine to help us fulfill our mission of improving the health of the public.
Exercise is Medicine — Focusing on “Healthy” Care at UW Medicine

Did you know that physical inactivity is the 4th-leading risk factor for death worldwide? It’s also a major risk factor for cardiovascular disease, stroke, type 2 diabetes, cancers, obesity, and depression, according to the World Health Organization. Unfortunately, exercise is under-discussed and under-prescribed by healthcare professionals. According to the American Heart Association (2016 scientific statement ), aerobic fitness should be considered a vital sign — just as important as body temperature, blood pressure, pulse and breathing rates.
That concept was formalized as a global initiative – Exercise is Medicine (EIM) — in 2007 by the American Medical Association (AMA) and the American College of Sports Medicine (ACSM). EIM now has national task groups in more than 40 countries with a goal to institutionalize physical activity assessment and prescription in healthcare systems.
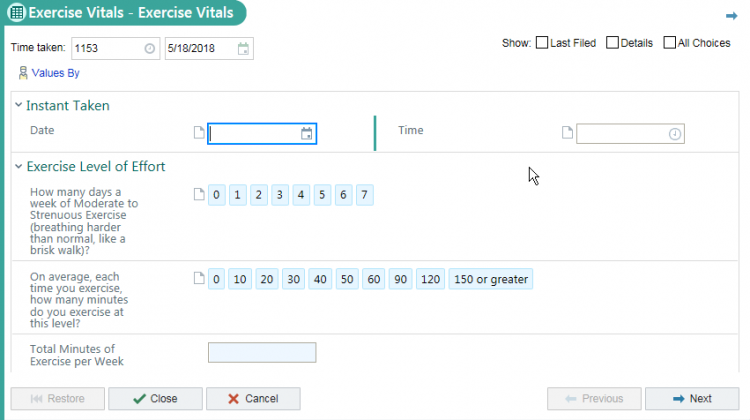
UW Medicine is one of those systems taking up the charge toward integrating exercise as a vital sign (EVS) and exercise prescription in clinical practice. Led by Cindy Lin MD, a standardized and simple two question “exercise as vital sign” screener was integrated in the EPIC electronic medical record. Using the smartphrase .EXERCISEVITALS pulls the minutes per week of exercise into the clinic note (see below).
Sports & Spine practices at UW Eastside Specialty Center, Stadium Sports Medicine Center, and HMC, are now participating, with medical assistants asking these questions as part of the typical blood pressure, heart rate, and vital sign intake. In 2017, the EVS was recorded in more than 8,000 Sports & Spine patient visits.
“With UW Medicine’s focus on population health and healthy care, asking about EVS with these two simple questions – which takes around ten seconds – is a great opportunity to engage the patient in conversation about their lifestyle,” said Lin. “Physical activity and fitness is a major health risk factor that we in healthcare can help patients to change.”
In 2018, the EVS was expanded to Northgate Family Medicine Clinic and HMC Rehabilitation Medicine Clinic. While a cultural shift, clinics are finding the pilot program easy to implement. “The initial pilot has been smooth and well-received by patients and staff without any notable interruption in workflow, which is highly important in this very busy primary care clinic,” said Nicole Gentile MD PhD, resident physician in family medicine leading the pilot at UW Neighborhood Clinic-Northgate.
Based on the EVS, providers can then discuss the importance of exercise with their patients and recommend appropriate community-based or online exercise resources. Next steps are to develop more exercise prescription referral resources and expand the EVS to more clinical settings. This is a great example of UW Medicine expanding its focus from “sick” care to “healthy” care — a move totally aligned to our mission.